What CPAP and BiPAP Actually Do
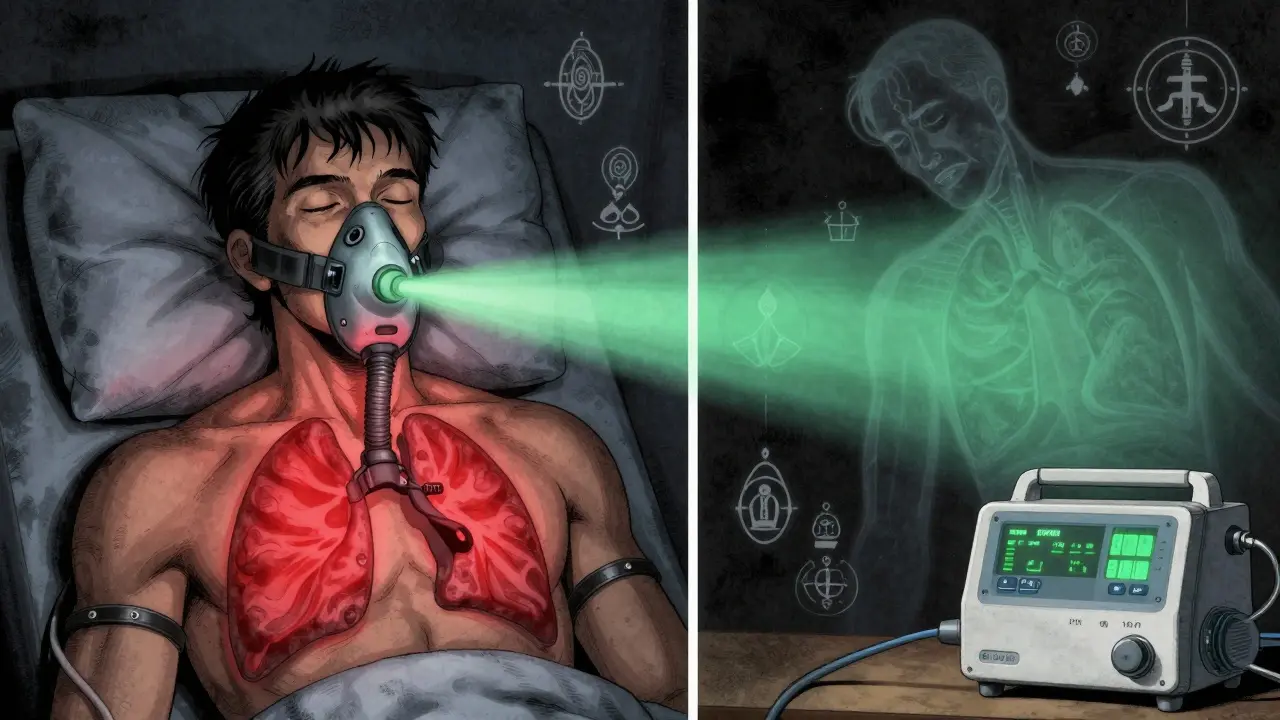
Both CPAP and BiPAP machines help you breathe better while you sleep. They push air through a mask to keep your airway open, stopping snoring and pauses in breathing. This is critical for people with sleep apnea, where the throat collapses during sleep and cuts off oxygen. The difference isn’t in the goal-it’s in how they do it.
CPAP delivers one steady pressure all night long. Think of it like a constant breeze holding your airway open. BiPAP, on the other hand, gives you two pressures: a higher one when you inhale (IPAP) and a lower one when you exhale (EPAP). That drop in pressure on the way out makes breathing feel less like fighting against a wall.
Neither device cures sleep apnea. They manage it. You still need to use them every night. Skip a few nights, and the snoring, gasping, and daytime fatigue come right back.
How the Pressure Settings Work
CPAP machines work with a single pressure setting, usually between 4 and 20 cm H₂O. That number is set after a sleep study, where technicians watch your breathing and find the lowest pressure that keeps your airway open. Most people end up between 8 and 12 cm H₂O.
BiPAP machines have two dials: one for inhalation pressure (IPAP), typically 8-30 cm H₂O, and one for exhalation pressure (EPAP), usually 4-25 cm H₂O. The difference between them-called the pressure support-must be at least 3 cm H₂O to work properly. So if your EPAP is set to 8, your IPAP might be 12 or 14. That 4-6 cm difference is what makes exhalation easier.
Modern BiPAP machines also have backup modes. If you stop breathing for more than 10-20 seconds, the machine will force a breath. That’s not just comfort-it’s safety. This feature matters for people with central sleep apnea, where the brain forgets to tell the lungs to breathe, or for those with weak respiratory muscles from conditions like ALS or COPD.
Who Gets CPAP and Who Gets BiPAP
For about 9 out of 10 people with obstructive sleep apnea (OSA), CPAP is the first and best choice. It’s simpler, cheaper, and just as effective at keeping the airway open. Studies show no big difference in how well people sleep or how much they use the machine between CPAP and BiPAP for standard OSA.
BiPAP is reserved for specific cases:
- High CPAP pressure needs: If you need more than 15 cm H₂O to stay open, exhaling against that pressure can feel suffocating. BiPAP’s lower exhalation setting makes it tolerable.
- COPD with high carbon dioxide: People with chronic lung disease often build up CO₂ in their blood. BiPAP helps them blow it out more easily.
- Central sleep apnea: This isn’t caused by a blocked airway-it’s when the brain doesn’t signal breathing. BiPAP’s backup breath feature saves lives here.
- Obesity hypoventilation syndrome: People with severe obesity (BMI over 30) and daytime drowsiness often need extra help exhaling. BiPAP gives it.
- Neuromuscular disorders: Conditions like Parkinson’s, ALS, or spinal cord injuries weaken breathing muscles. BiPAP steps in where the body can’t.
Doctors don’t pick BiPAP because it’s "better." They pick it because CPAP won’t work-or won’t be used-without it.
Cost, Insurance, and What You’ll Pay
CPAP machines cost between $500 and $1,200. Basic models from ResMed or Philips are often covered by insurance after a sleep study. Medicare and most private insurers pay for 80% of the cost if you meet usage requirements: at least 4 hours a night, 70% of nights, for 30 days.
BiPAP machines? They’re $800 to $1,800. Insurance won’t cover them unless you prove CPAP failed. That means you tried CPAP for at least 30 days, used it over 15 cm H₂O for 4 hours a night, and still couldn’t tolerate it. That’s a high bar. Many people give up on CPAP too soon because of mask leaks or dry mouth-not because the pressure is too high.
Don’t assume BiPAP is the "upgrade." It’s not. It’s a specialized tool. If your doctor suggests BiPAP without testing CPAP first, ask why. There’s a good chance they’re following outdated habits, not current guidelines.
Real User Experiences
On forums like Reddit’s r/CPAP, users who switched from CPAP to BiPAP often say things like: "I was on 14 cm H₂O and felt like I was drowning every time I exhaled. At 14/8 BiPAP, I actually slept." That’s not hype-it’s physics. Lowering exhalation pressure reduces the work of breathing by 30-40%.
But here’s the flip side: BiPAP is harder to use. One survey found 34% of BiPAP users struggled with machine settings, compared to 18% of CPAP users. The machine can sometimes misread your breathing, especially if you’re a light sleeper or breathe irregularly. That leads to "cycling issues"-where the machine switches pressure at the wrong time, making you feel like you’re gasping.
CPAP users report higher satisfaction with ease of use. 71% rate it as "excellent," versus 58% for BiPAP. Simplicity matters. If you’re not struggling with pressure, CPAP is the easier path.
What Happens After You Start
Getting used to either machine takes time. Most people need 2-4 weeks to adjust to CPAP. BiPAP? It can take 3-6 weeks. Why? More settings, more variables, more things that can go wrong.
Here’s what works:
- Mask fit: 70% of early problems come from a bad seal. Try different styles-nasal pillows, full face, hybrid. Don’t stick with the first one.
- Humidification: Dry mouth and nose are common. Turn up the heat on your humidifier. Many machines now auto-adjust humidity based on room conditions.
- Pressure ramp: Both devices let you start at a lower pressure and slowly increase over 10-45 minutes. Use it. Falling asleep with full pressure is hard.
- Follow-up: Don’t wait until you’re miserable to call your provider. Schedule a check-in at 2 weeks. They can tweak pressure, mask, or settings before you quit.
BiPAP users often need more help. A respiratory therapist should be involved in setup, especially if you’re on a backup mode. CPAP? Most people can manage with a good video guide and a phone call to customer service.

What’s New in 2026
Devices today aren’t just air pumps. ResMed’s AirCurve 10 VAuto and Philips’ DreamStation 3 use AI to read your breathing in real time and adjust pressure automatically. Some can even track your blood oxygen levels overnight without a separate sensor.
But here’s the catch: these features don’t make BiPAP better for simple sleep apnea. They just make it smarter. The core issue remains: if you don’t need two pressures, you don’t need BiPAP.
Manufacturers are pushing BiPAP harder now because the market for simple CPAP is slowing. But clinical evidence hasn’t changed. BiPAP’s growth is driven by aging populations with complex conditions-not by better outcomes for standard OSA.
Bottom Line: Don’t Overcomplicate It
Most people with sleep apnea do fine with CPAP. It’s proven, affordable, and effective. BiPAP isn’t a "premium version." It’s a medical tool for specific problems. If you’re on CPAP and it’s working-don’t switch. If you’re struggling with high pressure, gasping on exhale, or have another condition like COPD, then BiPAP might be the answer.
Ask your doctor: "Why BiPAP? What’s wrong with CPAP for me?" If they can’t give you a clear reason based on your diagnosis, get a second opinion. Sleep therapy isn’t one-size-fits-all. But it also doesn’t need to be over-engineered.
What to Do Next
If you’ve been diagnosed with sleep apnea:
- Start with CPAP unless your doctor has a strong clinical reason not to.
- Use it every night. Even 4 hours helps. More is better.
- If you can’t tolerate CPAP after 30 days, talk about BiPAP-not as a default, but as a next step.
- Get a follow-up sleep study if you’re still tired. Sometimes the pressure is wrong, not the machine.
- Don’t buy a machine online without a prescription. Settings matter. Wrong pressure can hurt more than help.
Good sleep isn’t about the fanciest device. It’s about finding the one that lets you breathe-and stay asleep-without fighting it.


Alvin Bregman
January 14, 2026 AT 10:33Sarah -Jane Vincent
January 16, 2026 AT 02:16Andrew Freeman
January 16, 2026 AT 18:41says haze
January 17, 2026 AT 03:06Anna Hunger
January 17, 2026 AT 20:59Jason Yan
January 18, 2026 AT 19:16shiv singh
January 19, 2026 AT 19:21Robert Way
January 20, 2026 AT 10:33Sarah Triphahn
January 20, 2026 AT 16:50Vicky Zhang
January 21, 2026 AT 13:32Allison Deming
January 22, 2026 AT 06:28Susie Deer
January 23, 2026 AT 01:16TooAfraid ToSay
January 24, 2026 AT 16:40