GLP-1 Dose Escalation Calculator
Dose Escalation Calculator
Find the optimal dose escalation schedule to minimize nausea while achieving your weight loss goals with GLP-1 agonists like Ozempic, Wegovy, or Mounjaro.
Key Facts
- Nausea incidence 40%+
- Peak side effects First 4 weeks
- Typical improvement 4-8 weeks
- Best strategy Go slow
When you hear about GLP-1 receptor agonists like Ozempic or Wegovy, the conversation often centers on weight loss. People share success stories - dropping 20 pounds, reversing prediabetes, finally feeling in control of their appetite. But behind those results is a very real, very common problem: nausea, stomach pain, vomiting, and other gastrointestinal (GI) side effects that can make these drugs feel like a burden instead of a breakthrough.
More than 40% of people who start a GLP-1 agonist experience nausea. For some, it’s a mild discomfort. For others, it’s debilitating. A 2022 study in the Journal of Clinical Medicine found that up to 70% of users report GI side effects during the first few weeks. That’s not a small number - it’s nearly 7 out of 10 people. And while these effects usually fade, they’re still the #1 reason people quit taking the medication.
Why Do GLP-1 Drugs Make You Feel Sick?
It’s not a bug - it’s the feature. GLP-1 agonists work by mimicking a natural hormone in your gut called glucagon-like peptide-1. This hormone tells your brain you’re full, slows down how fast food leaves your stomach, and helps your pancreas release insulin. That’s why they’re so good for weight loss and blood sugar control.
But slowing your digestion? That’s a double-edged sword. When food moves too slowly through your stomach, it sits there longer. That can cause bloating, pressure, and nausea. Your body isn’t used to it. Think of it like putting your car in neutral on a hill - the engine’s still running, but nothing’s moving smoothly. Your gut is doing the same thing.
This isn’t just about one drug. All GLP-1 agonists - whether it’s liraglutide (Victoza), semaglutide (Ozempic, Wegovy), or tirzepatide (Mounjaro) - do this. It doesn’t matter if it’s a daily shot or a weekly one. The mechanism is the same. That’s why GI side effects are a class-wide issue, not a problem with a single brand.
What Side Effects Should You Expect?
Here’s what most people actually experience, based on real-world data and clinical trials:
- Nausea - The most common. Feels like a constant queasiness, sometimes with the urge to vomit. Affects 15-25% of users at maintenance dose.
- Vomiting - Less common than nausea, but still frequent. Happens in 5-10% of users.
- Diarrhea - Your gut gets too active. Happens in up to 20% of people.
- Constipation - Slowed digestion can also mean nothing moves. About 15% report this.
- Bloating and stomach pain - A dull, heavy feeling after eating. Often worse with fatty or sugary meals.
- Indigestion - Heartburn, burping, or a feeling that food is stuck.
These usually start during the first few weeks - especially during the dose-escalation phase. That’s when your doctor slowly increases the dose to help your body adjust. That’s also when most side effects peak.
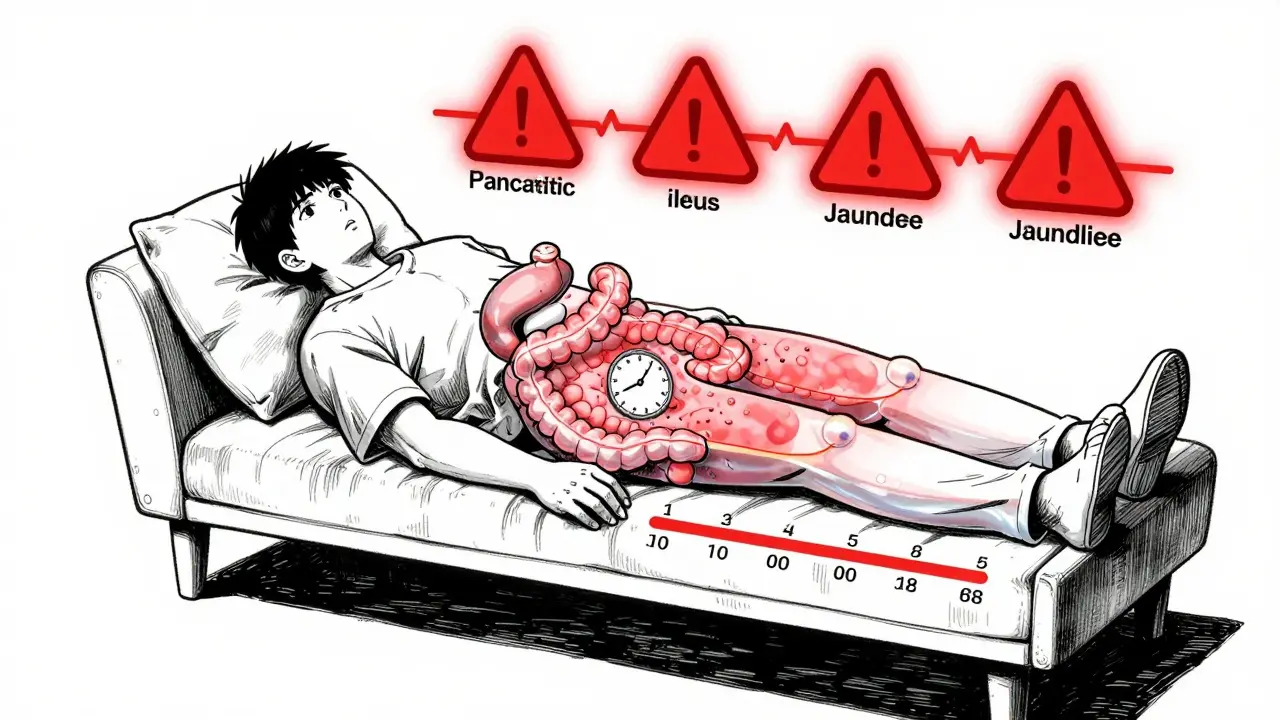
When to Worry: Red Flags You Can’t Ignore
Most GI side effects are annoying, not dangerous. But some symptoms mean you need to call your doctor - right away.
- Severe, persistent abdominal pain - Not just cramps. Sharp, unrelenting pain could signal pancreatitis or bowel obstruction.
- Cannot pass gas or have a bowel movement - This could mean ileus, a dangerous paralysis of the intestines.
- Jaundice - Yellow skin or eyes. Could mean liver or gallbladder trouble.
- Severe vomiting or diarrhea lasting more than 24 hours - This can lead to dehydration and kidney stress.
A 2023 study in JAMA Network Open found that GLP-1 agonists increased the risk of pancreatitis by over 9 times compared to other weight-loss drugs. Bowel obstruction risk went up 4 times. These are rare - but real. If you’re on one of these drugs and feel like something’s seriously wrong, don’t wait. Get checked.
How Long Do These Side Effects Last?
The good news? Most people get used to it.
Research shows that nausea and other GI issues usually improve within 4 to 8 weeks. By the time you reach your full maintenance dose - often after 16 to 20 weeks - symptoms are much milder or gone entirely. A Reddit thread from r/Ozempic had hundreds of users saying, "Week 3 was hell. Week 6? I barely notice it."
That’s why sticking with the medication matters. The body adapts. Your gut learns to handle the slower emptying. But you have to give it time. Quitting too early means you’ll never get to the other side - the weight loss, the better blood sugar, the energy.
How to Manage the Side Effects (Practical Tips)
If you’re struggling, here’s what actually works - based on clinical advice and user experience:
- Go slow with the dose - Don’t rush the escalation. If your doctor is increasing your dose every 4 weeks, stick to that schedule. Slower = less nausea.
- Eat smaller meals - Skip the big dinner. Eat 4-5 small meals instead. Your stomach can’t handle large volumes.
- Avoid high-fat and sugary foods - Fatty meals (pizza, fried chicken, ice cream) are the worst offenders. They sit in your stomach longer and trigger nausea.
- Stay hydrated - Sip water throughout the day. Don’t chug. Dehydration makes nausea worse.
- Don’t lie down after eating - Wait at least 2 hours. Gravity helps your stomach empty.
- Try ginger or peppermint - Ginger tea, ginger candies, or peppermint oil capsules can help calm nausea. Many users swear by this.
- Take the dose at night - If nausea hits hardest in the morning, try taking it before bed. Sleep helps your body process the drug.
- Don’t skip meals - Even if you’re not hungry, eat something light. An empty stomach can make nausea worse.
Some people use over-the-counter meds like Dramamine or Pepto-Bismol. Talk to your doctor first. They’re not always safe with GLP-1 drugs.

What About Long-Term Use?
Even after side effects fade, you still need to be mindful. Long-term use means your digestive system stays slower than normal. That’s why doctors recommend stopping GLP-1 drugs at least a week before surgery - to avoid anesthesia complications from delayed stomach emptying.
Also, if you’ve been on the drug for months or years and suddenly start having GI issues again, don’t assume it’s just "old side effects." It could be something else - gallstones, an ulcer, or even a new food intolerance. Get it checked.
Why Do People Keep Taking It?
Because the benefits are huge.
One study in the New England Journal of Medicine showed that semaglutide helped people lose an average of 14.9% of their body weight over 68 weeks. Placebo? Just 2.4%. That’s not just a few pounds - it’s life-changing for people with type 2 diabetes, fatty liver, or severe obesity.
And it’s not just about weight. Better blood sugar control means fewer diabetes complications - less nerve damage, fewer kidney problems, lower risk of heart attack. For many, the trade-off is worth it.
That’s why the global market for these drugs is projected to hit $43.6 billion by 2028. People are willing to deal with nausea because the payoff is real.
What’s Next?
Researchers are already working on next-gen versions. New drugs in development aim to reduce GI side effects by changing how the drug is absorbed or delivered. Some are combining GLP-1 agonists with other medications to allow lower doses - meaning less nausea, same results.
For now, the best strategy is patience, smart eating, and communication with your doctor. Don’t let nausea stop you from seeing the full benefit. Most people who stick with it say the side effects fade - and the results? They’re worth it.


Mike Hammer
February 14, 2026 AT 19:37Daniel Dover
February 16, 2026 AT 03:24Chiruvella Pardha Krishna
February 16, 2026 AT 09:04Virginia Kimball
February 17, 2026 AT 10:44Kapil Verma
February 19, 2026 AT 06:54Mandeep Singh
February 21, 2026 AT 04:00Betty Kirby
February 21, 2026 AT 11:47Erica Banatao Darilag
February 22, 2026 AT 15:29Joe Grushkin
February 23, 2026 AT 21:27