Before you reach for that $4 prescription at the pharmacy, take a second to think about how we got here. Just a few decades ago, most Americans didn’t even know generic drugs existed. Today, more than 9 in 10 prescriptions filled in the U.S. are for generic versions of brand-name drugs. That’s not just convenience-it’s a revolution in how medicine is priced, made, and accessed. And it didn’t happen by accident.
From Patent Monopolies to the First Standards
The story starts long before modern pills and tablets. In 1820, eleven doctors gathered in Washington, D.C., and created the first U.S. Pharmacopeia-a list of standard drug ingredients and strengths. At the time, medicine was a wild west. A bottle labeled "quinine" might contain chalk, sawdust, or worse. There were no rules. This first compendium was the beginning of drug quality control in America.
By 1848, Congress passed the Drug Importation Act, giving U.S. Customs the power to stop fake or dangerous drugs from crossing the border. That was a small step, but it showed the government was starting to care. In 1888, the American Pharmaceutical Association published the National Formulary, another effort to stop counterfeit drugs from slipping through. Still, there was no enforcement. No oversight. No real accountability.
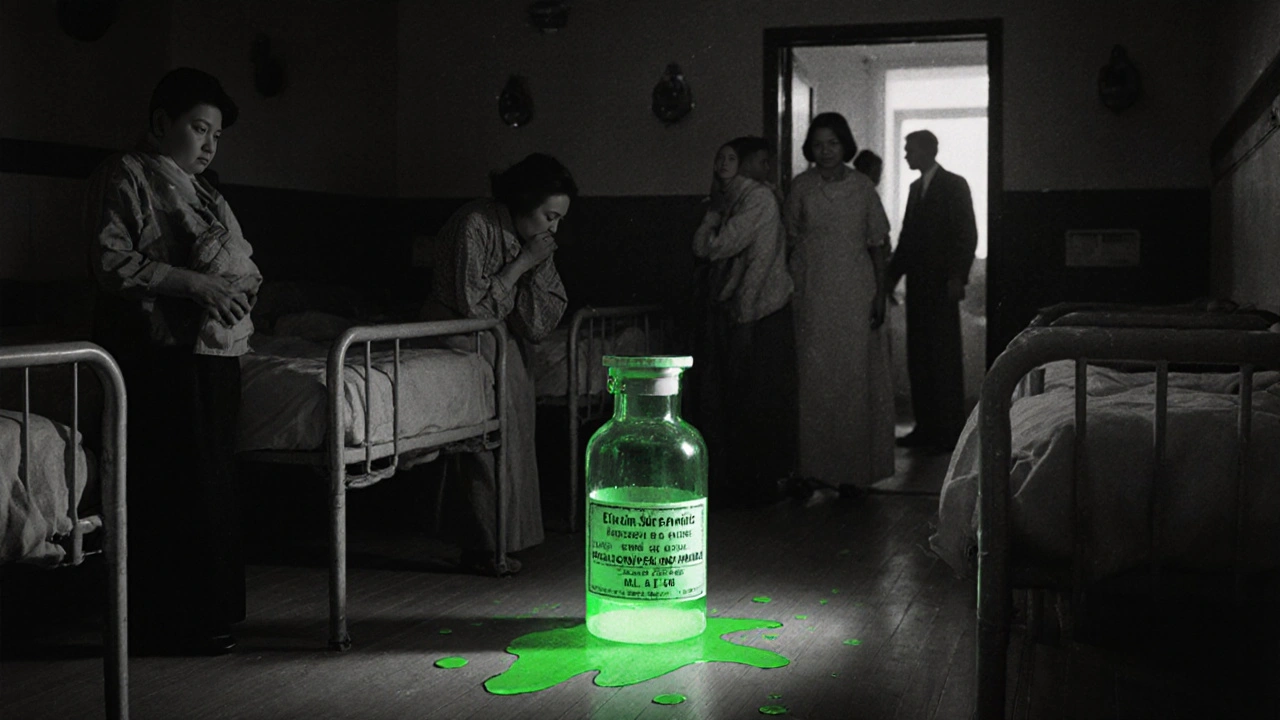
The Elixir Sulfanilamide Disaster and the Birth of Real Regulation
Everything changed in 1937. A pharmaceutical company in Tennessee marketed a new painkiller called Elixir Sulfanilamide. The drug was dissolved in diethylene glycol-a toxic chemical used in antifreeze. Over 100 people died, mostly children. The public outcry was immediate. Congress had no choice: they had to act.
In 1938, the Federal Food, Drug, and Cosmetic Act (FDCA) was signed into law. For the first time, drugmakers had to prove their products were safe before selling them. The FDA, which had been around since 1906 but had weak powers, suddenly had teeth. This law laid the foundation for everything that followed.
Prescriptions, Efficacy, and the Kefauver-Harris Amendments
By the 1950s, the drug market was growing fast. The Durham-Humphrey Amendment in 1951 split drugs into two categories: prescription and over-the-counter. That made sense. But there was still a huge gap: companies didn’t have to prove their drugs actually worked. They only had to prove they weren’t deadly.
That changed in 1962 after the thalidomide scandal in Europe. Although thalidomide wasn’t approved in the U.S., the FDA’s Dr. Frances Kelsey held it back, saving thousands of babies from severe birth defects. Her actions led to the Kefauver-Harris Drug Amendments, which required drugmakers to prove both safety and effectiveness. Suddenly, every new drug had to go through rigorous clinical trials.
And here’s the twist: the law also required the FDA to review every drug on the market between 1938 and 1962. Thousands of drugs were pulled or reclassified. The system was messy, expensive, and slow. But it created a new problem: brand-name companies now had a monopoly on proven, effective drugs. And they charged accordingly.

The Hatch-Waxman Act: The Turning Point
By the early 1980s, brand-name drugs dominated the market. But costs were rising fast. Medicare and Medicaid were spending billions. Congress knew something had to change. In 1984, they passed the Drug Price Competition and Patent Term Restoration Act-better known as the Hatch-Waxman Act.
This law was genius. It created a path for generic drugs to enter the market without repeating expensive clinical trials. Instead, generic makers only had to prove their version was bioequivalent-meaning it delivered the same amount of active ingredient into the bloodstream at the same rate as the brand-name drug. That’s it. No need to retest safety or effectiveness. The FDA already knew those things.
The law also gave brand-name companies a 5-year exclusivity period and a possible 30-month patent extension if they sued a generic maker. That last part became a loophole. Some companies used lawsuits not to protect real patents, but to delay competition. Still, the overall effect was dramatic. In 1984, only 19% of prescriptions were for generics. By 2022, that number hit 90.5%.
Cost Savings That Changed Healthcare
Here’s the real impact: in 2021, generic drugs saved the U.S. healthcare system $373 billion. Over the last decade, that total climbed to over $3.7 trillion. The Congressional Budget Office found generic drugs cut prescription costs by 80% to 85% compared to brand-name versions.
Think about that. You’re paying $4 for a blood pressure pill that costs $300 as a brand. That’s not magic. It’s policy. The Hatch-Waxman Act didn’t just make generics legal-it made them affordable. And that’s why 9 out of 10 prescriptions today are generic.

Quality, Shortages, and Global Supply Chains
But it’s not all smooth sailing. Between 2018 and 2022, the FDA recorded 1,234 drug shortages. Sixty-five percent of them involved generic drugs. Why? Because the generic industry is built on thin margins. Companies compete on price, not profit. When a manufacturer shuts down a plant, or a raw material gets delayed, there’s no backup.
And here’s the bigger issue: 80% of the active ingredients in U.S. generic drugs come from just two countries-China and India. The FDA inspects these foreign facilities, but they oversee more than 13,000 manufacturing sites worldwide. That’s a lot of ground to cover.
In 2012, the FDA launched the Generic Drug User Fee Amendments (GDUFA). It gave the agency more money to hire reviewers and speed up approvals. The results? Review times dropped from 30 months to 10. Approval rates jumped from 45% to 95%. That’s progress.
Price Spikes and Market Manipulation
Even with all these gains, there’s a dark side. Between 2013 and 2017, prices for 15% of generic drugs jumped more than 100%. Some drugs, like doxycycline or nitrofurantoin, went from pennies to dollars per pill. Why? Because a handful of companies controlled the market. When one manufacturer leaves, the rest can raise prices. It’s not illegal-it’s just how the system works when competition disappears.
The FDA and Congress have tried to fix this. The CREATES Act, passed in 2019, stops brand-name companies from blocking generic access by refusing to sell samples needed for testing. As of 2022, the FDA had taken 27 enforcement actions under this law.
What’s Next? Biosimilars and the Future
The next frontier isn’t small-molecule generics-it’s biosimilars. These are copies of complex biologic drugs, like those used for cancer, arthritis, or diabetes. They’re harder to make, harder to test, and much more expensive. But they’re coming fast.
By 2027, analysts expect generics to still make up 90% to 92% of prescriptions. Biosimilars will add another layer of competition. The goal is the same: lower costs. More access. Better care.
Generic drugs aren’t just cheaper versions of brand-name pills. They’re the backbone of affordable healthcare in America. They exist because of decades of law, science, and public pressure. They’re not perfect. But they’ve saved trillions-and they’re still saving lives every day.
Are generic drugs as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove bioequivalence-meaning they deliver the same amount of medicine into your bloodstream at the same rate. Thousands of studies and real-world use confirm they work just as well.
Why are generic drugs so much cheaper?
Generic manufacturers don’t have to repeat expensive clinical trials because the safety and effectiveness of the drug were already proven by the brand-name company. They also face competition from multiple makers, which drives prices down. Marketing and branding costs are minimal compared to brand-name drugs, which spend billions on advertising.
Do generic drugs have the same side effects?
Yes. Since the active ingredient is identical, the side effects are the same. Some people report differences because of inactive ingredients-like fillers or dyes-which can cause rare allergic reactions. But these are not related to the drug’s effectiveness. If you have a reaction, talk to your pharmacist or doctor.
Why do some generic drugs have different shapes or colors?
By law, generic drugs can’t look exactly like the brand-name version. That’s to avoid confusion. So manufacturers change the shape, color, or markings. But the active ingredient, dosage, and effect are unchanged. If you’re unsure, check the label or ask your pharmacist.
Can I trust generic drugs made overseas?
Yes. The FDA inspects all manufacturing facilities, whether they’re in the U.S., India, China, or elsewhere. The same standards apply. Over 80% of active ingredients come from outside the U.S., but every facility must meet U.S. quality rules. The FDA has increased inspections and uses risk-based monitoring to catch problems early.
What should I do if my generic drug seems different?
If you notice changes in how the drug works, or if you experience new side effects, contact your doctor or pharmacist. Sometimes, switching between different generic manufacturers can cause minor differences in how your body responds-but this is rare. Your pharmacist can help you identify if it’s a different manufacturer and whether you need to switch back.

Ragini Sharma
November 22, 2025 AT 05:23so like... i got my generic blood pressure med from india and it looks like a tiny rainbow pill? 😅 but it works?? how do i know they didnt just put sugar and vibes in there??
Linda Rosie
November 23, 2025 AT 02:05The regulatory framework established by the Hatch-Waxman Act represents a paradigm shift in pharmaceutical accessibility.
Vivian C Martinez
November 24, 2025 AT 11:53It’s amazing how much progress we’ve made-generic drugs are safe, effective, and save so many people money. Keep pushing for transparency and quality control. We’ve got this.
Ross Ruprecht
November 25, 2025 AT 02:57why do i care about all this history? just give me the $4 pill and stop talking.
Bryson Carroll
November 25, 2025 AT 18:3790 percent generics? that’s not progress that’s a surrender to third world manufacturing standards and corporate greed disguised as affordability
Lisa Lee
November 26, 2025 AT 16:0480% of active ingredients from China and India? no thanks. America should make its own medicine. This is national security.
Jennifer Shannon
November 27, 2025 AT 19:17It’s fascinating, isn’t it?-how a bunch of doctors in 1820, trying to stop chalk from being sold as quinine, set off a chain reaction that led to FDA inspections in Shanghai, biosimilars in 2027, and a $4 pill in my local pharmacy… it’s like a quiet revolution, stitched together by law, science, and sheer stubbornness. No parades, no headlines, just people living longer because someone cared enough to write a rule that didn’t let profit kill. And yet… we still fight over whether the blue pill is the same as the pink one. We’re complicated creatures.
Manjistha Roy
November 28, 2025 AT 15:24Many people worry about overseas manufacturing, but the FDA maintains strict standards regardless of location. It’s important to understand that quality control is not tied to geography but to regulatory enforcement.
Jennifer Skolney
November 30, 2025 AT 14:20Love this breakdown!! 💪 The Hatch-Waxman Act is one of those quiet heroes of modern medicine. Also, if your generic looks different? Totally normal. Your pharmacist is your best friend here. ❤️
JD Mette
December 1, 2025 AT 07:20I’ve been on the same generic for years. Never had an issue. But I know some people feel different when the pill changes color. It’s worth listening to those concerns, even if the science says it’s the same.