When your liver gets scarred from years of damage, it doesn’t just heal-it changes. Forever. That’s cirrhosis. It’s not a single disease. It’s the end result of long-term harm-whether from alcohol, hepatitis, or fat buildup-and it turns healthy liver tissue into stiff, useless scar tissue. By the time most people notice symptoms, the damage is already advanced. But here’s the thing: if you catch it early, you can still stop it from getting worse. And if it’s too far gone? A liver transplant can save your life.
What Actually Happens When Your Liver Gets Scarred
Your liver is tough. It can handle a lot-alcohol, meds, viruses-and still keep working. But when the damage keeps coming, it starts to rebuild itself the wrong way. Instead of growing back healthy cells, it lays down thick bands of scar tissue. This isn’t like a skin cut that heals clean. This scar tissue doesn’t work. It doesn’t filter toxins. It doesn’t make proteins. It doesn’t help digest food. Over time, these scars squeeze the blood vessels inside the liver. That raises pressure in the portal vein-the main blood highway coming from your gut. When that pressure climbs above 10 mmHg, you’ve got portal hypertension. That’s when things start going downhill fast: fluid builds up in your belly (ascites), veins in your esophagus swell and can burst, and your spleen gets enlarged. The liver tries to compensate. It forms little nodules of regenerating tissue, but they’re trapped in a web of scar. That’s what a biopsy shows: a patchwork of healthy-looking cells surrounded by fibrous bands. It looks like a cracked pavement. The liver still works-at first. That’s called compensated cirrhosis. You might feel fine. Maybe just tired. But your blood tests already tell a different story: low albumin, high bilirubin, low platelets, and a prolonged INR. These aren’t just numbers. They’re signs your liver is struggling.The Difference Between Compensated and Decompensated Cirrhosis
There’s a line in the sand between compensated and decompensated cirrhosis-and crossing it changes everything. In compensated cirrhosis, your liver is scarred, but it’s still doing enough to keep you alive. You might not even know you have it. Many people find out during a routine blood test or an ultrasound for something else. One patient in Bristol told me he only found out after his GP noticed his liver enzymes were up. He had no symptoms. No jaundice. No swelling. Just a silent, slowly failing organ. Decompensated cirrhosis is when the liver gives up. That’s when symptoms crash in: your belly swells with fluid, you get confused or forgetful (hepatic encephalopathy), you vomit blood from burst veins, or you get infections you can’t shake. At this stage, your 5-year survival drops from 80-90% to 20-50%. That’s not a guess. That’s from decades of tracking patients. The Child-Pugh score and MELD score are the tools doctors use to measure how bad it is. Child-Pugh looks at bilirubin, albumin, INR, ascites, and brain function. MELD uses bilirubin, creatinine, and INR to predict death risk without a transplant. A MELD score above 15 means you’re in serious danger. Above 25? You’re on the fast track to needing a liver.What Causes Cirrhosis? It’s Not Just Alcohol
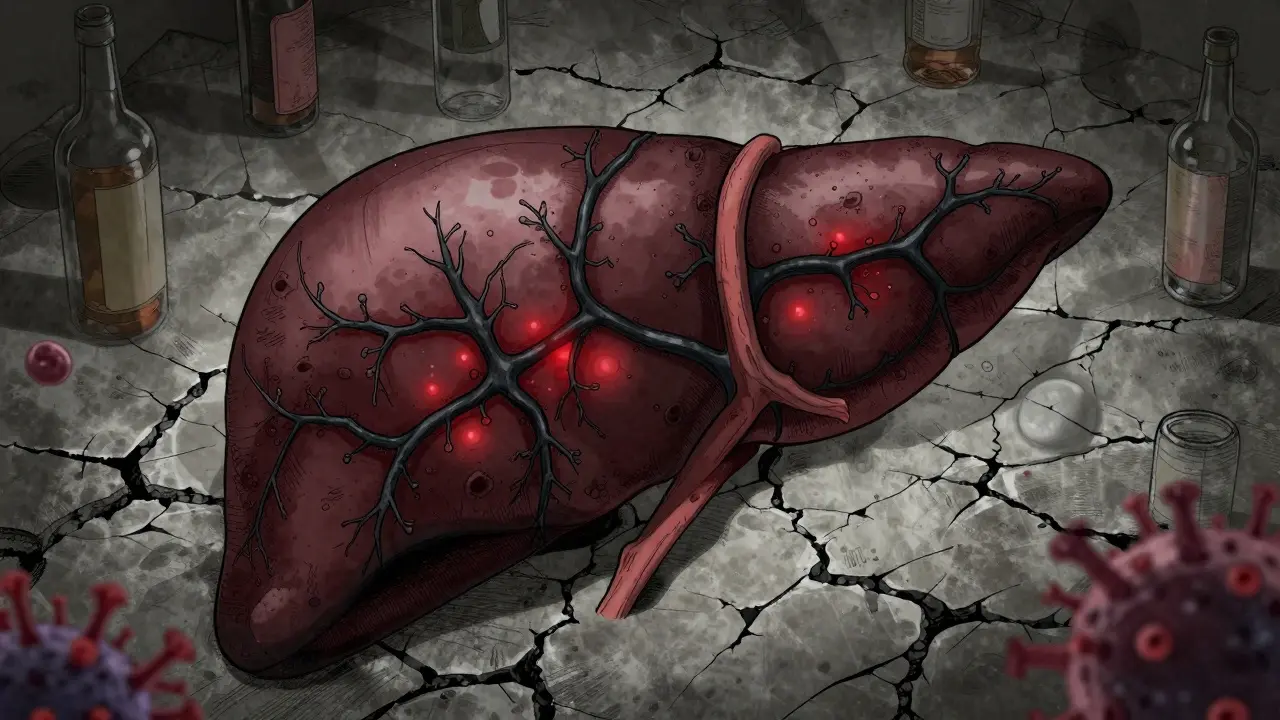
People still think cirrhosis only comes from drinking too much. That used to be true. But now? Non-alcoholic fatty liver disease (NAFLD) is the fastest-growing cause in the U.S. and the UK. About 24% of cirrhosis cases now come from fat buildup in the liver-often tied to obesity, diabetes, or high cholesterol. It’s silent. You don’t feel it until it’s too late. Hepatitis B and C are still big players. Hepatitis C, in particular, can hide for 20 years before causing serious damage. That’s why so many people are diagnosed in their 50s or 60s-they were infected decades ago and never knew. Other causes: autoimmune hepatitis, long-term bile duct blockage (like primary biliary cholangitis), genetic disorders like hemochromatosis (too much iron), or even certain medications. The cause matters because it changes your treatment. Stop drinking? You might stabilize. Treat hepatitis C? You might reverse early scarring. But once cirrhosis sets in, you can’t undo the scar tissue.
Can Cirrhosis Be Reversed?
Here’s the hard truth: once you’ve got cirrhosis, the scarring is permanent. No pill, no supplement, no detox can erase it. That’s why early detection is everything. Fibrosis-the early stage before cirrhosis-can sometimes be reversed. If you catch fatty liver disease early and lose weight, or treat hepatitis C with antivirals, your liver can heal. But once the scar tissue forms a network across the liver, it’s locked in. The liver can still function, but it can’t regenerate past the damage. That’s why doctors focus on stopping further harm. No more alcohol. Control your blood sugar. Get vaccinated for hepatitis A and B. Take prescribed meds like beta-blockers to lower portal pressure. Cut sodium to under 2,000 mg a day to keep fluid from pooling. These aren’t suggestions. They’re survival tools.Liver Transplant: The Only Real Cure
If your liver fails, a transplant is the only option that gives you back a normal life expectancy. It’s not a quick fix. It’s a major surgery with lifelong consequences. But for many, it’s the difference between dying in a year and living for 20 more. In the U.S., about 40% of all liver transplants are for cirrhosis. The waiting list is brutal. In 2022, there were 14,300 people waiting for a liver in the U.S. and only 8,780 transplants performed. That means about 12% of people on the list die each year before they get one. The MELD-Na score determines who gets priority. Higher score = higher risk of dying = higher on the list. It’s cold, but it’s fair. Your age, location, and blood type matter too. A 60-year-old with a MELD of 30 in London might wait longer than a 45-year-old with the same score in a smaller city. Post-transplant, you’ll need to take anti-rejection drugs for the rest of your life. You’ll be more prone to infections, kidney problems, and certain cancers. But you’ll also eat normally, walk without swelling, think clearly, and sleep through the night. Many patients say it’s like being reborn.What’s New in Cirrhosis Treatment?
The field is changing fast. Non-invasive tests like MRI elastography are replacing biopsies in many clinics. They measure liver stiffness with 90% accuracy-no needle needed. That means earlier diagnosis, fewer complications, and less fear for patients. New drugs are on the horizon. Obeticholic acid is already approved for some types of cirrhosis from bile duct disease. And in 2023, a drug called simtuzumab showed it could slow fibrosis progression in fatty liver-related cirrhosis by 30% in early trials. That’s not a cure, but it’s hope. Even transplants are improving. Machines that keep donor livers alive and beating outside the body (normothermic perfusion) are increasing the number of usable organs by 22%. That’s huge. And in labs, scientists are growing liver tissue from stem cells. The first human trials showed a 40% drop in MELD scores after six months. It’s early, but it’s real.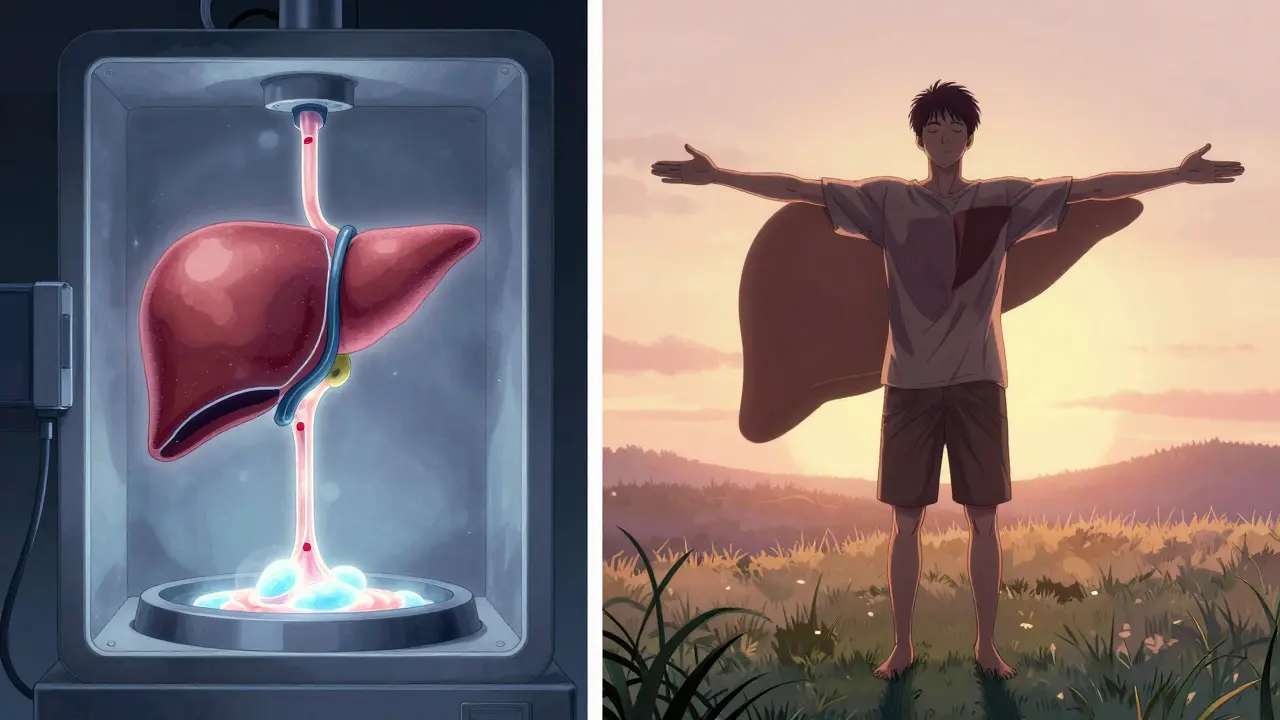
What Patients Wish They Knew Sooner
I’ve talked to dozens of people living with cirrhosis. The same things come up:- "I didn’t realize fatigue was a symptom. I thought I was just getting old."
- "No one explained the difference between compensated and decompensated until I was in the hospital with fluid in my lungs."
- "I was told to cut salt. I didn’t know how much was in bread, soup, or frozen meals."
- "My doctor didn’t mention transplant until I was on the verge of collapse."
Where to Get Help
You don’t have to figure this out alone. If you’re in the UK, your GP can refer you to a hepatologist. Most major hospitals now have liver clinics with teams of specialists: doctors, dietitians, addiction counselors, social workers. They’ll help you manage meds, diet, and mental health. The American Liver Foundation’s helpline (1-800-GO-LIVER) is a great resource, even if you’re overseas. They have free guides on low-sodium diets, coping with encephalopathy, and how to talk to your doctor about transplant. And if you’re thinking about transplant: start the conversation early. Even if you’re not ready, getting evaluated now puts you on the list. You can’t rush it, but you can prepare for it.Final Thought: It’s Not a Death Sentence-Yet
Cirrhosis isn’t a quick end. It’s a slow burn. But it’s also a call to act. Whether you’re in the early stage and still have time, or you’re already struggling with fluid and confusion, there are steps you can take. Stop the damage. Manage the symptoms. Prepare for the future. And if the worst happens? A transplant isn’t just a last resort. For many, it’s a second chance.Can cirrhosis be reversed naturally?
No, cirrhosis itself cannot be reversed once scar tissue has formed. However, if you catch liver damage early-before it becomes cirrhosis-you can stop or even reverse fibrosis by removing the cause (like quitting alcohol, treating hepatitis C, or losing weight). Once cirrhosis is diagnosed, treatment focuses on preventing further damage and managing complications, not undoing the scarring.
How do you know if you have cirrhosis?
Early cirrhosis often has no symptoms. Signs usually appear later: fatigue, swelling in the legs or belly, yellowing skin (jaundice), confusion, easy bruising, or red palms. Blood tests showing low albumin, high bilirubin, or low platelets can raise suspicion. Imaging like ultrasound, FibroScan, or MRI elastography can detect liver stiffness. A liver biopsy is the gold standard but is increasingly replaced by non-invasive tests.
What’s the life expectancy with cirrhosis?
It depends on the stage. With compensated cirrhosis, 80-90% of people live at least 5 years. Once it becomes decompensated-meaning symptoms like fluid buildup or confusion appear-survival drops to 20-50% over 5 years. The MELD score gives a more precise prediction: a score of 20-30 means about a 50% chance of dying within a year without a transplant.
Can you live a normal life with cirrhosis?
Yes-if it’s caught early and managed well. Many people with compensated cirrhosis live for years without major issues by avoiding alcohol, eating low-sodium diets, taking prescribed medications, and getting regular checkups. But once complications like ascites or encephalopathy develop, daily life becomes much harder. A liver transplant can restore near-normal function and quality of life.
How long is the wait for a liver transplant?
There’s no fixed wait time. It depends on your MELD-Na score, blood type, location, and organ availability. People with higher scores (above 25) usually get transplants within months. Those with lower scores may wait over a year. In the U.S., about 12% of people on the waiting list die each year before receiving a liver. Some centers use expanded criteria donors or machine-perfused livers to shorten wait times.
What are the biggest risks after a liver transplant?
The biggest risks are organ rejection and infection. You’ll need to take immunosuppressants for life, which lowers your body’s ability to fight germs. Other risks include kidney damage from meds, high blood pressure, diabetes, and certain cancers. About 70% of transplant recipients survive at least 5 years, and many live 20+ years with good quality of life if they follow their treatment plan closely.

Kat Peterson
January 23, 2026 AT 13:19Himanshu Singh
January 23, 2026 AT 21:51Jamie Hooper
January 24, 2026 AT 20:40Sawyer Vitela
January 25, 2026 AT 00:45Shanta Blank
January 26, 2026 AT 06:08Dolores Rider
January 27, 2026 AT 02:57Sharon Biggins
January 27, 2026 AT 20:55Michael Camilleri
January 29, 2026 AT 16:27