Most people think sleep problems are just about being tired. But if you’re always wide awake at 3 a.m. and can’t fall asleep until dawn-even on weekends-that’s not laziness. It’s your body clock out of sync. Same goes for hopping on a plane and feeling wrecked for days, even after a full night’s sleep. These aren’t just bad nights. They’re circadian rhythm disorders.
What Your Body Clock Is Doing
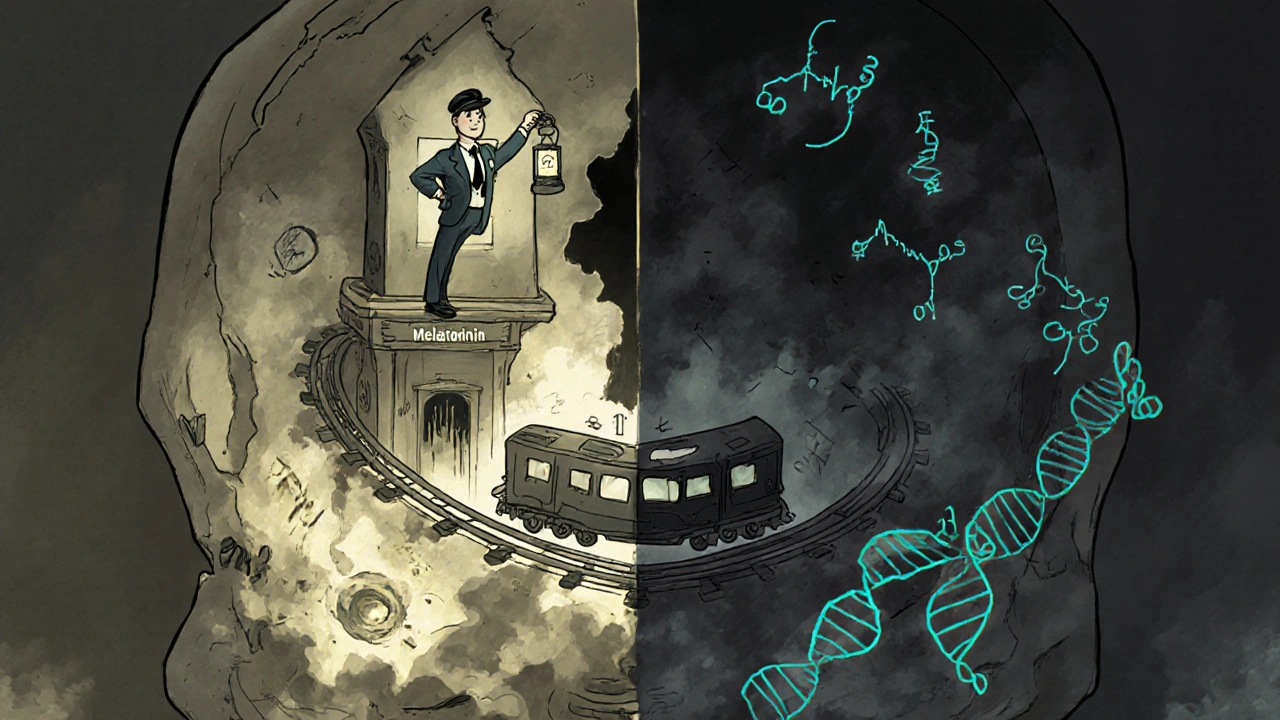
Your body runs on a 24-hour internal timer called the circadian rhythm. It’s not just about sleep. It controls when you feel hungry, when your body temperature drops, when hormones like cortisol and melatonin kick in. This rhythm is guided by light-especially morning sunlight-and kept in sync by a tiny cluster of cells in your brain called the suprachiasmatic nucleus. Think of it like a conductor leading an orchestra. If the conductor gets confused, everything falls out of tune.
When this system gets disrupted, you don’t just feel groggy. Your metabolism, mood, focus, and even immune response take a hit. Studies show people with untreated circadian disorders have a 29% higher risk of type 2 diabetes and a 23% higher risk of heart disease. That’s not a small thing. It’s a silent, slow-burning health risk.
Jet Lag: The Traveler’s Curse
Jet lag hits fast. You land in Tokyo after a 12-hour flight from Adelaide, and suddenly it’s 10 p.m. your body thinks it’s 4 a.m. You’re exhausted, but your brain won’t shut down. Your stomach churns. You can’t concentrate. This isn’t fatigue from flying-it’s your internal clock stuck in Adelaide while the world moved ahead.
Here’s the catch: eastbound travel is worse. Why? Because your body naturally wants to stay up later, not go to bed earlier. Crossing five time zones eastward? That’s about 7.5 hours of misalignment. Your body can only adjust about 1 hour per day when moving forward. So it takes 7-8 days to fully reset. Westbound? You’re delaying your clock-something your body does naturally. You might feel off for only 3-4 days.
Most travelers don’t know this: the key isn’t just sleeping on the plane. It’s managing light. If you’re flying east, get bright light in the morning at your destination. Avoid it in the evening. If you’re flying west, seek light in the late afternoon and early evening. No light therapy? Then start shifting your sleep schedule 1 hour earlier (for east) or later (for west) three days before you leave. It’s not magic-it’s physics. Your clock needs time to catch up.
Delayed Sleep Phase Disorder: When Night Is Your Day
Jet lag fades. Delayed sleep-wake phase disorder (DSWPD) doesn’t. This is a chronic condition where your sleep time is pushed back by two or more hours. You don’t fall asleep until 3-6 a.m. You wake up between 10 a.m. and 1 p.m. And if you force yourself to sleep earlier? You lie awake for hours. But if you follow your natural rhythm? You sleep deeply, fully, and feel fine.
This isn’t just a teen thing. It affects 7-16% of adolescents and young adults. But it doesn’t disappear. Many adults live with it for years. A 22-year-old student in a Reddit thread said they failed 8 a.m. classes despite accommodations. A 28-year-old software developer said their best work happens at 2 a.m.-but they’re stuck in a 9-to-5 job. The result? Chronic fatigue, anxiety, burnout.
Doctors can measure this. Dim light melatonin onset (DLMO)-when your body starts releasing sleep hormone melatonin-happens about two hours later in people with DSWPD than in others. That’s not a preference. It’s biology. And it’s genetic. Variants in genes like PER3 and CRY1 explain why some people are wired to be night owls.
How to Fix It-Without Pills
Most people reach for melatonin supplements. But here’s the problem: 80% of people take too much. The recommended dose is 0.5 mg-about the size of a grain of rice. Most over-the-counter pills are 3-5 mg. That’s like using a firehose to water a plant. High doses can make your body stop responding, or even shift your rhythm the wrong way.
The real fix? A three-part plan backed by the American Academy of Sleep Medicine:
- Morning light therapy: Sit in bright light (10,000 lux) for 30-60 minutes within an hour of your natural wake time. A light box works. So does sitting by a window with no sunglasses. Even on cloudy days, outdoor light is 10x brighter than indoor lighting.
- Evening melatonin: Take 0.5 mg five to seven hours before your target bedtime. Not when you’re tired. Not after dinner. Five to seven hours before you want to sleep. That’s when your body expects it.
- Consistency: No sleeping in on weekends. No staying up late to ‘catch up.’ Your body needs predictability. Even one late night can undo a week of progress.
Studies show this combo moves your sleep time forward by 2.1 hours on average over four weeks. Alone, melatonin moves it 1.3 hours. Light alone? 1.5 hours. Together? It’s powerful.
But here’s the hard truth: 78% of people fail because they break the schedule on weekends. That’s why apps like Timeshifter exist. They use algorithms to tell you exactly when to get light, when to avoid it, and when to take melatonin based on your travel schedule or sleep goal. A 2023 trial showed users recovered from jet lag 63% faster than those using basic advice.
What Doesn’t Work (And Why)
People try everything: sleeping pills, caffeine, alcohol, modafinil. But none fix the root problem. Sleeping pills might knock you out, but they don’t reset your clock. Caffeine at 10 p.m.? You’ll lie awake, wired and frustrated. Alcohol makes you fall asleep faster-but it ruins deep sleep and fragments your rhythm.
Modafinil, a stimulant sometimes prescribed for shift workers, is especially risky. One 19-year-old on HealthUnlocked.com took it for months to stay awake for class. It worked-until it didn’t. Then they developed insomnia that made their DSWPD worse. Studies show 22% of people with circadian disorders misuse stimulants or sedatives, making their condition harder to treat.
And don’t assume it’s just ‘not trying hard enough.’ This isn’t discipline. It’s biology. Telling someone with DSWPD to ‘just go to bed earlier’ is like telling a diabetic to ‘just stop eating sugar.’ It ignores the system.
Why This Matters More Than You Think
There are 1.2 billion people worldwide who work non-traditional hours. That’s 20% of the global workforce. Shift work disorder affects 10-40% of night workers, who average 1.4 hours less sleep per day than day workers. That’s not just tiredness. That’s increased risk of obesity, cancer, depression, and heart disease.
And it’s not just workers. Students, parents, caregivers, freelancers-all of us are fighting against a world designed for 8 a.m. to 5 p.m. But human biology isn’t built that way. The global sleep disorder market is now worth $53.7 billion. Circadian rhythm treatments make up $6.4 billion of that. And yet, only 4% of people with symptoms have been diagnosed.
Why? Because doctors still think it’s ‘bad habits.’ But science says otherwise. The 2023 ICSD-4 guidelines now require objective measurements like DLMO for diagnosis. That’s a big shift. It means we’re finally treating this like a real medical condition-not a lifestyle flaw.
What You Can Do Today
If you’re struggling with jet lag after a trip:
- Get sunlight within 30 minutes of waking at your destination.
- Avoid bright screens after 8 p.m. Use night mode if you must use them.
- Wait 24 hours before taking melatonin. Let your body start adjusting naturally first.
If you think you have delayed sleep phase disorder:
- Track your sleep for two weeks. Use a free app or journal. Note when you fall asleep and wake up naturally-even on weekends.
- If your sleep time is consistently 3 a.m. to 11 a.m. or later, and you’ve felt this way for more than three months, you likely have DSWPD.
- Start with 0.5 mg melatonin 6 hours before your desired bedtime. Add 30 minutes of bright light immediately after waking.
- Stick to the same wake time every day, even on weekends. It’s the hardest part. But it’s the most important.
It takes 4-6 weeks to see real change. But once you do, the difference is life-altering. You stop feeling like a failure. You stop blaming yourself. You realize your body wasn’t broken-it was just out of sync.
When to See a Doctor
You don’t need to suffer in silence. If you’ve tried consistent light and melatonin for six weeks with no improvement, or if your sleep issues are affecting your job, school, or relationships, talk to a sleep specialist. They can order a DLMO test or use actigraphy (a wrist monitor that tracks movement and light exposure) to confirm the diagnosis.
There are no quick fixes. But there are real, science-backed solutions. And they work-if you give them time.
Is jet lag the same as delayed sleep phase disorder?
No. Jet lag is temporary and caused by traveling across time zones. Your body will reset on its own in a few days. Delayed sleep phase disorder is a chronic condition where your internal clock is permanently shifted later-often by two or more hours. It doesn’t go away without treatment, even if you don’t travel.
Can melatonin cure delayed sleep phase disorder?
Melatonin alone isn’t enough. While it helps signal sleep time, studies show it only shifts your rhythm by about 1.3 hours. To get a full 2+ hour advance, you need melatonin + morning light + strict schedule consistency. Most people who only use melatonin don’t see lasting results.
Why is eastbound jet lag worse than westbound?
Your body’s natural circadian period is about 24.2 hours, which means it’s easier to delay sleep (stay up later) than to advance it (go to bed earlier). Eastbound travel forces you to go to bed earlier-something your body resists. Westbound travel lets you stay up later, which your body does naturally. That’s why eastbound trips take longer to recover from.
Can teenagers outgrow delayed sleep phase disorder?
Some do, but not all. About 40% of adolescents with DSWPD continue to have symptoms into adulthood. It’s not just a phase-it’s often genetic. Early treatment with light and melatonin can help reset the rhythm before it becomes deeply entrenched. Waiting usually makes it harder to fix later.
Do I need a sleep study to diagnose delayed sleep phase disorder?
Not always. A sleep specialist can often diagnose DSWPD based on a sleep diary and actigraphy (a wrist monitor that tracks sleep patterns). But for confirmation, they may test your dim light melatonin onset (DLMO)-a blood or saliva test that shows when your body naturally releases melatonin. If it’s two or more hours later than normal, it’s a strong indicator of DSWPD.
Is it okay to sleep in on weekends if I have DSWPD?
No. Sleeping in-even one hour-on weekends resets your clock and makes it harder to adjust during the week. Consistency is the most important part of treatment. You might feel exhausted on Monday, but sticking to your schedule will make your body adapt over time. The first two weeks are the hardest. After that, it gets easier.


Jeremy Hernandez
November 18, 2025 AT 03:41Bro just stop taking melatonin like it’s candy. I took 5mg for a week and woke up feeling like a zombie who got hit by a bus. The doc told me 0.5mg is all you need - that’s like a grain of rice, not a damn vitamin. I thought I was fixing my sleep, but I was just poisoning my clock. Now I just sit by a window at 7 a.m. and let the sun do the work. No pills. No apps. Just sunlight and discipline.
Tarryne Rolle
November 18, 2025 AT 15:55It’s funny how we’ve been conditioned to believe that 9-to-5 is the natural human rhythm. The truth? Humans evolved to sleep when it’s dark and wake when it’s light. Our entire industrial society is built on a lie - that we should all conform to the same schedule. The real disorder isn’t your circadian rhythm - it’s the system that punishes you for being biologically honest.
Kyle Swatt
November 20, 2025 AT 02:20Man I used to think I was lazy because I couldn’t wake up before noon. Then I found out my DLMO was two hours behind everyone else’s. It’s not weakness. It’s not laziness. It’s just my genes wired me to be a night owl. I work from 2 a.m. to 10 a.m. now. My brain is sharp, my creativity is on fire. The world needs night people too. We’re not broken - we’re just running on a different clock. And honestly? I think we’re the ones who see the world more clearly when everyone else is asleep.
Try telling a poet they’re broken because they write at 3 a.m. Tell a coder their code is trash because they don’t show up at 8 a.m. We’re not defective. We’re just not programmed for your schedule.
Deb McLachlin
November 21, 2025 AT 12:13While the article presents compelling scientific evidence regarding circadian rhythm disorders, I would encourage readers to consult peer-reviewed studies from the Journal of Clinical Sleep Medicine for further validation. The recommendation of 0.5 mg melatonin aligns with recent meta-analyses, but the long-term efficacy of light therapy varies significantly across populations. Additionally, the claim that 78% of individuals fail due to weekend deviation lacks a cited source. Transparency in data sourcing is critical for public health messaging.
saurabh lamba
November 23, 2025 AT 11:59bro i just sleep when i feel like it. why u gotta make it so complicated? melatonin? light box? u sound like a robot. i work at night, sleep at noon, eat when hungry. life is simple. u just overthink everything. chill.
:)
Kiran Mandavkar
November 24, 2025 AT 04:11You people treat this like it’s a lifestyle tweak. This is biological warfare against your own physiology. The fact that doctors still call it a ‘habit’ proves how ignorant the medical establishment is. My PER3 gene variant doesn’t care about your 9-to-5 corporate slavery. I’ve seen people on modafinil for years - they’re not fixing anything, they’re just chemically numbing their own bodies. Wake up. Your body isn’t broken - your society is.
Eric Healy
November 26, 2025 AT 03:32light therapy my ass. i tried it for 2 weeks and still woke up at 4am. u think sunlight fixes everything? lol. i dont even have a window in my apartment. what am i supposed to do sit in the parking lot at 6am? and dont even get me started on melatonin. i took it and had nightmares about floating clocks. this whole thing feels like a cult.
Shannon Hale
November 26, 2025 AT 19:37OMG I WAS THIS PERSON. I thought I was just a lazy, unmotivated mess. I failed three classes because I couldn’t wake up. I cried in the shower every Monday. Then I found out I had DSWPD. I started the 0.5mg melatonin + light therapy + NO WEEKEND SLEEPING IN. And guess what? After six weeks - I didn’t just wake up. I felt ALIVE. Like my brain had been wrapped in plastic and someone finally peeled it off. I’m not exaggerating. This changed my life. If you’re reading this and you’re still sleeping in on weekends - stop. Just stop. Your future self will thank you.
Holli Yancey
November 27, 2025 AT 00:47I just wanted to say thank you for writing this. I’ve lived with this for years and never felt understood. People tell me I’m just not trying hard enough. But it’s not about willpower. It’s biology. I’m not lazy. I’m just wired differently. And knowing there’s a real, science-backed way to fix this - it gives me hope. I’m starting light therapy tomorrow. No pills. Just the sun. And maybe… maybe I’ll finally feel like myself.
Gordon Mcdonough
November 27, 2025 AT 21:46WHY DO PEOPLE THINK THIS IS A CHOICE??? I’M AN AMERICAN. I WORK HARD. I DON’T SLEEP IN. I’M NOT SOME EUROPEAN WHO SITS AROUND DRINKING COFFEE UNTIL NOON. I’VE BEEN WAKING UP AT 5AM SINCE I WAS 16. MY GRANDPA WORKED ON A FARM. MY DAD WORKED IN A FACTORY. AND NOW I’M SUPPOSED TO BELIEVE THAT SOME PEOPLE JUST… DON’T WANT TO WAKE UP?? THIS ISN’T A DISORDER - THIS IS ENTITLEMENT. GET A JOB. GET UP. STOP BLAMING YOUR GENES.