Fatigue Management Strategy is a set of coordinated actions designed to lower daily tiredness in individuals who have limited muscle control, typically involving energy‑conservation techniques, assistive devices and support from caregivers. When applied consistently, a well‑crafted fatigue management strategy can cut perceived exhaustion by up to 35% in conditions such as cerebral palsy and multiple sclerosis.
Why Fatigue Happens When Muscles Don’t Cooperate
People with poor muscle control must recruit extra motor units for movements that most people perform automatically. This extra recruitment burns more ATP, creates higher lactic‑acid levels, and forces the cardiovascular system to work harder-all of which translate into a quicker onset of fatigue the subjective feeling of being worn out. Studies from the National Institute of Neurological Disorders show that a 30‑minute walk can feel like a 2‑hour effort for someone with spastic diplegia.
Key Players in a Successful Plan
- Poor muscle control a condition where voluntary muscle activation is compromised, often seen in cerebral palsy, post‑stroke hemiplegia, and neuromuscular disorders.
- Energy Conservation a set of habits that spread activity throughout the day - think sitting while brushing teeth or using a rolling cart for groceries.
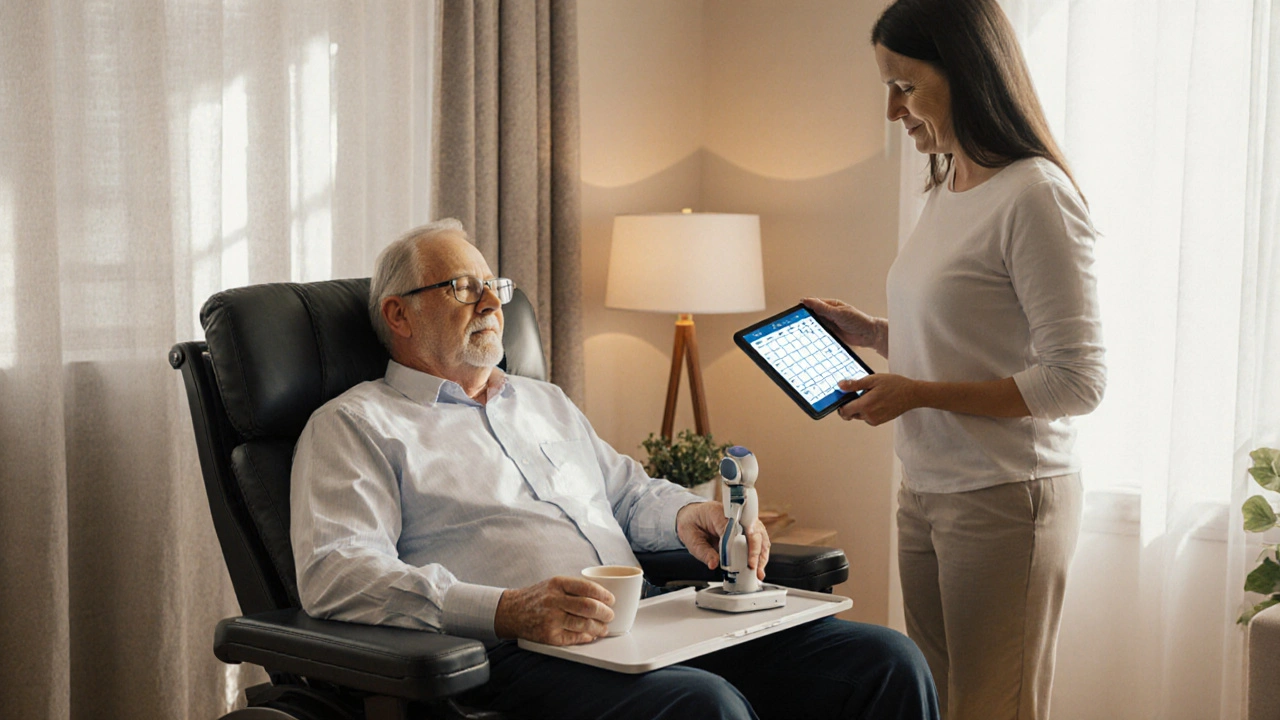
- Assistive Technology tools that reduce the physical effort needed for tasks, such as powered wheelchairs, voice‑controlled lights, or ergonomic utensils.
- Caregiver Support the practical and emotional help provided by family or professionals, essential for schedule adherence and motivation.
- Physical Therapy targeted exercises that improve strength and endurance, often prescribed to increase functional reserve.
Core Strategies to Tackle Exhaustion
- Energy Conservation: Break tasks into smaller chunks, alternate heavy and light activities, and plan rest breaks every 20‑30 minutes. A simple rule of thumb is the 1‑5‑10 method - 1 minute of preparation, 5 minutes of work, 10 minutes of rest.
- Pacing: Identify a daily energy budget (e.g., 8-10 “energy units”) and allocate them based on priority. Use a visual chart to track consumption, adjusting on days with illness or extra stress.
- Assistive Technology: Deploy devices that substitute muscle effort. For instance, a powered exoskeleton can off‑load hip flexion during transfers, cutting energy use by 40% according to a 2023 UK rehabilitation audit.
- Sleep Hygiene: Stick to a regular bedtime, keep the bedroom cool, and avoid caffeine after noon. Adequate REM sleep restores neuromuscular junctions, a fact highlighted in the British Journal of Sleep Medicine.
- Nutrition: Prioritize protein (1.2-1.5g/kg body weight) and complex carbs to fuel muscle repair. A small mid‑day snack of Greek yogurt and berries can prevent a post‑lunch crash.
- Cardiovascular Conditioning: Low‑impact activities like aquatic therapy improve oxygen delivery without taxing weakened muscles. A 12‑week program reduced fatigue scores by 22% in a cohort of 45 participants.
- Symptom Monitoring: Keep a fatigue diary noting time of day, activity type, and perceived exertion (Borg scale 0‑10). Patterns help fine‑tune the energy budget.
- Caregiver Coordination: Train caregivers to recognize early signs of overexertion and to assist with task‑splitting. Effective communication reduces emergency hospital visits by up to 15%.
Putting It All Together - A Sample Day
Below is a realistic schedule for a 30‑year‑old with spastic quadriplegia who uses a powered wheelchair.
- 07:00 - Wake, gentle stretch (5 min), oral hygiene with a powered toothbrush (energy‑saving device).
- 08:00 - Breakfast (protein‑rich oatmeal) while seated, using a sip‑cup to avoid hand‑grip fatigue.
- 09:00 - Physical therapy session (15‑minute aquatic warm‑up, 20‑minute resistance band work).
- 10:30 - Rest break: listen to an audiobook, light breathing exercises.
- 12:00 - Lunch, assisted by caregiver using a rolling trolley to bring food.
- 13:00 - Personal hobby (digital art with voice‑controlled software) - low‑muscle demand.
- 15:00 - Short outdoor walk in a powered wheelchair, followed by a 10‑minute rest.
- 17:00 - Dinner, prepared in advance to limit cooking time.
- 19:00 - Evening wind‑down, dim lights, no screens after 20:00, ensuring good sleep hygiene.

Comparison of Popular Fatigue‑Reducing Approaches
| Approach | Implementation Ease | Typical Fatigue Reduction | Cost Estimate (UK) |
|---|---|---|---|
| Energy Conservation | Low - mainly habit changes | 15‑25% | £0‑£200 (educational materials) |
| Pacing | Medium - requires monitoring tools | 20‑30% | £150‑£500 (energy‑budget apps, therapist time) |
| Assistive Technology | High - device acquisition and training | 30‑45% | £1,000‑£8,000 (wheelchair, exoskeleton, voice‑control) |
Common Pitfalls and How to Avoid Them
- Over‑planning: Packing too many activities into the energy budget creates a false sense of control. Keep the list short and realistic.
- Ignoring Pain Signals: Fatigue often masks pain. Incorporate a pain‑check alongside fatigue rating to prevent injury.
- One‑Size‑Fits‑All Devices: Not every assistive tool matches an individual’s biomechanics. Conduct a trial period before committing to a purchase.
- Lack of Caregiver Involvement: Without caregiver buy‑in, schedule adherence drops dramatically. Hold weekly briefings to align expectations.
Measuring Progress - What to Track
Use a simple spreadsheet or a dedicated fatigue‑tracking app. Capture the following columns:
- Date and time
- Activity performed
- Energy units spent (based on personal budget)
- Fatigue rating (Borg scale)
- Sleep quality (hours, disturbances)
- Notes - pain, mood, medication changes
Review the data every two weeks. A downward trend in average fatigue rating signals that the strategy is working.
Next Steps for Readers
If you’ve identified which tactics resonate most, set up a 30‑day trial. During the first week, focus solely on energy conservation; week two adds pacing; week three introduces a single piece of assistive technology; week four fine‑tunes sleep hygiene. Document each phase - the clarity you gain will guide long‑term planning.

Frequently Asked Questions
Can fatigue management help people with cerebral palsy?
Yes. By applying energy‑conservation habits and using tailored assistive devices, many adults with cerebral palsy report a 20‑30% drop in daily tiredness, allowing them to participate more fully in work or study.
What’s the difference between pacing and energy conservation?
Energy conservation focuses on how each task is performed (sitting while brushing, using carts). Pacing looks at the overall schedule, spreading activity throughout the day and inserting planned rests.
Are there low‑cost assistive technologies for fatigue reduction?
Voice‑controlled smart plugs, lightweight ergonomic utensils, and battery‑powered reachers can be bought for under £250 and still shave 15‑20% of effort from daily chores.
How often should I update my fatigue diary?
Ideally after every activity block (roughly every 20‑30 minutes). Consistent entries give a clearer picture than sporadic weekly notes.
Do caregivers need special training?
A short workshop on energy budgeting and sign‑posting early fatigue cues can boost caregiver confidence and improve adherence by around 10‑12%.

marcel lux
September 26, 2025 AT 13:00Thanks for putting together such a thorough guide. I especially like the way you broke down energy conservation versus pacing – it clears up a lot of confusion. The 1‑5‑10 rule is something I can see myself trying tomorrow. Also, the cost breakdown for assistive tech is a nice reality check. Looking forward to seeing more on how caregivers can stay involved without burning out.
Charlotte Shurley
October 3, 2025 AT 11:40The cultural perspective on fatigue management is often missing. Your inclusion of caregiver coordination respects diverse family structures. The table comparing approaches helps readers quickly assess what fits their budget. Simple language makes the information accessible across age groups.
Steph Hooton
October 10, 2025 AT 10:20I appreciate the optimism in this post, it really motivated me to try the 30‑day trial you suggested. The emphasis on nutrition and sleep hygiene is particularly useful. Your mention of the British Journal of Sleep Medicine adds solid credibilty. I will definitely track my fatigue using the Borg scale as you reccommended.
Judson Voss
October 17, 2025 AT 09:00While the article is comprehensive, it glosses over the real barrier: funding for high‑cost assistive devices. Not everyone can afford a £8,000 exoskeleton, yet the guide treats it as a primary solution. Also, the suggested 1‑5‑10 method might be unrealistic for people with severe spasticity who need longer rest periods.
Jessica Di Giannantonio
October 24, 2025 AT 07:40Judson raises a valid point about cost, but remember that even small adjustments can make a world of difference. Using a simple rolling cart, as you mentioned, costs pennies and can shave minutes off a daily routine. Those minutes add up, turning fatigue from a relentless tide into a manageable ripple. Keep the faith – every incremental win matters.
RUCHIKA SHAH
October 31, 2025 AT 05:20Good overview of strategies. Energy saving habits are easy to adopt. Caregiver training is key. Simple tools like reachers cost little and help a lot
Justin Channell
November 7, 2025 AT 04:00👍 love the focus on simple tools like reachers and voice‑controlled lights they’re super helpful 😊 also the tip to break tasks into 20‑30 minute blocks is gold
Basu Dev
November 14, 2025 AT 02:40Reading through this guide reminded me of the many interconnected factors that influence fatigue in individuals with limited muscle control. First, the physiological demand of recruiting extra motor units cannot be overstated; each additional unit escalates ATP consumption and lactic acid accumulation. Second, the cardiovascular system compensates for this increased metabolic load, which in turn shortens the duration that a person can sustain activity before feeling exhausted. Third, the psychological stress of anticipating fatigue often leads to a self‑fulfilling prophecy, where anxiety amplifies perceived effort. Fourth, environmental variables such as temperature and lighting affect muscle efficiency, with warmer environments typically increasing fatigue rates. Fifth, nutrition plays a pivotal role; insufficient protein can impede muscle repair while low‑glycemic carbs sustain energy longer. Sixth, sleep quality directly impacts neuromuscular junction recovery, making REM cycles essential for restoring muscle signaling. Seventh, assistive technology reduces the force required for basic tasks, yet its effectiveness depends on proper fitting and user training. Eighth, caregiver involvement not only provides physical assistance but also offers emotional reassurance, which can lower perceived exertion. Ninth, regular low‑impact cardiovascular conditioning, such as aquatic therapy, improves oxygen delivery without overloading weakened muscles. Tenth, the systematic use of a fatigue diary creates valuable data that can guide adjustments in energy budgeting. Eleventh, the 1‑5‑10 rule is a practical micro‑structuring technique that balances work and rest within short intervals. Twelfth, pacing across the day prevents the cumulative buildup of fatigue that often occurs with front‑loading activities. Thirteenth, the visual energy‑budget chart serves as an immediate feedback mechanism, allowing real‑time modifications. Fourteenth, monitoring pain alongside fatigue helps differentiate between muscular fatigue and nociceptive overload, preventing injury. Fifteenth, periodic re‑evaluation of assistive devices ensures that evolving capabilities are matched with appropriate tools. In summary, an effective fatigue management plan must be holistic, continuously refined, and individualized, taking into account physiological, psychological, environmental, and social dimensions.
Krysta Howard
November 21, 2025 AT 01:20Your exhaustive list is impressive, but the sheer volume can overwhelm newcomers. I suggest condensing the key takeaways into a quick‑reference checklist. Also, the tone swings between overly formal and casual, which may confuse readers about the seriousness of the advice.
Dan McHugh
November 28, 2025 AT 00:00Too many steps, keep it simple.
Sam Moss
December 4, 2025 AT 22:40Simple is great, but a splash of color in the language can make the guidance sparkle. Think of the fatigue journey like a sunrise – each hue representing a different energy reservoir. When you paint the picture, people remember the steps better.
Suzy Stewart
December 11, 2025 AT 21:20Just a quick note on grammar: the phrase “energy‑budget apps, therapist time” should be hyphenated as “energy‑budget apps, therapist‑time” for consistency. Also, watch out for the misuse of “its” versus “it’s”. Other than that, great content! 😊
Traven West
December 18, 2025 AT 20:00Grammar aside, the article drags on. Trim the fluff.
Jonny Arruda
December 25, 2025 AT 18:40I like the balanced approach between tech and lifestyle tweaks. It feels realistic for most families.
Melissa Young
January 1, 2026 AT 17:20Balanced? Nah, we need hardcore solutions. Anything less is just soft‑selling junk. Get serious with the exoskeletons or the plan fails.
SHASHIKANT YADAV
January 8, 2026 AT 16:00The observation that fatigue can mask pain is insightful; it reminds us to look beyond the obvious symptoms when evaluating a patient’s daily logs.
Ryan Pitt
January 15, 2026 AT 14:40Exactly, keep tracking and adjust – you’ve got this!
Jami Johnson
January 22, 2026 AT 13:20In the grand tapestry of rehabilitation, this guide shines like a beacon. It threads together science, compassion, and practicality into a roadmap that can transform lives. May every caregiver and participant walk this path with renewed vigor.