Medication Swelling Emergency Checker
Assess Your Symptoms
This tool helps you determine if your hand or foot swelling requires immediate medical attention based on FDA guidelines.
Swelling in your hands or feet might seem like a minor annoyance-maybe you wore tight shoes, stood too long, or had a salty meal. But if it’s new, sudden, or getting worse, it could be your medication talking. And in some cases, ignoring it could lead to something serious.
What’s Actually Happening When Your Hands or Feet Swell?
Swelling from medications isn’t just water retention-it’s a biological reaction. There are two main types you need to know about.
The first is vasodilator-induced edema. This happens when drugs like amlodipine (a common blood pressure pill), nitrates, or gabapentin cause your blood vessels to widen. That extra space lets fluid leak into your tissues, especially in your ankles and feet. You’ll notice pitting swelling-press your skin and it leaves a dent. It usually shows up after a few weeks on the drug, gets worse during the day, and improves when you lie down.
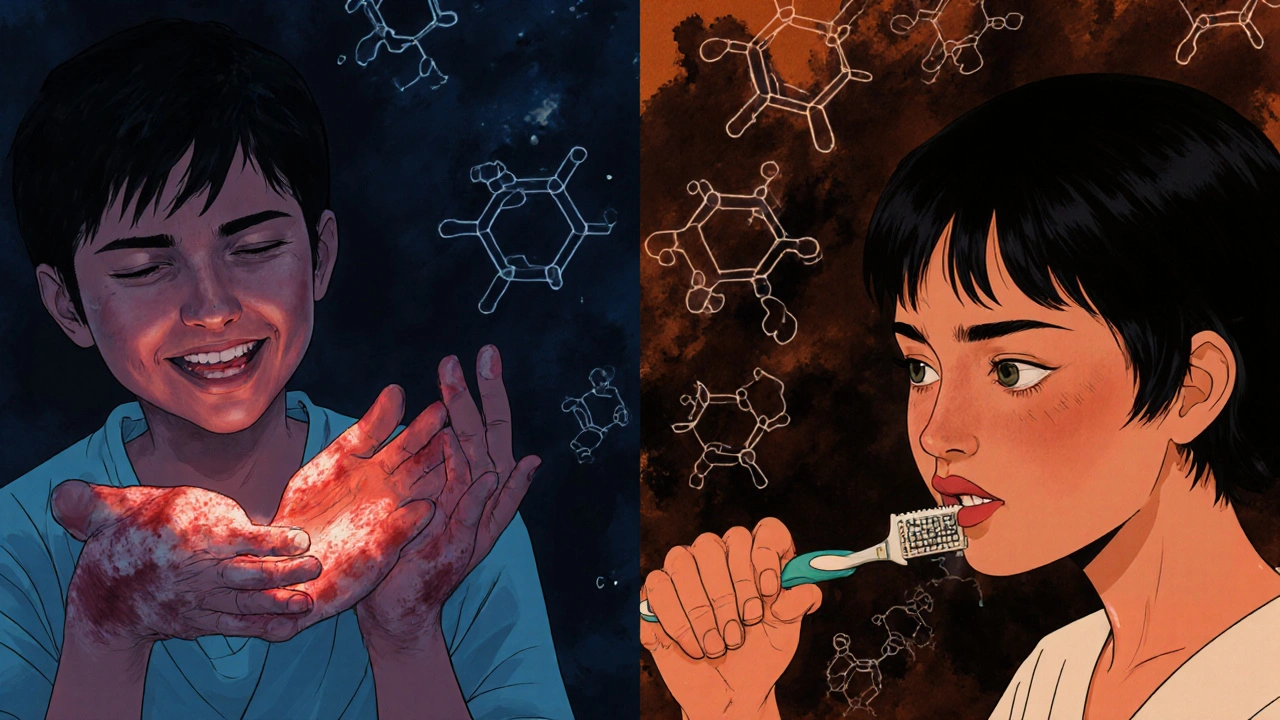
The second is hand-foot syndrome (also called palmar-plantar erythrodysesthesia). This one’s more common with chemotherapy drugs like capecitabine. Instead of just puffiness, you get redness, tingling, numbness, and sometimes blisters or peeling skin on your palms and soles. It’s not just uncomfortable-it can make it hard to hold a toothbrush, open a jar, or walk without pain.
According to the 2022 GoodRx analysis of FDA data, up to 15% of people taking a 10mg daily dose of amlodipine develop noticeable swelling. For chemo patients, that number jumps to 50-60% with capecitabine. These aren’t rare side effects-they’re common enough that doctors expect them.
Which Medications Are Most Likely to Cause This?
Not all drugs cause swelling the same way. Here’s who’s most likely to be the culprit:
- Calcium channel blockers (amlodipine, nifedipine): Most common cause of foot swelling in people with high blood pressure. Risk goes up with higher doses.
- NSAIDs (ibuprofen, naproxen): Even over-the-counter painkillers can make you retain fluid, especially if taken daily for months.
- Corticosteroids (prednisone): Used for inflammation, but they mess with your kidneys’ ability to flush out sodium.
- Thiazolidinediones (pioglitazone): Diabetes meds that cause fluid buildup in 4-7% of users within three months.
- Chemotherapy agents (capecitabine, docetaxel): Cause hand-foot syndrome in up to 60% of patients.
- Gabapentin and pregabalin: Used for nerve pain and seizures, these are increasingly reported to cause swelling in the lower legs.
The NIH’s 2021 analysis found that swelling appearing within 72 hours of starting a new drug has a 78% chance of being drug-related. That’s a strong signal-not something to brush off.
When Does Swelling Become an Emergency?
Not all swelling needs a trip to the ER. But some signs mean you should call your doctor today:
- Swelling is only on one side-like just your right ankle. This could mean a blood clot (deep vein thrombosis), which can travel to your lungs.
- You’re short of breath or feel tightness in your chest. Swelling combined with breathing trouble could signal heart failure.
- You gained more than 2 pounds in 24 hours or over 5 pounds in a week. That’s fluid overload, not just puffiness.
- Your skin is red, warm, or breaking open-especially on your hands or feet. Ulcers or blisters mean hand-foot syndrome has reached a dangerous stage.
- You’re urinating less than 500 mL a day (about 2 cups). Reduced urine output with swelling suggests kidney trouble or severe fluid imbalance.
- Fever comes with swelling. Infection plus swelling? That’s a red flag.
The American Heart Association and ASCO both say: if you have any of these, don’t wait. Call your doctor or go to urgent care. Delayed care is behind 37% of serious outcomes from medication-induced swelling, according to FDA data from 2023.
What Your Doctor Will Do
Once you report the swelling, your doctor won’t just tell you to “elevate your feet.” They’ll dig into why it’s happening.
For swelling from blood pressure meds like amlodipine, the first move is often dose adjustment. Switching from 10mg to 5mg can cut swelling risk by more than half. If that doesn’t help, switching to a different class of drug-like an ACE inhibitor or ARB (losartan, lisinopril)-resolves the issue in 85% of cases within two weeks.
For hand-foot syndrome from chemo, the approach is different. Your oncologist may reduce your chemo dose or delay the next cycle. Some patients get pyridoxine (vitamin B6), but studies show mixed results. A 2022 Cochrane review found no clear benefit. Topical urea cream is sometimes used, but guidelines disagree on whether it’s worth it.
One thing almost all experts agree on: compression stockings (20-30 mmHg pressure) help. A 2021 trial with 127 patients showed a 40% drop in swelling severity. They’re not glamorous, but they work.
What You Can Do at Home
While you wait for your appointment or manage mild swelling, these steps can help:
- Elevate your legs for 30 minutes, three times a day. Keep them above heart level. Clinical data shows this reduces swelling volume by 15% in 48 hours.
- Limit salt. Aim for under 2,300 mg per day. That’s about one teaspoon of salt. Processed foods, canned soups, and restaurant meals are the hidden culprits.
- Wear loose, comfortable shoes. Look for ones with extra depth (1-1.5 cm) so your swollen feet aren’t squeezed.
- Move gently. Walk for 10-15 minutes a few times a day. Movement helps your muscles pump fluid back up.
- Take diuretics at the right time. If your doctor prescribes water pills, take them in the morning so you’re not waking up every hour to pee.
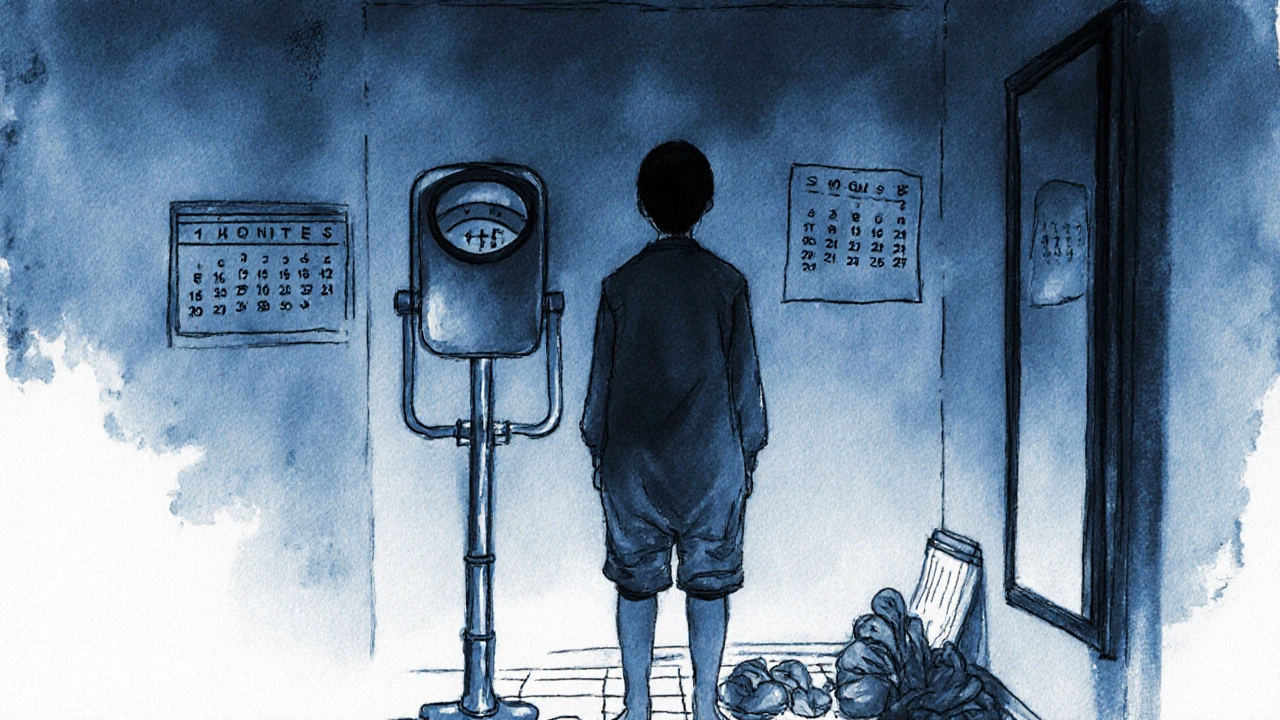
- Track your weight daily. Step on the scale at the same time each morning, after using the bathroom. A sudden jump is your body’s alarm bell.
Some people swear by arnica gel or Epsom salt soaks, but there’s no solid proof they help. Stick to what’s backed by data.
Why People Wait Too Long (And What It Costs)
A 2023 survey by the National Edema Foundation found that 55% of patients with medication-induced swelling waited to call their doctor. Why? They thought it was “normal,” “just aging,” or “not bad enough.”
That delay is dangerous. The average time between noticing swelling and seeking help? 8.2 days. In that time, fluid can build up enough to strain your heart, kidneys, or skin. One Reddit user described “sock marks that last all day” from pregabalin-painful, but they didn’t say anything for three weeks. By then, their feet were so swollen they couldn’t wear shoes.
On the flip side, people who act fast often see quick results. One GoodRx user switched from amlodipine to losartan and had complete ankle swelling resolution in five days-without losing blood pressure control.
Prevention Is Possible
You don’t have to just accept swelling as part of the deal. Here’s how to reduce your risk:
- Start with the lowest effective dose of any new medication. For amlodipine, 2.5-5mg instead of 10mg cuts swelling risk by 60%.
- If you’re on chemo, ask about prophylactic urea cream. A 2023 trial showed a 25% reduction in hand-foot syndrome when applied twice daily.
- Get educated. Patients who received clear instructions on swelling signs were 3.2 times more likely to report symptoms early, according to the Norton School’s 2023 data.
Bottom line: You don’t need to suffer in silence. Medication side effects are manageable-if you speak up.
What Happens After You Call Your Doctor?
Most cases resolve quickly once the cause is addressed. The American Journal of Medicine reports that 89% of medication-induced swelling clears up within four weeks of proper intervention. But 11% develop chronic lymphedema, which needs ongoing care-compression, physical therapy, and sometimes special garments.
If your doctor changes your medication, they’ll monitor you closely. Blood pressure, kidney function, and fluid balance will be checked. Don’t stop or switch drugs on your own. Even if the swelling seems minor, it’s your body telling you something’s off.
And if you’re on multiple medications? That’s even more reason to be cautious. A 2023 review by Dr. Robert Page II points out that swelling in someone taking several drugs isn’t always about one pill-it could be a dangerous interaction. That’s why a full medication review is essential.
Is hand and foot swelling from medication normal?
It’s common, but not normal. Up to 15% of people on amlodipine get swelling, and up to 60% of chemo patients develop hand-foot syndrome. But “common” doesn’t mean harmless. It’s a side effect your doctor needs to know about so they can adjust your treatment and prevent complications.
How long does swelling last after stopping the medication?
Most swelling improves within 1-4 weeks after stopping or switching the drug. For vasodilator-induced edema, it often clears in 7-10 days. Hand-foot syndrome from chemo may take longer, especially if skin damage occurred. Patience helps, but don’t wait more than a month without checking in with your doctor.
Can I take a diuretic (water pill) to reduce the swelling?
Only if your doctor says so. Diuretics can help with fluid overload, but they don’t fix the root cause. For example, if swelling is from calcium channel blockers, a diuretic might mask the issue without stopping the vasodilation. Plus, they can cause low potassium, dizziness, or kidney stress. Never self-prescribe.
Should I stop taking my medication if I get swelling?
No. Stopping abruptly can be dangerous-especially for blood pressure or heart meds. Contact your doctor first. They might lower your dose, switch you to another drug, or add a treatment to manage the swelling. Never make changes on your own.
Can stress or diet cause this kind of swelling?
Stress and high salt intake can make swelling worse, but they don’t cause medication-induced edema on their own. If you started a new drug and swelling appeared shortly after, the medication is the likely trigger. Diet and stress are contributing factors, not the primary cause.
Is hand-foot syndrome the same as a rash?
No. A rash is usually itchy and spread out. Hand-foot syndrome starts with tingling, then redness, swelling, and sometimes peeling or blistering-mostly on the palms and soles. It’s a direct toxic reaction to certain chemo drugs, not an allergic response. It can be very painful and interfere with daily tasks.
Are there natural remedies that help?
Some people report relief with arnica gel, Epsom salt soaks, or cold compresses, but clinical evidence is limited. A 2023 study showed arnica reduced HFS symptoms by 28% compared to placebo, but it’s not yet a standard recommendation. The safest, most proven methods are medical adjustments, compression, salt control, and elevation.
Will I always have swelling if I stay on this medication?
Not necessarily. Many people find that swelling improves after a few weeks as their body adjusts. Others need a dose change or a switch to a different drug. In about 45% of cases, swelling persists despite management-then discontinuing the drug is the only option. Your doctor will help you weigh the benefits of the medication against the side effects.
Final Thoughts
Swelling in your hands or feet isn’t something to ignore-especially if it started after a new medication. It’s not just a nuisance. It’s a signal. Whether it’s from a blood pressure pill, a painkiller, or chemo, the right action can prevent bigger problems. Talk to your doctor early. Track your symptoms. Don’t assume it’s “just part of getting older.” Your body is giving you information. Listen to it.


Ryan C
November 26, 2025 AT 07:51Let’s be real - if you’re on amlodipine and your socks leave impressions that last until dinner, you’re not ‘just retaining water.’ You’re experiencing vasodilator-induced edema, and it’s documented in the FDA’s Adverse Event Reporting System (2022). The NIH says 78% of new-onset swelling within 72 hours of starting a new med is drug-related. Don’t let your doctor brush it off with ‘elevate your feet.’ Dose reduction to 5mg cuts risk by 60%. If it persists, switch to an ARB. Losartan works. I’ve seen it.
Also - compression stockings (20-30 mmHg) aren’t optional. They’re evidence-based. A 2021 trial with 127 patients showed a 40% drop in severity. You’re not ‘old’ - you’re pharmacologically affected. 📊🩺
Dan Rua
November 27, 2025 AT 20:12Hey, thanks for laying this out so clearly. I’ve been on gabapentin for nerve pain and started noticing swelling in my ankles after about 4 weeks. I didn’t think it was the med because I thought it was just from sitting too much at my desk. Now I’m going to talk to my doc about lowering the dose - I didn’t realize it was this common. Appreciate the data points. 😊
Douglas Fisher
November 28, 2025 AT 08:13So, I’ve had this issue for months - swelling in my feet, especially after lunch. I thought it was my diet, or maybe I was just getting older. But then I read this - and realized I’d been on prednisone for my eczema for 6 months. I didn’t connect the dots. I’ve been limiting salt, elevating my legs, and wearing loose shoes - but I didn’t know corticosteroids mess with sodium excretion. I’m calling my doctor tomorrow. Thank you for the clarity. I feel less alone now. 🙏
Stephanie Deschenes
November 29, 2025 AT 06:48I’m a nurse, and I’ve seen this so many times. Patients will say, ‘It’s just swelling,’ and wait until their skin breaks open or they can’t walk. Hand-foot syndrome from chemo is brutal - it’s not a rash, it’s a toxic reaction. I always tell my patients: if your palms feel like they’re on fire, or your soles are peeling like sunburn - don’t wait. Tell your oncologist. There’s a reason they give you that pamphlet. Prophylactic urea cream isn’t magic, but it helps. And compression socks? They’re ugly, but they’re your best friend. You’ve got this. 💪
vikas kumar
November 30, 2025 AT 22:29From India, here. I’ve seen many patients here ignore swelling because they think it’s ‘normal’ or ‘too expensive’ to change meds. But this post is spot-on. Amlodipine is everywhere here - cheap, effective - but the swelling? Common. We don’t always have access to ARBs, but even reducing the dose helps. And compression stockings? We use old cotton bandages as makeshift ones. It’s not perfect, but it’s better than nothing. Thank you for sharing real data. People need to know - this isn’t just ‘aging.’ It’s medicine. 🙏
Vanessa Carpenter
December 1, 2025 AT 16:19I had hand-foot syndrome from capecitabine. It felt like my hands were dipped in hot glue. Couldn’t hold a coffee cup. My oncologist cut my dose by 25% and told me to use urea cream twice a day. Took 3 weeks to recover. Didn’t help with the pain, but stopped it from getting worse. I didn’t know about the 60% stat - that’s wild. I’m glad someone wrote this. I wish I’d known sooner. 🤍
Bea Rose
December 3, 2025 AT 02:28Michael Collier
December 4, 2025 AT 01:21As a primary care physician, I appreciate the comprehensive breakdown. I would only add that when patients present with unilateral swelling - particularly in the context of recent immobility or cancer - we must rule out deep vein thrombosis before attributing it to medication. The American Heart Association’s guidance on this is unequivocal. Furthermore, while compression therapy is underutilized, its efficacy is well-documented. I routinely prescribe 20-30 mmHg stockings as first-line adjunctive therapy, and I’ve observed a marked reduction in patient distress and clinic visits. Please, if you are experiencing unexplained edema, do not delay consultation. The window for intervention is narrow, and the consequences of inaction are disproportionate to the inconvenience of a single office visit. Your health is not a suggestion - it is a priority.