More than half of all people with asthma have a form that’s triggered by everyday allergens-things like pollen, dust mites, or pet dander. This is called allergic asthma. It’s not just about sneezing or a runny nose. When your immune system overreacts to these harmless substances, your airways swell, tighten, and fill with mucus, making it hard to breathe. For many, this isn’t occasional-it’s daily. And the good news? You can take control of it.
What Really Triggers Allergic Asthma?
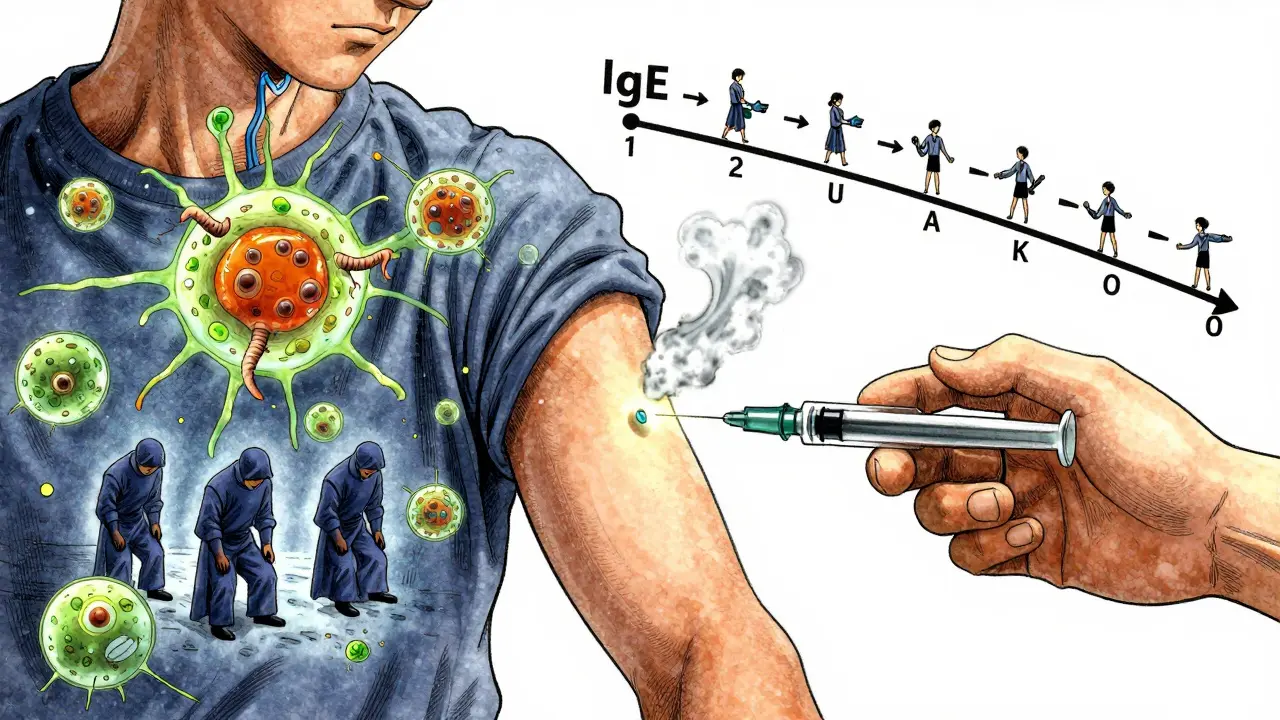
Allergic asthma isn’t caused by stress, cold air, or exercise alone. It’s tied to your body’s IgE antibodies reacting to specific allergens. These aren’t random. They’re predictable, seasonal, and often hiding in plain sight.
Outside, pollen is the biggest culprit. Tree pollen spikes from February to April, especially in March. Grass pollen hits hard in May and June. Then, in late summer, ragweed takes over-its pollen counts can hit over 100 grains per cubic meter in September. If you’ve ever had a bad asthma flare during peak season, it’s likely pollen.
Indoors, the triggers are quieter but just as dangerous. Dust mites live in your mattress, pillows, and carpets. They thrive where humidity is above 50%. In fact, 84% of U.S. homes have dust mite levels high enough to trigger asthma. Cat allergen (Fel d 1) is found in 79% of homes-even if you don’t own a cat. It sticks to clothes, furniture, and walls. Dog allergen (Can f 1) is present in two out of three homes. Mold is another silent trigger, especially Alternaria spores, which surge during thunderstorms and can send emergency room visits through the roof.
And it’s not just what’s in the air. Pollutants like PM2.5 (fine particles from traffic or smoke) damage the lining of your airways, making it easier for allergens to sneak in and start a reaction. One study showed PM2.5 exposure can increase airway permeability by 40-60% in just 24 hours.
How to Avoid Allergens-Without Moving Out
You don’t need to give up your home or your pet to manage allergic asthma. You just need smart, science-backed changes.
Start with your bedroom. Dust mites love warm, humid bedding. Replace your mattress and pillow covers with allergen-proof ones made of tightly woven fabric. These aren’t just fancy covers-they reduce dust mite exposure by up to 90%. Wash your sheets weekly in water hotter than 130°F. Cold water won’t kill them.
Use a HEPA vacuum at least twice a week. Regular vacuums just kick dust back into the air. A HEPA filter traps it. Studies show this cuts cat allergen levels by 42%. If you can, replace carpets with hard floors. If you can’t, vacuum them daily.
Control humidity. Keep it between 30% and 50%. Use a hygrometer to check. If it’s too high, run a dehumidifier. Too low, and your airways dry out. The right balance stops dust mites and mold in their tracks.
When pollen counts are high-usually above 9.7 grains per cubic meter-keep windows shut. Use air conditioning instead. If you go outside, wear an N95 mask while mowing the lawn or raking leaves. It cuts pollen exposure by 85%. Shower and change clothes right after coming in. Allergens cling to skin and hair. Leaving them on your pillow means you’re breathing them in all night.
For pet allergies, keep pets out of the bedroom. Wash them weekly with hypoallergenic shampoo. Use a HEPA air purifier in living areas. These steps won’t eliminate allergens, but they can cut exposure enough to reduce symptoms significantly.
Immunotherapy: Changing How Your Body Reacts
Medications like inhalers and antihistamines treat symptoms. But immunotherapy treats the root cause. It’s the only treatment that can actually change how your immune system responds to allergens.
There are two main types: shots (subcutaneous immunotherapy, or SCIT) and under-the-tongue tablets or drops (sublingual immunotherapy, or SLIT).
SCIT starts with weekly injections of tiny amounts of the allergen you’re sensitive to. Over 4-6 months, the dose slowly increases until you reach a maintenance level. Then you switch to monthly shots for 3-5 years. It’s not quick. But 70-80% of people see major improvement after 12-18 months. One long-term study found that after five years, people needed 40% fewer asthma medications.
SLIT is easier. You take a tablet or drop under your tongue every day. It’s less invasive. But it can cause mild itching or tingling in the mouth-especially at first. About 78% of users feel this during the first month. Still, 65% of people stick with it because it’s convenient. Studies show SLIT reduces asthma symptoms by 35% in people allergic to dust mites, compared to just 15% with inhaled steroids alone.
Both types work best when you stick with them. Stopping early means losing the benefit. The goal is long-term tolerance-not just temporary relief.
And it’s not just for pollen or dust mites. New treatments are coming fast. A new cat allergen therapy called CAT-PAD cuts the build-up phase from six months to just eight weeks. A pollen vaccine in trials requires only four doses a year. These aren’t science fiction-they’re real, FDA-approved options now or coming soon.

Who Benefits Most-and Who Doesn’t?
Allergic asthma isn’t the same for everyone. The best candidates for immunotherapy are people who:
- Have clear positive skin or blood tests for specific allergens
- Have symptoms that don’t fully respond to medication
- Want to reduce long-term drug use
- Are willing to commit to 3-5 years of treatment
But not everyone with asthma has allergic asthma. About 30% of people diagnosed with it actually have non-type 2 inflammation-meaning their immune system isn’t driven by IgE or eosinophils. Giving them immunotherapy or expensive biologics like omalizumab won’t help. That’s why testing matters. Blood tests for eosinophils (above 300 cells/µL) and FeNO (above 25 ppb) can tell if your asthma is allergic or not.
Children often respond better than adults. Studies show over 80% of kids with asthma have the allergic form. Early intervention can prevent worsening symptoms and reduce the chance of developing chronic lung problems later.
Non-allergic asthma responds better to other treatments: bronchial thermoplasty, macrolide antibiotics, or different biologics. Mixing up the diagnosis leads to wasted money and time. Biologics cost $30,000-$40,000 a year. If you don’t have the right type of asthma, you’re paying for nothing.
Real People, Real Results
One Reddit user, after years of poor peak flow readings (as low as 380 L/min), made three changes: allergen-proof bedding, a HEPA vacuum, and a whole-home dehumidifier. Six months later, their peak flow jumped to 470 L/min. No extra meds. Just better environment control.
A 12-year-old with severe cat allergy had skin test reactions so strong they measured 15mm (normal is under 3mm). After three years of cat dander immunotherapy, their IgE levels dropped from 120 kU/L to 15 kU/L. They passed a challenge test-no reaction when exposed to cats. Their asthma? Gone.
On the flip side, 68% of asthma patients in a UK survey said they still struggled with pollen season-even with proper meds. One in five had an ER visit during high pollen days. Avoidance isn’t optional. It’s part of the treatment plan.
Immunotherapy isn’t perfect. About 28% of people on shots report injection site reactions. But most are mild. And the long-term payoff? Fewer flare-ups, fewer hospital visits, less reliance on inhalers.
What’s New in 2026?
The field is moving fast. New tools are making management smarter.
The Allergen Insight nasal sensor, approved by the FDA in 2023, detects airborne allergens as low as 0.1 µg/m³. It connects to your phone and alerts you when triggers are near. No more guessing if it’s safe to go outside.
AI platforms like AsthmaIQ now combine pollen forecasts, your personal exposure history, and medication logs to predict your next asthma flare-with 92% accuracy. It’s like a weather app for your lungs.
Genetic testing is starting to show which patients will respond best to immunotherapy. A marker on chromosome 17q21 can predict response with 85% accuracy. Soon, doctors may not just treat your symptoms-they’ll tailor your treatment based on your DNA.
And insurance is catching up. Medicare now covers 80% of immunotherapy costs. In Europe, where universal healthcare is the norm, nearly 28% of allergic asthma patients get immunotherapy. In the U.S., it’s still only 15%. But that number is rising.
What You Can Do Today
If you have asthma and think allergens might be triggering it:
- Get tested. Skin prick or blood tests can confirm which allergens matter.
- Track your symptoms. Note when they get worse-seasons, pets, cleaning, weather.
- Start with avoidance. Change bedding, control humidity, vacuum with HEPA, keep windows closed on high-pollen days.
- Talk to your doctor about immunotherapy. It’s not a last resort. It’s a long-term solution.
- Ask about biomarkers. Blood eosinophils and FeNO can tell you if you’re a good candidate for biologics or immunotherapy.
Allergic asthma doesn’t have to control your life. It’s not a life sentence. With the right triggers identified, the right avoidance steps taken, and the right treatment chosen, you can breathe easier-for good.


Dave Old-Wolf
January 8, 2026 AT 03:23My asthma got way worse after we got the cat. Didn't realize it was the dander until I read this. I switched to HEPA vacuum and allergen-proof covers, and honestly? My peak flow went up 50 points in two months. No meds added. Just cleaner air.
Kristina Felixita
January 8, 2026 AT 22:08OMG YES. I used to cry every spring because I couldn't breathe. Then I started wearing an N95 when I raked leaves. I know it looks ridiculous but I'm alive and I don't need my inhaler every other hour anymore. Also, shower after being outside. It's not optional. It's survival.
Donny Airlangga
January 10, 2026 AT 00:30I’ve been on immunotherapy for 3 years now. The first six months were rough-itchy mouth, weird fatigue. But after year two? I stopped needing my nightly inhaler. My doctor said my IgE levels dropped like a rock. It’s not magic. It’s science. And it works if you stick with it.
Molly Silvernale
January 10, 2026 AT 06:28They say asthma is a silent epidemic… but it’s not silent-it’s screaming in the middle of the night when you’re gasping for air like a fish on pavement. And nobody listens until you’re in the ER again. This post? It’s the first time I felt seen.
Evan Smith
January 11, 2026 AT 23:54So wait… you’re telling me I could’ve avoided all this by just vacuuming with a HEPA filter and not letting my cat sleep on my pillow? I spent $2000 on biologics last year. I feel like a fool.
Luke Crump
January 13, 2026 AT 14:28Let’s be real-this is just corporate asthma propaganda. Big Pharma wants you to believe you need $40k/year drugs or ‘immunotherapy’ to breathe. Meanwhile, in ancient India, they just drank turmeric milk and breathed through their nose. Maybe we’re overcomplicating this? Nature didn’t give us asthma. Modern life did. And we’re still buying the lie.
Manish Kumar
January 15, 2026 AT 00:56You know, in India, we don’t have this obsession with HEPA filters and allergen-proof bedding. We live with dust, with pets, with pollen-and we don’t die. My grandmother had asthma since she was 12, never used a mask, never changed her mattress, and lived to 92. Maybe the problem isn’t the allergens… maybe it’s the fear of them? We’ve turned breathing into a performance.
Aubrey Mallory
January 15, 2026 AT 22:50Stop romanticizing ‘natural living.’ If you have allergic asthma, your immune system is broken. You don’t get to ignore science because it’s inconvenient. HEPA filters aren’t a luxury-they’re a medical device. If you refuse to use them, you’re not ‘living authentically,’ you’re just being reckless. And your kids might pay for it.
Annette Robinson
January 17, 2026 AT 06:07I appreciate the data here. But I want to say thank you to the person who shared their peak flow numbers. That’s the moment it clicked for me. I didn’t realize how much improvement was possible without adding more meds. I’m getting tested this week.
Joanna Brancewicz
January 17, 2026 AT 13:57FeNO >25 ppb + eosinophils >300 = Type 2 inflammation. If you’re not testing for these, you’re guessing. And guessing with asthma is dangerous. Get the labs. Don’t wait for an ER visit.
Lois Li
January 18, 2026 AT 10:54My mom used to say ‘just breathe through your nose’ like it was a magic spell. I thought she was being naive. Then I tried nasal breathing during a pollen spike… and I didn’t collapse. It’s not a cure, but it helps. And it’s free. So maybe there’s something to old advice after all.
swati Thounaojam
January 20, 2026 AT 00:46My brother had asthma and he used to say ‘I just need to get away from the city.’ He moved to the mountains. Didn’t help. Turns out pollen travels. And mold grows everywhere. You can’t out-run it. You have to out-smart it.
Ken Porter
January 20, 2026 AT 20:34Immunotherapy? In the US? Good luck getting insurance to cover it. We pay $1000/month for inhalers and call it healthcare. Meanwhile, Europe gives people shots for free. Guess which system actually works?
Prakash Sharma
January 21, 2026 AT 04:14Why are Americans so obsessed with buying solutions? In India, we use neem leaves, steam inhalation, and honey. You don’t need $40k treatments. You need discipline. And maybe less plastic. Your house is a chemical swamp. Clean it with water, not gadgets.