Every year, Americans spend over $650 billion on prescription drugs. That’s more than any other country in the world. But here’s the surprising part: generics make up 90% of all prescriptions filled, yet they only account for 12% of total spending. Meanwhile, brand-name drugs, which make up just 10% of prescriptions, swallow up 88% of the money. This isn’t a mistake. It’s the power of generics at work.
What Exactly Are Generic Drugs?
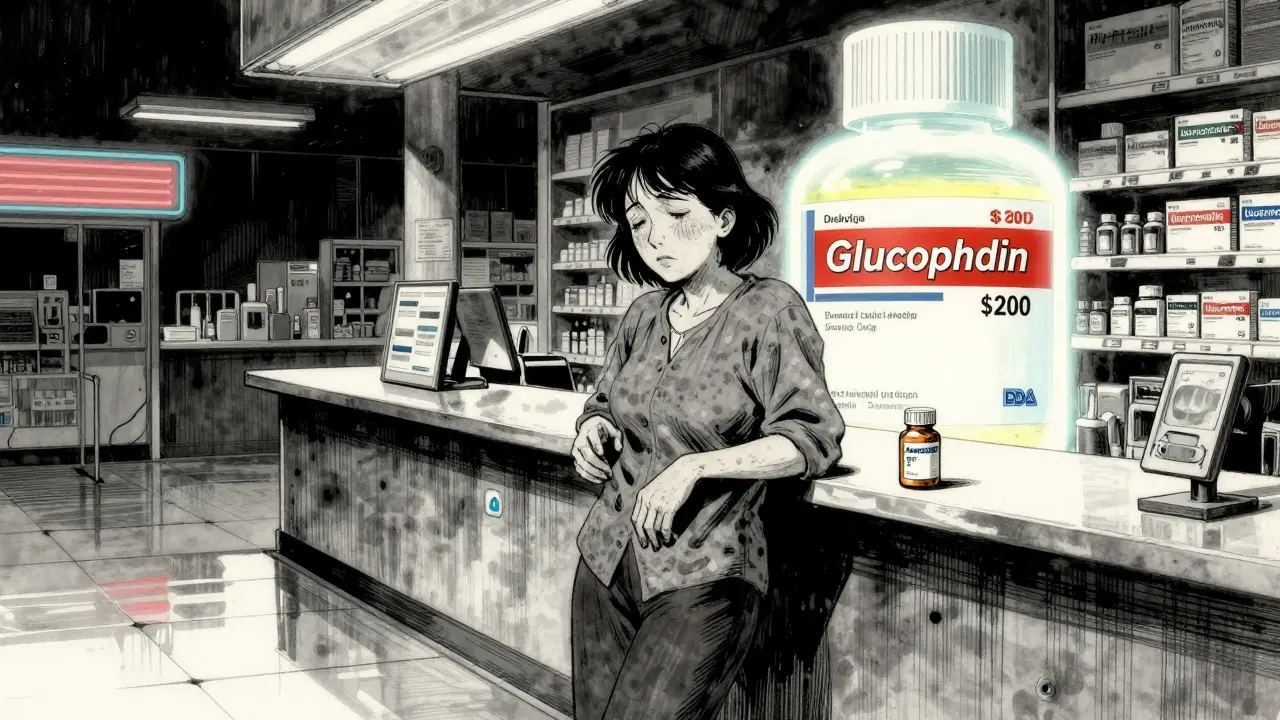
Generic drugs are chemically identical copies of brand-name medications. They contain the same active ingredient, in the same strength, and work the same way in your body. The FDA requires them to meet the same strict standards for safety, purity, and effectiveness. The only differences? The color, shape, or inactive ingredients like fillers or dyes - and the price. Generics cost, on average, 80 to 85% less than their brand-name equivalents. Take metformin, for example. The brand-name version, Glucophage, used to cost over $200 a month. Today, the generic version sells for under $10 at most pharmacies. The same goes for statins like atorvastatin (Lipitor), blood pressure meds like lisinopril, and even insulin. When generics enter the market, prices drop fast - often by 90% within a year.How Generics Got Their Start
Before 1984, bringing a generic drug to market meant repeating the same expensive clinical trials as the original. That made generics too costly to produce. Everything changed with the Hatch-Waxman Act. This law created a shortcut: the Abbreviated New Drug Application (ANDA). Instead of proving safety and effectiveness from scratch, generic manufacturers only had to show their product was bioequivalent to the brand-name drug. Bioequivalence means the generic delivers the same amount of active ingredient into your bloodstream at the same rate as the brand. The FDA tests this with 24 to 36 healthy volunteers, taking blood samples over 72 hours. If the generic’s absorption falls within 80-125% of the brand’s, it’s approved. No need for long-term outcome studies. No need for massive clinical trials. Just science, efficiency, and lower costs. Since then, over 14,000 generic products have been approved. The FDA’s Orange Book, which lists all approved generics and their therapeutic equivalence ratings, is now the go-to tool for pharmacists and doctors deciding what to substitute.The Real Impact on Spending
In 2024, generics saved the U.S. healthcare system $98 billion in direct spending. That’s not a guess. It’s from the Association for Accessible Medicines’ official report. Cumulative savings since 1984? Over $445 billion. That’s enough to cover the annual healthcare costs of millions of uninsured people. The numbers tell the story:- 90% of prescriptions filled = generics
- 12% of total drug spending = generics
- 10% of prescriptions filled = brand-name
- 88% of total drug spending = brand-name

Generics vs. Other Cost-Cutting Strategies
Some people think drug price negotiations or step therapy are the best ways to control spending. They’re not. Medicare negotiations on 10 drugs in 2026 are projected to save $6 billion a year. That’s impressive - but it only affects 10 drugs. Generics affect thousands. The Congressional Budget Office found that generic competition reduces prices by 90% after patent expiry. Medicare negotiation? Only 42%. Step therapy - where you try cheaper drugs first - saves 12-15% per episode. Generics save 80-85% per pill. Even specialty drugs - the most expensive ones, like cancer treatments or rare disease meds - are starting to see relief through biosimilars. These are the generic versions of complex biologic drugs. They’re not exact copies, but they’re close enough to be just as effective. And they cost 15-35% less than the original. That’s not a full 80% drop, but it’s still massive when you’re talking about $10,000-a-month treatments.Where Generics Struggle
Generics aren’t magic. Some drugs are just too hard to copy. Complex molecules - like inhalers, injectables, or topical creams - are tricky. The active ingredient might be simple, but how it’s delivered matters. A generic inhaler might have the same drug, but if the propellant or nozzle design is different, it won’t work the same way. The FDA requires extra testing for these, which drives up cost and delays entry. Then there’s the patent thicket. Brand-name companies file dozens, sometimes over 100, patents on a single drug - not just for the active ingredient, but for packaging, dosage forms, even the color of the pill. This legal maze can delay generics for years. One study found patent litigation adds an average of 28 months to the time between patent expiry and generic launch. And then there’s the ‘pay-for-delay’ problem. Sometimes, the brand-name company pays the generic maker to wait before entering the market. The FTC estimates these deals cost consumers $3.5 billion a year in higher prices. Even worse, some brand companies release their own “authorized generics” - copies made by the original manufacturer - right when the patent expires. This keeps prices high because there’s no real competition. Instead of a 90% drop, prices only fall 25-30%.Real People, Real Savings
Behind every statistic is a person. A Reddit user shared how switching her mom from brand-name Humalog insulin ($350/month) to generic insulin lispro ($25/month) kept her from rationing doses. That’s not an outlier. GoodRx’s 2024 report found 68% of patients skip or split pills when generics aren’t available. For Medicare beneficiaries, 42% skip doses for brand-name drugs - but only 12% do so for generics. On Drugs.com, patients rate generics 4.1 out of 5 for effectiveness - almost identical to brand-name drugs. But affordability? Generics score 4.5 out of 5. Brands? 2.3. Still, complaints exist. In 2023, the FDA received over 1,200 reports of side effects linked to generic substitutions. Most were from changes in inactive ingredients - fillers that cause stomach upset in some people. For drugs with a narrow therapeutic index - like warfarin or levothyroxine - even tiny differences can matter. A small percentage of patients report symptoms returning after switching. That’s why some states require doctor approval before substituting these drugs.

Lydia H.
January 18, 2026 AT 08:27Generics are the quiet heroes of modern medicine. I never thought about how much of my dad’s monthly pill costs were just padding for corporate profits until I saw the price drop from $280 to $18 for his lisinopril. It’s not magic-it’s just common sense.
Josh Kenna
January 19, 2026 AT 22:34bro why are we still paying 200 bucks for insulin when the generic is 25?? my cousin had to choose between rent and her meds last year. this system is broken. someone needs to burn down the pharma boardroom and replace it with librarians.
Jacob Hill
January 21, 2026 AT 07:55Let me just say, I didn’t realize how much of a difference generics made-until my wife switched from brand-name Zoloft to sertraline. Same effect, same dosage, same results. And we saved $180 a month. Honestly? I’m kind of mad we didn’t do this sooner.
Valerie DeLoach
January 21, 2026 AT 10:36It’s fascinating how something so simple-replacing a brand logo with a plain pill-can dismantle entire economic structures built on fear and misinformation. We’ve been conditioned to believe that ‘brand’ means ‘better,’ when in reality, it just means ‘more expensive.’ The FDA’s bioequivalence standards are rigorous, and yet, the marketing machine still convinces people to pay 10x more for the same molecule. This isn’t healthcare-it’s behavioral economics disguised as medicine.
And let’s not forget the psychological weight of a pill: the color, the shape, the imprint. Patients report feeling ‘less effective’ when switching-even when the drug is identical. That’s not pharmacology. That’s placebo psychology. We need better patient education, not just cheaper pills.
Generics don’t just save money-they restore dignity. When a diabetic can afford to take their insulin without rationing, they’re not just surviving-they’re living. That’s not a statistic. That’s a human right.
And yet, we let PBMs dictate formularies based on rebates, not outcomes. We let patent thickets delay access for years. We let ‘authorized generics’ pretend to be competition while keeping prices high. The system is rigged. But at least we know the truth now.
Let’s not just celebrate generics. Let’s demand that they become the default-without asking, without opt-ins, without bureaucracy. Every prescription should start with: ‘Is there a generic?’ And if the answer is no, we should demand an explanation-not a copay.
Tracy Howard
January 22, 2026 AT 19:22U.S. healthcare is a joke, but at least we have generics. Canada? We pay half for the same drugs because our government actually regulates prices. You guys have a $650B problem because you let corporations run the show. Shameful.
Astha Jain
January 23, 2026 AT 01:42generic drugs r sooo good but why dose the FDA make it so hard to get them? like i get it but also like… why so many forms? its 2025!!
sujit paul
January 23, 2026 AT 14:31Did you know that 80% of the active ingredients in your ‘American-made’ generics come from China? And that the same factories that make your pills also make toxic laundry detergent? The FDA doesn’t inspect them properly. This is a national security threat. Your insulin is being made in a facility that failed 3 safety audits last year. Wake up.
Erwin Kodiat
January 25, 2026 AT 08:48I’ve been on metformin for 12 years. Switched from Glucophage to generic in 2018. Never noticed a difference. My A1C stayed stable. My wallet? Thank you. Generics aren’t ‘cheap’-they’re smart.
Christi Steinbeck
January 26, 2026 AT 08:21STOP letting insurance companies trick you! I called my PBM and asked why my generic copay was higher than the brand-and they admitted it was because the brand paid them a bigger rebate. I switched plans. Now I pay $5 for my blood pressure med. Don’t be afraid to fight. You’re not asking for a favor-you’re claiming your right to affordable care.
Lewis Yeaple
January 28, 2026 AT 03:36It is imperative to note that the Hatch-Waxman Act of 1984, codified under Title 21 of the United States Code, Section 355(j), established the Abbreviated New Drug Application (ANDA) pathway, which permits generic manufacturers to rely on the safety and efficacy data of the reference-listed drug, thereby circumventing redundant clinical trials. This regulatory innovation has demonstrably reduced pharmaceutical expenditures by an order of magnitude, as corroborated by the Congressional Budget Office and the Association for Accessible Medicines. The economic impact is both statistically significant and ethically non-negotiable.
Malikah Rajap
January 28, 2026 AT 20:14Wait, so… if generics are so great, why do some people get weird side effects after switching? Like, I know my friend’s thyroid meds made her feel like a zombie after the pharmacy switched her to generic levothyroxine. Is that real? Or is she just being dramatic? I feel like we need to talk about this more… like, really talk about it, not just brush it off like it’s not a big deal.
Aman Kumar
January 29, 2026 AT 20:05The entire pharmaceutical-industrial complex is a Ponzi scheme built on patent trolling, regulatory capture, and the commodification of human suffering. Generics are the only crack in the wall. But don’t be fooled-this is not a victory. It’s a temporary reprieve. The corporations are already lobbying for ‘evergreening’ extensions, biosimilar paywalls, and data exclusivity loopholes. The real enemy isn’t the pill-it’s the system that turns healing into a profit margin.
Jackson Doughart
January 30, 2026 AT 09:08One of the most profound, yet underappreciated, achievements of modern pharmacology is the systematic deconstruction of price inflation through bioequivalent alternatives. The fact that 90% of prescriptions are filled with generics, while accounting for only 12% of total expenditure, is not merely an economic anomaly-it is a moral imperative fulfilled. The disparity between cost and outcome underscores a fundamental truth: medicine need not be a luxury. It can-and should-be accessible.