Every year, millions of people walk into a pharmacy looking for relief from a headache, a cold, or stomach upset. They grab a box off the shelf, pay at the counter, and head home - no prescription needed. But here’s the thing: just because you don’t need a doctor’s note doesn’t mean these medications are harmless. In fact, OTC medications cause more than 198,000 emergency room visits in the U.S. each year, mostly because people don’t read the label or mix the wrong things together.
Read the Drug Facts Label - Every Time
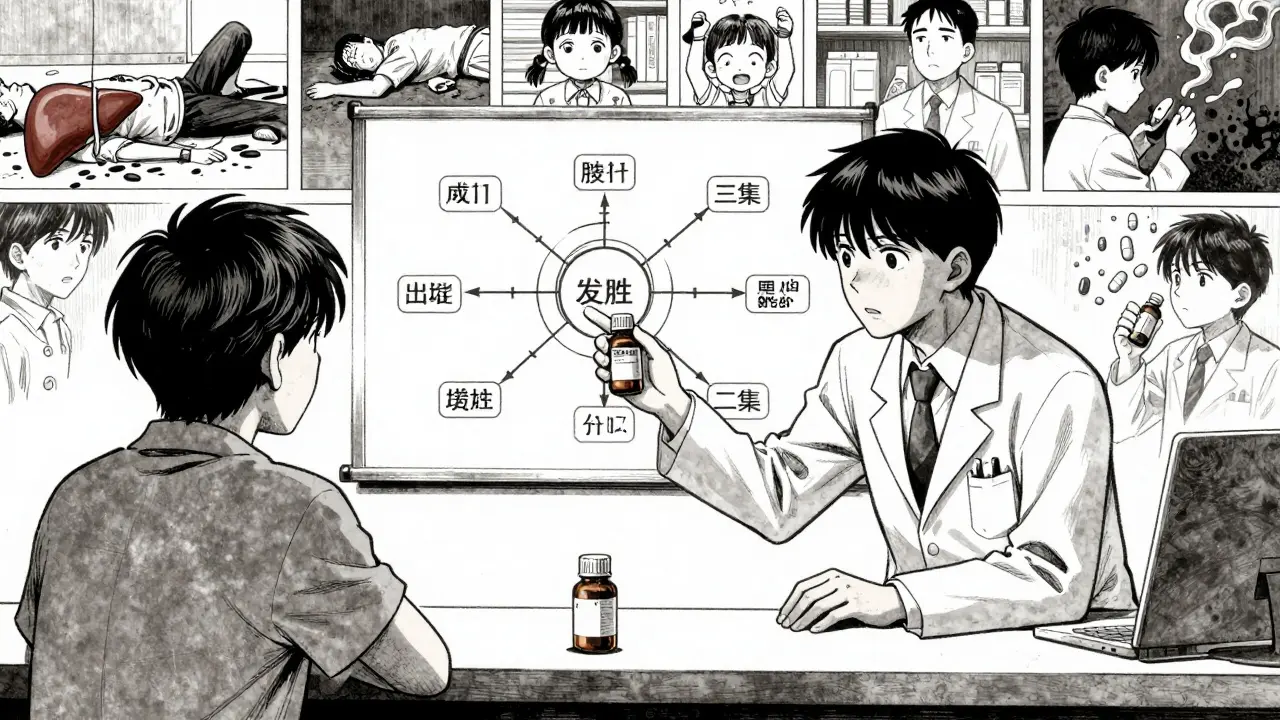
The first and most important step? Look at the Drug Facts label. It’s not just a sticker. It’s your safety manual. Since 1999, the FDA has required every OTC medicine to use this standard format. That means no matter what brand you pick - Tylenol, Advil, or a store-brand version - the information is laid out the same way.Start with the active ingredients. This is the part that actually does the work. If you’re taking more than one OTC product, you might be doubling up without realizing it. For example, Tylenol, Excedrin, and many cold medicines all contain acetaminophen. Taking two of them together can push you over the safe daily limit - 4,000 milligrams for most adults - and cause serious liver damage. In fact, acetaminophen overdose is the leading cause of acute liver failure in the U.S., with around 56,000 ER visits each year.
Next, check the purpose and uses. Are you taking this for fever, or for a runny nose? If you only have a headache, don’t buy a multi-symptom cold remedy full of decongestants, antihistamines, and cough suppressants you don’t need. More ingredients don’t mean better results - they mean more chances for side effects or interactions.
Know What’s in Your Medicine
Some ingredients are safer than others, depending on your health. Here’s what to watch for:- Acetaminophen - Great for pain and fever, but dangerous for your liver if you drink alcohol, have liver disease, or take more than directed.
- Ibuprofen or naproxen - Good for inflammation, muscle pain, or menstrual cramps. But they can irritate your stomach, raise blood pressure, or hurt your kidneys if you have heart or kidney issues.
- Decongestants (pseudoephedrine, phenylephrine) - These can spike your blood pressure and make heart problems worse. Avoid them if you have high blood pressure, heart disease, or an enlarged prostate.
- Antihistamines (diphenhydramine, chlorpheniramine) - Help with allergies and sleep, but they cause drowsiness, dry mouth, and can make it hard to urinate if you have prostate issues.
- Dextromethorphan - A cough suppressant that’s safe at recommended doses, but can cause serious side effects if taken in large amounts - and some people abuse it.
Always ask yourself: Do I really need this ingredient? If you’re unsure, skip it. Simpler is safer.
Dosing Matters - Especially for Kids and Seniors
Children aren’t just small adults. Giving a child an adult dose - even half of it - can be deadly. Always use the measuring tool that comes with the medicine. A teaspoon isn’t a tablespoon. A kitchen spoon? Even worse. Studies show kitchen spoons can vary by up to 200% in volume. That means you could be giving your child twice the dose - or half - without knowing it.For older adults, the risks are different. As we age, our bodies process medicine slower. Many seniors take multiple prescriptions, and adding an OTC pill can create dangerous interactions. For example, mixing an OTC pain reliever with a blood thinner like warfarin can cause bleeding. Or combining a sleep aid with a prescription sedative can slow your breathing to dangerous levels.
One in two adverse drug reactions in older adults comes from OTC medicines. That’s not because they’re careless - it’s because the labels don’t always make it clear what’s safe for them.

Talk to the Pharmacist - It’s Free
You paid for the medicine. You didn’t pay for the advice. But here’s the truth: pharmacists are trained to help you. They see hundreds of people every week. They know which products are overhyped, which ones have hidden risks, and which ones actually work.Don’t be shy. Say: “I’m taking this for my headache, but I’m also on high blood pressure medicine. Is this safe?” Or: “I’m 72 and take five prescriptions. Can you check if this cold medicine will mix with them?”
Pharmacist consultations reduce OTC medication errors by 67%. That’s not a guess - it’s a study result from the Research in Social and Administrative Pharmacy journal. And you don’t need an appointment. Just ask when you pick up your medicine.
Check for Interactions - Even with Supplements
You might think herbal supplements are harmless. But they’re not. St. John’s wort can make birth control, antidepressants, and blood thinners less effective. Garlic pills and ginkgo biloba can increase bleeding risk - especially before surgery. Even vitamin E in high doses can interfere with blood thinners.Keep a list of everything you take: prescription drugs, OTC medicines, vitamins, and supplements. Bring it to your doctor and your pharmacist. If you don’t have a list, write it down the next time you’re at the pharmacy. It takes five minutes. It could save your life.
Don’t Use Old Medicine
That bottle of ibuprofen from last winter? It’s probably still safe to take - if it’s within the expiration date. But if it’s been sitting in a hot car, a damp bathroom, or a drawer for three years, it’s not worth the risk. Medicines lose potency over time. Some can even break down into harmful substances.Also, never take medicine prescribed for someone else. Just because it worked for your partner doesn’t mean it’s right for you. Different health conditions, different weights, different reactions. What’s safe for one person could be dangerous for another.
Know When to Stop - and When to See a Doctor
OTC meds are for short-term relief. If your headache lasts more than three days, your fever doesn’t go down after 48 hours, or your cough won’t quit after a week - it’s time to see a doctor. These aren’t just signs you need a stronger pill. They could be signs you need a different kind of care.Same goes for symptoms like chest pain, confusion, trouble breathing, or swelling. Don’t try to medicate your way out of those. Call your doctor or go to urgent care.
Stick With One Pharmacy
It’s easy to switch pharmacies for convenience - maybe one’s closer, or has better prices. But if you use multiple pharmacies, your medication history gets split up. That means no one has the full picture of what you’re taking. If you get all your prescriptions and OTC meds from one place, your pharmacist can flag dangerous combinations before you even walk out the door.It’s not just about saving money. It’s about safety.
What’s New in 2026?
The FDA is still updating the rules for OTC drugs. In 2023, they approved the first over-the-counter nasal steroid for allergies - fluticasone furoate. That means people with seasonal allergies can now skip the doctor for a treatment that used to require a prescription.And by 2025, the FDA plans to finish a major overhaul of the OTC drug review system. This is the first big update in over 50 years. The goal? Faster updates to safety info, clearer labels, and better warnings - especially for older adults and people with chronic conditions.
But until then, you’re still the one holding the bottle. So read the label. Ask questions. Don’t guess. Your body will thank you.


Barbara Mahone
January 21, 2026 AT 05:17I used to grab whatever was on sale until I ended up in the ER for liver enzyme spikes. Turns out I was doubling up on acetaminophen between my cold medicine and my sleep aid. Now I keep a little notebook by the sink. Write it down. Don’t trust your memory. Simple.
Ashok Sakra
January 22, 2026 AT 11:51bro why are you scared of medicine?? i took 4 advil and 2 tylenol and i felt like a god. also my dog took my old cough syrup and lived. so chill.
Andrew Rinaldi
January 23, 2026 AT 11:08It’s funny how we treat OTC meds like snacks but would never eat a random pill off the street. The label isn’t bureaucracy-it’s a conversation your body is having with you. If you skip it, you’re just ignoring the warning signs. Not reckless. Just unaware.
Gerard Jordan
January 24, 2026 AT 23:27Pharmacists are the unsung heroes of healthcare 🙌 I once asked mine if my turmeric supplement was okay with my blood thinner. She said, ‘Nope, and here’s a paper on why.’ Free advice? Yes. Life-saving? Absolutely. Go talk to them. They’re not just the people who hand you the box.
lokesh prasanth
January 26, 2026 AT 11:36label? what label? i read the front. 'headache relief' = i take it. problem solved. why overthink?
Malvina Tomja
January 28, 2026 AT 03:22It’s embarrassing that we need a 2,000-word essay to tell people not to mix Tylenol and alcohol. This isn’t rocket science. It’s basic biology. If you can’t read a label, maybe you shouldn’t be self-medicating. Period.
MARILYN ONEILL
January 29, 2026 AT 19:25I only buy name brands. Store brands are for people who don’t care if they die slow. Also, I don’t trust pharmacists. They’re just trying to upsell you. I’ve read the FDA website. I know better.
Philip Williams
January 30, 2026 AT 02:14My grandmother took a new OTC sleep aid and ended up in a hospital with confusion and urinary retention. She’d never taken anything like it before. The label didn’t mention elderly risk. That’s the problem-not the user, but the system. We need clearer warnings for aging bodies.
Ben McKibbin
January 31, 2026 AT 13:17One pharmacy. Always. I used to hop between CVS, Walgreens, and the corner store-until my pharmacist flagged that my OTC antihistamine was canceling out my blood pressure med. She pulled up my entire history in 30 seconds. That’s the power of continuity. Don’t make your health a puzzle.