When you pick up a prescription, you might not notice the thick black border on the drug label. But that border isn’t just for decoration-it’s the FDA’s strongest possible warning that this medicine could kill you or cause life-changing harm. These are called black box warnings, and they’re the highest level of safety alert the U.S. Food and Drug Administration can issue. Over 400 prescription drugs carry one right now, including some of the most commonly used medications for depression, diabetes, pain, and heart conditions.
What Exactly Is a Black Box Warning?
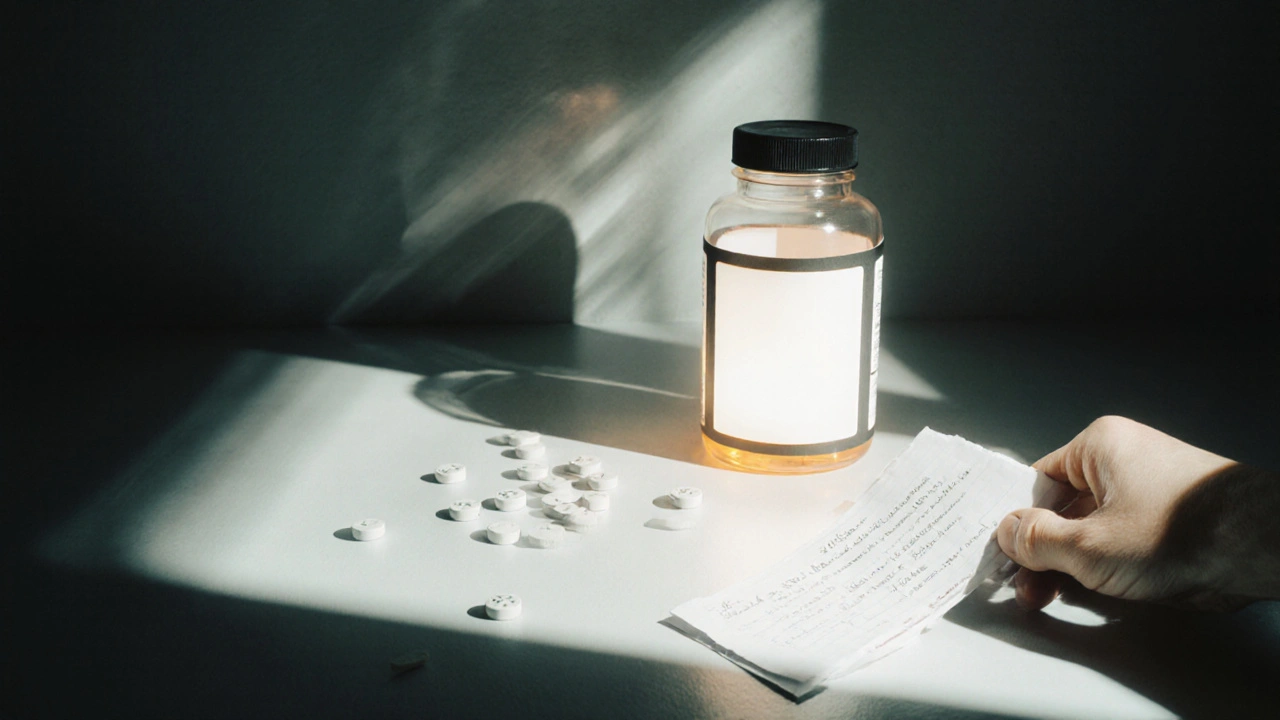
A black box warning isn’t a suggestion. It’s a legal requirement. The FDA mandates that drugmakers place this warning right at the front of the prescribing information, enclosed in a thick black border so doctors and patients can’t miss it. It’s not buried in fine print. It’s not tucked away in a footnote. It’s front and center because the risks it describes are serious enough to outweigh the benefits for some people. These warnings don’t talk about mild side effects like nausea or dizziness. They flag dangers that can lead to death, organ failure, suicidal behavior, severe infections, or irreversible damage. For example, some antidepressants carry a black box warning for increased suicide risk in young adults. Certain painkillers warn of fatal respiratory depression. Diabetes drugs may carry warnings about heart failure. These aren’t rare outliers-they’re well-documented, statistically significant risks that the FDA has confirmed through years of patient data.How Does the FDA Decide to Add a Black Box Warning?
Most black box warnings aren’t added before a drug hits the market. They’re added after. That’s because some dangers only show up when thousands or millions of people start using the drug over time. The FDA tracks these risks through the MedWatch program, where doctors, pharmacists, and even patients report side effects. Every year, the agency reviews about 1.3 million of these reports. If a pattern emerges-like a spike in liver failure among users of a certain drug, or a cluster of heart attacks in people taking a new weight-loss pill-the FDA investigates. They dig into clinical trial data, hospital records, and death certificates. If the evidence shows the risk is real, severe, and preventable with better use, they require a black box warning. Sometimes, the warning comes with extra rules. For drugs with extreme risks, the FDA adds a Risk Evaluation and Mitigation Strategy (REMS). This might mean only certified doctors can prescribe it, patients must sign a consent form, or the drug can only be dispensed through special pharmacies. These aren’t just paperwork-they’re safety nets.Common Drugs With Black Box Warnings
You might be surprised how many everyday medications carry these warnings. Here are a few real examples:- Fluoxetine (Prozac) and other SSRIs: Increased risk of suicidal thoughts in people under 25.
- Avandia (rosiglitazone): Higher risk of heart attack and heart failure.
- Depo-Provera: Possible bone density loss with long-term use.
- Valproate: Can cause severe liver damage and birth defects-strictly avoided in pregnant women.
- Insulin glargine (Lantus): May increase cancer risk in some patients (based on observational data).
Does a Black Box Warning Mean You Should Avoid the Drug?
No. And that’s the biggest misunderstanding. A black box warning doesn’t equal a ban. It means the drug is powerful-and dangerous if used carelessly. Take the case of antidepressants. For a teenager with severe depression, the risk of suicide without treatment is far higher than the risk from the medication. The warning doesn’t stop doctors from prescribing-it just forces them to have a real conversation. They’ll ask: Are you having thoughts of self-harm? Are you being monitored? Are there other options? The same goes for drugs like biologics used to treat rheumatoid arthritis or Crohn’s disease. They carry warnings about serious infections, including tuberculosis and fungal diseases. But for many patients, these drugs are the only thing keeping them out of a wheelchair or off a feeding tube. The key isn’t avoiding the drug-it’s understanding your personal risk. Are you older? Do you have liver disease? Are you taking other medications that interact? Your doctor should walk you through this.What Should You Do If Your Medication Has a Black Box Warning?
If you’re on a drug with a black box warning, don’t panic. Don’t stop taking it cold turkey. Do this:- Read the warning. Don’t just glance at it. Read exactly what it says. Is it about liver damage? Heart failure? Suicide risk? Know the exact threat.
- Ask your doctor: "What’s the specific risk for me?" and "What signs should I watch for?"
- Ask about alternatives. Is there another drug without the warning that works just as well? Sometimes yes. Sometimes no.
- Know your monitoring plan. Some drugs require blood tests every month. Others need EKGs or liver scans. Don’t skip them.
- Report side effects. If you feel something’s wrong-fatigue, confusion, chest pain, mood changes-tell your doctor immediately. You can also report it directly to the FDA through MedWatch.

Why Don’t More Patients Talk About These Warnings?
Studies show that even when a drug has a black box warning, doctors often don’t bring it up. Patients rarely ask. It’s uncomfortable. People assume if the doctor prescribed it, it’s safe. But safety isn’t about approval-it’s about awareness. One study found that after the black box warning for rosiglitazone (Avandia), prescriptions dropped by 70%. But 3.8 million people still took it. Why? Because for many, the benefit-controlling diabetes-was worth the risk. The warning didn’t stop use. It just made it more intentional. The same thing happened with opioid painkillers. Black box warnings about addiction and overdose didn’t eliminate prescriptions-but they did push doctors to think twice before writing them.What’s Changing in the Future?
The FDA is moving toward smarter warnings. Instead of saying "this drug can cause liver damage," future labels might say: "This drug can cause liver damage in people with the HLA-B*57:01 gene variant." That’s pharmacogenomics-using your DNA to predict risk. They’re also testing digital labels. Imagine your doctor clicks a button to prescribe a drug, and a pop-up says: "Patient is 72, on blood thinners, has kidney disease. This drug carries a black box warning for kidney failure in this group. Consider alternative." These aren’t sci-fi ideas-they’re in development right now. The goal is to make warnings more personal, not just louder.Final Thought: Knowledge Is the Safest Medicine
Black box warnings aren’t meant to scare you. They’re meant to empower you. They exist because the FDA learned the hard way that silence kills. A patient who doesn’t know their drug can cause heart failure might ignore chest pain and wait too long to call for help. A doctor who doesn’t know the warning exists might prescribe it without checking liver function. The warning doesn’t change the drug. It changes how you use it. If you’re on a medication with a black box warning, you’re not taking a gamble. You’re making a calculated choice-with full information. That’s exactly how it should be.Are black box warnings only for prescription drugs?
Yes. Black box warnings only apply to prescription medications approved by the FDA. Over-the-counter drugs, supplements, and vitamins don’t carry these warnings because they don’t go through the same rigorous review process. However, some OTC drugs have strong warnings on the label-just not in a black box.
Can a black box warning be removed?
Yes, but it’s rare. The FDA will remove a black box warning only if new evidence proves the risk is much lower than originally thought-or if better safety measures (like monitoring or genetic testing) make the drug safe for broader use. For example, some older warnings about birth control pills were removed after decades of data showed lower risks than initially feared.
Do all doctors know about black box warnings?
Most do, especially specialists. But primary care doctors, who prescribe the majority of medications, may not always recall every warning for every drug. That’s why it’s your job to ask. Bring the warning label with you to appointments. Say: "This drug has a black box warning. Can we talk about what that means for me?"
Can I get a drug with a black box warning if I’m pregnant?
Sometimes, but only if the benefit clearly outweighs the risk. Many black box warnings specifically say the drug is contraindicated in pregnancy-for example, drugs that cause birth defects like valproate. In other cases, like certain antidepressants, the risk of untreated depression may be greater than the risk of the medication. This decision requires careful discussion with your OB-GYN and psychiatrist.
Where can I find a complete list of drugs with black box warnings?
The FDA’s official Drugs@FDA database lists every approved drug and its current labeling, including black box warnings. You can search by drug name or condition. Many reputable pharmacy websites like MedlinePlus and GoodRx also pull this data directly from the FDA. Avoid third-party blogs or forums-they may be outdated or inaccurate.

LINDA PUSPITASARI
November 29, 2025 AT 20:47Just found out my antidepressant has a black box warning 😳 I’ve been on it for 3 years and never read the fine print. Thanks for the wake-up call. I’m scheduling a chat with my doc this week. Never underestimate the power of a black border.
gerardo beaudoin
November 30, 2025 AT 18:11Yeah this is spot on. I work in a pharmacy and people freak out when they see the black box. But half the time they’re already on the med and just need to know what to watch for. Knowledge is power, not panic.
Brandy Johnson
November 30, 2025 AT 22:41It is an absolute disgrace that the FDA allows such dangerous substances to remain on the market under the guise of "treatment." This is corporate medicine at its most predatory. Patients are being treated like lab rats while shareholders profit.
Monica Lindsey
December 2, 2025 AT 00:27Wow. So you’re telling me people don’t read the warnings? Shocking. Truly. I mean, if you can’t be bothered to read a black box, maybe you shouldn’t be allowed to take pills at all.
stephen idiado
December 3, 2025 AT 21:07Black box? More like black propaganda. Big Pharma funds the FDA. These warnings are theater. The real danger is the system that lets them profit off your fear.
Subhash Singh
December 5, 2025 AT 04:40It is indeed a commendable initiative by the FDA to enforce such stringent labeling protocols. However, the efficacy of these warnings is contingent upon physician-patient communication, which remains inconsistent across socioeconomic strata.
Geoff Heredia
December 5, 2025 AT 18:21Wait… what if the black box isn’t about the drug… but about the cover-up? I’ve heard the FDA gets pressured by lobbyists. That warning? It’s a distraction. The real danger is the surveillance state tracking your meds through your insurance. They know everything.
Andrew Keh
December 6, 2025 AT 21:49Good breakdown. I think the key takeaway is that black box warnings aren’t meant to scare people off-they’re meant to make sure the decision to use the drug is informed. That’s just good medicine.
Peter Lubem Ause
December 7, 2025 AT 12:56Let me tell you something, folks. I’ve seen patients on these drugs turn their lives around. One guy I know was on insulin glargine, had the warning, but he lost 80 pounds, got off dialysis, and now coaches kids in basketball. The warning didn’t stop him-it gave him the tools to be safe while he fought. Don’t let fear silence your hope. Talk to your doctor, get tested, stay alert. You’ve got this.
Joy Aniekwe
December 9, 2025 AT 01:45Oh wow, so now I’m supposed to trust a system that gave us opioids and fen-phen? Thanks, but I’ll just keep my vitamins and my skepticism.
Latika Gupta
December 9, 2025 AT 07:31My mom is on Depo-Provera. I just looked it up. Bone loss? That’s… that’s not okay. I’m calling her doctor tomorrow. I didn’t even know she was on it. I’m so sorry I didn’t ask sooner.
Sullivan Lauer
December 11, 2025 AT 04:49THIS. RIGHT. HERE. I had a cousin die from liver failure on valproate. No one told her family the risk was higher if you’re under 30 and female. They just handed her the script. The black box? It’s not a warning-it’s a funeral notice waiting to be read. If you’re on one of these, don’t just take it-research it, question it, demand answers. Your life isn’t a footnote.
Sohini Majumder
December 11, 2025 AT 23:36so like… black box = big scary letters? but like… why do they even bother if like… nobody reads them? also why is it called a "box" like it’s a gift??
tushar makwana
December 12, 2025 AT 09:54in india we don't have these warnings much, but my sister took a drug for epilepsy and she had a bad reaction. we didn't know. now i tell everyone to always ask: "what's the worst that can happen?" simple question. big answer.
Matthew Higgins
December 12, 2025 AT 21:38Been on an SSRI with the black box for 5 years. Never had an issue. But I do monthly bloodwork and tell my therapist everything. It’s not about fear-it’s about being smart. This post? Perfect. Thanks for not being alarmist.