Anticoagulation Dose Calculator for Kidney & Liver Disease
Input Parameters
15
45
90
When someone has both kidney disease and liver disease, taking a blood thinner isn’t just tricky-it’s a tightrope walk between clotting and bleeding. This isn’t theoretical. Real people with atrial fibrillation, deep vein thrombosis, or mechanical heart valves need anticoagulation, but their organs can’t handle standard doses. And the drugs we think are safer-like apixaban or rivaroxaban-weren’t tested in these patients. So what do doctors actually do?
Why Standard Doses Don’t Work
Most blood thinners are cleared by the kidneys or liver. In healthy people, that’s fine. But when the kidneys are failing, drugs like dabigatran build up fast-80% of it leaves the body through urine. That’s why dabigatran is banned in patients with eGFR under 30. Rivaroxaban? About a third is cleared by the kidneys. Apixaban? Only 27%. That’s why apixaban is the go-to for advanced kidney disease, even though it wasn’t approved for it originally. Liver disease is worse. It doesn’t just slow drug clearance. It messes with the whole clotting system. The liver makes clotting factors, but it also makes natural anticoagulants. When it’s damaged, you get a fragile balance. A patient might have a normal INR but still be at high risk for bleeding because their platelets are low, their fibrinogen is gone, and their body can’t make protein C or antithrombin. INR? It’s useless here.Kidney Disease: What the Numbers Mean
Staging matters. If your eGFR is above 45, most DOACs are safe at standard doses. But once you hit stage 3b (eGFR 30-44), things change. Apixaban drops from 5 mg twice daily to 2.5 mg. Rivaroxaban drops from 20 mg to 15 mg. Edoxaban from 60 mg to 30 mg. These aren’t guesses-they’re FDA-approved adjustments based on real data. Now, stage 4 and 5 (eGFR under 30) is where the controversy explodes. The European Medicines Agency says don’t use rivaroxaban or apixaban. The FDA says apixaban 2.5 mg twice daily is okay. Why the difference? Because the ARISTOTLE trial showed that in patients with eGFR under 30, apixaban cut major bleeding by 70% compared to warfarin. That’s huge. But here’s the catch: those patients were still getting dialysis. And dialysis doesn’t remove apixaban much-it just makes levels unpredictable. For patients on hemodialysis, studies show apixaban 2.5 mg twice daily gives a trough level of about 47 ng/mL. Normal? Around 112. So you’re getting less than half the exposure. But is that enough to prevent strokes? The 2021 Nephrology Dialysis Transplantation registry of over 12,000 dialysis patients found DOACs had slightly lower bleeding rates than warfarin-and similar stroke rates. That’s why some doctors are using apixaban, even though guidelines say not to.Liver Disease: The INR Lie
If you’ve ever seen a cirrhotic patient on warfarin, you know the frustration. INR jumps from 1.8 to 3.5 overnight with no dose change. Why? Because the liver can’t make clotting factors consistently. That INR only measures vitamin K-dependent factors. It ignores everything else: low platelets, low fibrinogen, high fibrinolysis. The Child-Pugh score is your real guide. Child-Pugh A? DOACs are probably okay at normal doses. Child-Pugh B? Use caution. Reduce dose. Monitor closely. Child-Pugh C? Don’t use DOACs. Period. The RE-CIRRHOSIS study showed a 5.2-fold higher risk of major bleeding in this group. Warfarin has its place here-not because it’s better, but because we know how to reverse it. Vitamin K, fresh frozen plasma, prothrombin complex concentrate. But even that’s unreliable. One study found cirrhotic patients only stayed in the therapeutic INR range 45% of the time. Compare that to 65% in people with healthy livers. That’s why some hepatologists now use thromboelastography (TEG) or ROTEM. These tests show how the whole clot forms and breaks down-not just one number. But only 38% of U.S. hospitals have them.
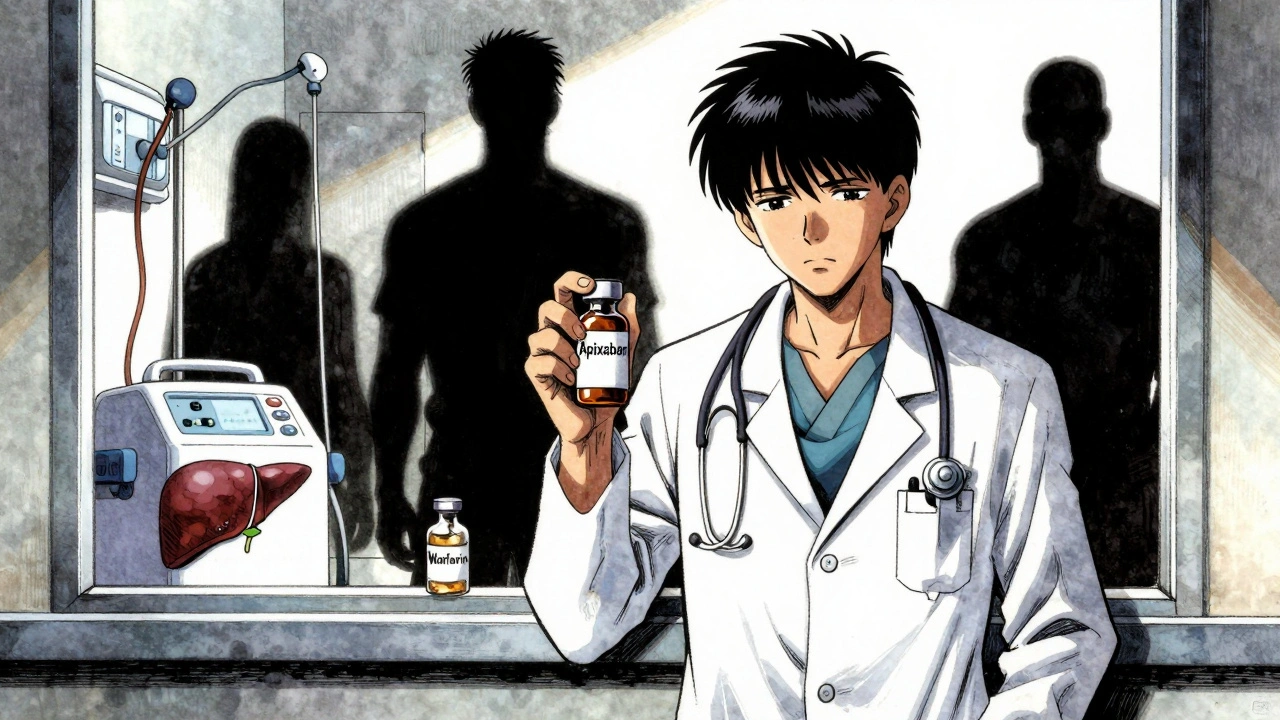
Apixaban vs. Warfarin: The Real Comparison
In kidney disease, apixaban wins on safety. The ARISTOTLE subgroup analysis showed 31% lower major bleeding risk in patients with eGFR 25-30. And for intracranial bleeding? DOACs cut it by 62% compared to warfarin. That’s life-saving. But in end-stage kidney disease, warfarin still has a role. Why? Mechanical heart valves. DOACs are not approved for them. And in patients with recurrent clots on DOACs, warfarin may be the only option left. In liver disease, warfarin’s main advantage is reversibility. But it’s a gamble. Apixaban has no proven reversal agent for liver patients, and andexanet alfa (Andexxa®) costs $19,000 per dose and isn’t available in most hospitals. Idarucizumab (Praxbind®) only works for dabigatran. So if you’re using apixaban in a cirrhotic patient and they bleed out? You’re stuck.What the Experts Disagree On
There’s a transatlantic divide. European guidelines say: no DOACs in dialysis patients. American guidelines say: maybe apixaban 5 mg daily, if no other option. Why? Because the AUGUSTUS trial subanalysis showed fewer bleeds with apixaban in dialysis patients. But the RENAL trial found rivaroxaban caused 2.8 times more GI bleeding in dialysis patients than warfarin. One nephrologist on Reddit said he’s treated 15 dialysis patients on apixaban 2.5 mg daily for two years-no bleeds. Another said one patient had a fatal retroperitoneal bleed. That’s the reality. No one has a perfect answer. For liver disease, some doctors say: treat the patient, not the INR. Others say: if you’re going to anticoagulate a cirrhotic, you need to know why. Portal vein thrombosis? That’s a different risk-benefit than atrial fibrillation. One can be deadly without anticoagulation. The other? Maybe not.
Practical Steps: What You Can Do Today
If you’re managing a patient with both kidney and liver disease:- Check eGFR with CKD-EPI, but don’t trust it if the number is under 30. Use cystatin C if available.
- Use Child-Pugh score-not MELD-to assess liver function for anticoagulation decisions.
- If eGFR is under 30 and Child-Pugh is B or C, avoid DOACs unless no other option.
- If you must use a DOAC, apixaban 2.5 mg twice daily is the least risky choice.
- Monitor platelets monthly. If they drop below 50,000/μL, reconsider anticoagulation.
- Don’t rely on INR in liver disease. If you have access to TEG or ROTEM, use it.
- Have a plan for bleeding. Know what reversal agents your hospital carries-and if they’re even available.
The Future Is Coming
Two big trials are underway. The MYD88 trial is randomizing 500 dialysis patients to apixaban vs. warfarin. Results in 2025. The LIVER-DOAC registry is tracking 1,200 cirrhotic patients on DOACs worldwide. That’s the first real data we’ll have. The FDA is preparing new labeling for apixaban in end-stage kidney disease. KDIGO’s updated guidelines are due in late 2024. They’ll likely recommend apixaban for select patients with advanced CKD, even if they’re on dialysis. Right now, we’re making decisions based on fragments: pharmacokinetics, subgroup analyses, registry data. We don’t have the big RCTs. But we can’t wait. Patients are dying from clots-or from bleeding. The best we can do is be honest, be cautious, and document every decision.There’s no perfect answer. But there’s a better way: work with nephrologists, hepatologists, and hematologists. Don’t guess. Don’t follow a checklist. Talk to your team. Because when kidneys and livers fail together, the answer isn’t in the drug label-it’s in the room with the patient.

Katherine Rodgers
December 11, 2025 AT 08:23Lauren Dare
December 12, 2025 AT 02:34Gilbert Lacasandile
December 13, 2025 AT 08:46Lola Bchoudi
December 13, 2025 AT 22:37Morgan Tait
December 15, 2025 AT 01:32Darcie Streeter-Oxland
December 16, 2025 AT 04:20Taya Rtichsheva
December 16, 2025 AT 05:20Christian Landry
December 16, 2025 AT 11:16Katie Harrison
December 18, 2025 AT 04:33Mona Schmidt
December 18, 2025 AT 12:03Guylaine Lapointe
December 19, 2025 AT 13:53Sarah Gray
December 19, 2025 AT 17:21Michael Robinson
December 19, 2025 AT 20:44Kathy Haverly
December 20, 2025 AT 05:46