Glaucoma doesn’t always cause symptoms until it’s too late. That’s why managing eye pressure with medication is often the first and most important step in stopping vision loss. Two main classes of drugs - prostaglandins and beta blockers - are used as first-line treatments for primary open-angle glaucoma. But they work differently, have different side effects, and affect your life in very different ways. Choosing between them isn’t just about which lowers pressure more. It’s about what you can stick with, what your body tolerates, and what risks you’re willing to accept.
How Prostaglandins Work and Why They’re First-Line
Prostaglandin analogs - like latanoprost, bimatoprost, and travoprost - are the most prescribed glaucoma meds today. They don’t reduce fluid production in the eye. Instead, they open up a different drainage path called the uveoscleral route. This lets fluid escape more easily, lowering pressure inside the eye. Latanoprost, first approved in 1996, set the standard. Today, it’s still the most used.
These drugs are effective. Most people see a 24% to 33% drop in eye pressure from baseline. That’s better than most other classes. And because they’re taken just once a day - usually at night - they’re easier to remember. Studies show people stick with prostaglandins longer. One 2019 study found that 39% of users were still taking their prostaglandin after a year, compared to only 25% of those on beta blockers. That’s a big deal. If you miss doses, pressure rises, and damage continues.
But there’s a catch. These drugs cause real, visible changes. About 5% to 10% of long-term users develop darker iris color - permanent. Eyelashes get longer, thicker, and darker. Some people like this. Others find it unsettling. And about 30% to 50% notice redness in the whites of their eyes, especially at first. It’s not dangerous, but it can make you self-conscious.
Beta Blockers: Effective, But With Hidden Risks
Beta blockers like timolol and betaxolol work the opposite way. They slow down how much fluid your eye makes. Timolol 0.5% drops typically reduce pressure by 20% to 25%. That’s solid - just a little less than prostaglandins. But here’s the problem: they’re absorbed into your bloodstream. That means they don’t just affect your eye.
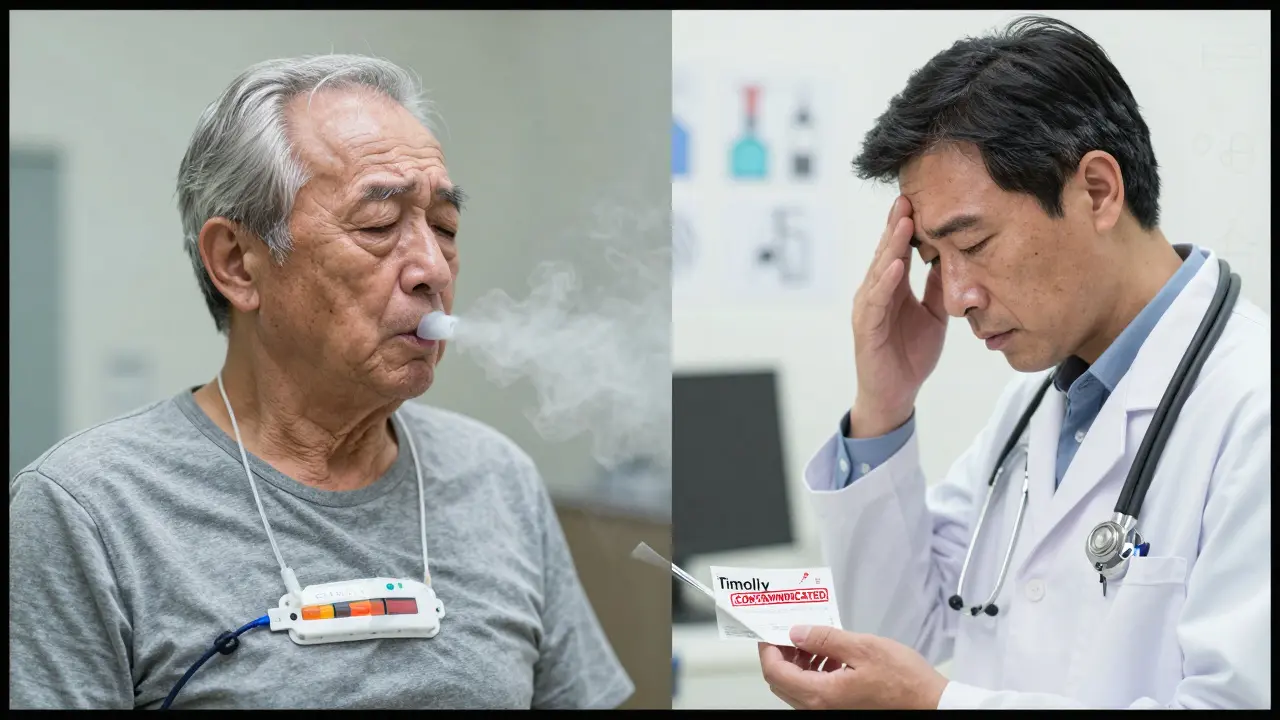
If you have asthma, COPD, or heart problems, beta blockers can be dangerous. They can trigger wheezing, slow your heart rate, or even cause low blood pressure. That’s why doctors screen for these conditions before prescribing them. The FDA even requires a black box warning on timolol for these risks. Fatigue and dizziness are common side effects, reported by 15% to 20% of users.
They also require two doses a day - morning and night. That doubles the chance you’ll forget one. And while they’re cheaper than prostaglandins, the cost isn’t the main issue. It’s the safety. For a healthy 45-year-old, timolol might be fine. For a 72-year-old with a pacemaker or emphysema? It’s a bad fit.
Comparing the Two: Efficacy, Side Effects, and Real-World Use
Here’s the truth: neither drug is clearly better at saving your vision. A seven-year study published in 2013 looked at visual field changes in patients on either prostaglandins or beta blockers. The results? No significant difference. Both worked equally well over time. So the choice isn’t about which protects sight more. It’s about which you can live with.
Let’s break it down:
| Feature | Prostaglandins (e.g., latanoprost) | Beta Blockers (e.g., timolol) |
|---|---|---|
| How it works | Increases fluid drainage | Reduces fluid production |
| Dosing | Once daily (night) | Twice daily |
| IOP reduction | 24-33% | 20-25% |
| Common side effects | Red eyes, longer eyelashes, darker iris | Fatigue, breathing trouble, slow heart rate |
| Systemic risks | Very low | High - asthma, heart disease |
| Persistence rate (12 months) | 39% | 25% |
| Preservative-free options | Available | Available |
One thing to note: bimatoprost lowers pressure slightly more than latanoprost - about 1 to 2 mm Hg more at certain times. But it also causes more burning and stinging. About 25% to 30% of users report irritation, compared to 15% to 20% with latanoprost. That’s why many doctors start with latanoprost. It’s the sweet spot between effectiveness and tolerability.
Safety First: What No One Tells You
Most patients focus on whether the drops work. Few ask about what happens after years of use. That’s where safety gets complicated.
Prostaglandins are generally safe for the body, but they can harm the eye’s surface over time - especially if they contain preservatives. Benzalkonium chloride (BAK) is used in most formulations to keep them sterile. But it’s harsh. A 2021 meta-analysis showed that preservative-free versions improved tear film quality and reduced dry eye symptoms. The catch? The pressure-lowering effect was nearly identical. So if you’re on these drops for life, switching to preservative-free might protect your eye surface - even if it costs more.
Beta blockers, on the other hand, can be dangerous if you have hidden health conditions. A patient might not know they have early-stage asthma or a slow heart rhythm. That’s why doctors should always ask about breathing problems, fatigue, or dizziness before prescribing. And never stop a beta blocker suddenly - it can cause a dangerous spike in eye pressure.
Another overlooked risk: prostaglandins can trigger cystoid macular edema in people who’ve had cataract surgery. It’s rare - about 0.5% to 1% - but serious. If your vision gets blurry or distorted after starting a prostaglandin, tell your eye doctor right away.
Combining Medications: When More Isn’t Better
Many patients end up on two or more drops. That’s because one isn’t enough. But here’s a myth: combining two prostaglandins won’t help. In fact, it might raise your pressure. Studies show that using bimatoprost and latanoprost together can backfire. Don’t do it.
But combining a prostaglandin with a beta blocker? That’s a classic and effective duo. Together, they can lower pressure an extra 13% to 25% beyond either alone. That’s why fixed combinations - like latanoprost/timolol - exist. They reduce the number of drops you need. But they don’t always work better than separate drops. And if you’re sensitive to preservatives, fixed combos often contain more of them.
What Should You Do?
If you’ve just been diagnosed with glaucoma, your doctor will likely start you on a prostaglandin - usually latanoprost. It’s the safest, most convenient option for most people. But if you have asthma, heart disease, or chronic fatigue, beta blockers are off the table. You’ll need alternatives like brimonidine or dorzolamide.
If you’re already on a beta blocker and feel tired, short of breath, or dizzy, talk to your doctor. Don’t assume it’s just aging. It might be the medication.
If you’re on a prostaglandin and notice your iris changing color or your eyelashes growing wildly, you’re not alone. It’s normal. But if you’re bothered by redness or irritation, ask about switching to a preservative-free version. It’s not a cure, but it can make a noticeable difference in comfort.
Adherence is everything. Glaucoma doesn’t hurt. You won’t feel it getting worse. But if you skip drops, you’re slowly losing vision. Use pill organizers. Set phone alarms. Link your drops to brushing your teeth. Make it part of your routine.
What’s Next?
Glaucoma treatment is evolving. New sustained-release implants, laser therapies, and minimally invasive surgeries are becoming more common. But for now, drops are still the backbone of care. Over 60% of new patients in the U.S. and Europe start with a prostaglandin. Beta blockers are fading from first-line use - not because they don’t work, but because they’re too risky for too many people.
The future isn’t about finding the ‘best’ drug. It’s about finding the right one for you. The one you can take every day without fear, without discomfort, without side effects that ruin your life. That’s the goal. And that’s why knowing the difference between prostaglandins and beta blockers isn’t just medical knowledge - it’s personal survival.
Can prostaglandins cause permanent eye color changes?
Yes. Prostaglandin analogs like latanoprost, bimatoprost, and travoprost can cause a gradual darkening of the iris, especially in people with hazel, green, or light brown eyes. This change is permanent and usually becomes noticeable after 6 to 12 months of use. It affects about 5% to 10% of long-term users. The change is limited to the iris and does not affect vision.
Are beta blockers safe for people with asthma?
No. Beta blockers like timolol can trigger severe bronchospasm in people with asthma or COPD. Even though they’re eye drops, a small amount gets absorbed into the bloodstream and can tighten airways. The FDA requires a black box warning for this risk. Patients with respiratory conditions should avoid beta blocker eye drops and use alternatives like prostaglandins or carbonic anhydrase inhibitors.
Why are prostaglandins prescribed more often than beta blockers?
Prostaglandins are prescribed more often because they’re more effective at lowering eye pressure, require only one daily dose, and have fewer serious systemic side effects. Studies show patients are nearly twice as likely to stick with prostaglandins long-term compared to beta blockers. For most people, the benefits outweigh the cosmetic side effects like red eyes or eyelash growth.
Can I use both a prostaglandin and a beta blocker together?
Yes, and it’s a common and effective combination. Prostaglandins increase fluid drainage while beta blockers reduce fluid production. Together, they can lower eye pressure by an extra 13% to 25% compared to either alone. Fixed-dose combinations (like latanoprost/timolol) are available to simplify dosing. However, using two prostaglandins together is not recommended and may raise pressure.
Should I switch to preservative-free glaucoma drops?
If you’ve been using glaucoma drops for more than a year and have dry eyes, redness, or irritation, preservative-free versions may help. Studies show they improve tear film stability and reduce surface damage. While they don’t lower pressure more, they’re gentler on your eyes. The downside is cost - they’re 20% to 25% more expensive. But for long-term users, the eye health benefits often justify the price.
Do glaucoma drops cure the disease?
No. Glaucoma drops control eye pressure - the main risk factor - but they don’t cure the disease. They prevent or slow further damage to the optic nerve. Vision lost to glaucoma cannot be restored. That’s why consistent use is critical. Even if you feel fine, stopping drops can lead to irreversible vision loss over time.
Final Thoughts
Glaucoma isn’t something you can ignore. But it’s also not something you have to live in fear of. With the right medication - one that fits your body, your lifestyle, and your health history - you can protect your vision for decades. Prostaglandins are the go-to for most people. Beta blockers still have a place, but only when safety allows. The key isn’t perfection. It’s persistence. Take your drops. Talk to your doctor about side effects. Ask about preservative-free options. Your eyes will thank you.

steve rumsford
January 7, 2026 AT 11:52Christine Joy Chicano
January 7, 2026 AT 13:40Vince Nairn
January 8, 2026 AT 02:00Mina Murray
January 9, 2026 AT 06:04Kyle King
January 10, 2026 AT 21:37Jessie Ann Lambrecht
January 11, 2026 AT 07:33Adam Gainski
January 13, 2026 AT 00:29Ayodeji Williams
January 14, 2026 AT 17:22Poppy Newman
January 16, 2026 AT 03:56Sai Ganesh
January 18, 2026 AT 03:03Andrew N
January 20, 2026 AT 02:05Paul Mason
January 20, 2026 AT 16:13Elen Pihlap
January 22, 2026 AT 14:59Kamlesh Chauhan
January 22, 2026 AT 19:54