When you’re in your late 40s or early 50s and hot flashes wake you up three times a night, or your mood swings feel like a rollercoaster with no brakes, it’s easy to wonder: Hormone Replacement Therapy-is it worth it? For millions of women, the answer is yes. But it’s not a one-size-fits-all solution. The truth is, HRT can be life-changing-or risky, depending on how, when, and why it’s used.
What Hormone Replacement Therapy Actually Does
HRT replaces hormones your body stops making after menopause-mostly estrogen, and sometimes progesterone. Estrogen drops sharply after your last period, and that’s what triggers hot flashes, night sweats, vaginal dryness, sleep problems, and even brain fog. HRT doesn’t reverse aging. It doesn’t make you young again. But it can restore balance to your body’s chemistry so you feel more like yourself.
There are two main types: estrogen-only therapy (ET) for women who’ve had a hysterectomy, and estrogen-progestogen therapy (EPT) for those with a uterus. Why the difference? Estrogen alone can cause the lining of the uterus to thicken, raising the risk of endometrial cancer. Adding progesterone-or a synthetic version called progestin-keeps that lining thin and safe.
Delivery methods matter more than you think. Oral pills are common, but they go through your liver first, which can increase your risk of blood clots. Transdermal options-patches, gels, sprays-deliver hormones straight into your bloodstream through the skin. That means less stress on your liver and a 1.5 to 2 times lower risk of dangerous clots compared to pills.
The Real Benefits: More Than Just Hot Flash Relief
The biggest win with HRT? Relief from vasomotor symptoms. Studies show it cuts hot flashes and night sweats by 80-90%. That’s far better than SSRIs or other non-hormonal options, which typically reduce them by 50-60%. If you’re losing sleep and energy because of these symptoms, HRT can give you your life back.
Bone health is another major benefit. After menopause, women lose bone density rapidly. HRT reduces fracture risk by 34% compared to no treatment, according to the Women’s Health Initiative. That’s more effective in the short term than bisphosphonates like Fosamax. For women in their 50s or early 60s, HRT isn’t just about comfort-it’s about staying strong and avoiding broken hips.
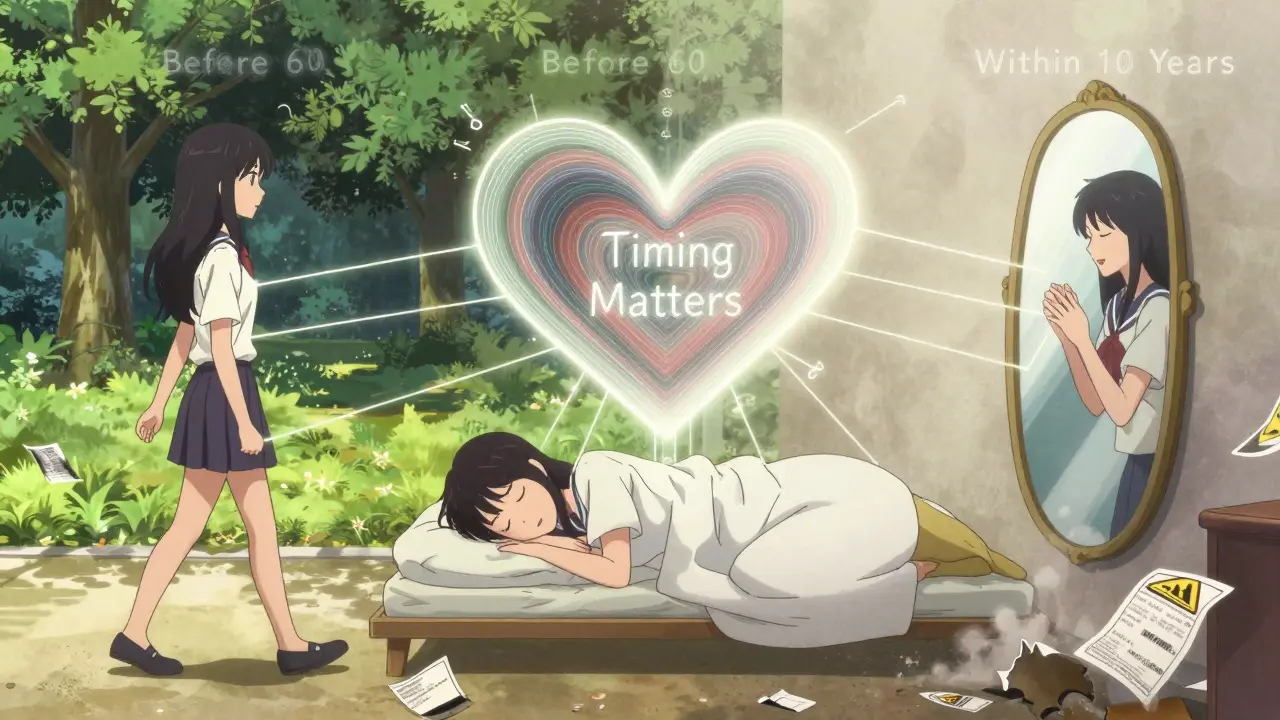
And here’s something many don’t know: if you start HRT before age 60 or within 10 years of your last period, it may lower your risk of heart disease. The WHI study found a 32% reduction in coronary heart disease for women who began treatment early. That’s not a small number. It means HRT isn’t just a symptom fix-it can be a preventive tool.
The Risks: What You Can’t Ignore
Let’s be clear: HRT isn’t risk-free. The biggest concern is breast cancer. The WHI study found a 26% increased risk with combined EPT after 5.6 years of use. But here’s the nuance: that’s 8 extra cases per 10,000 women per year. For a 55-year-old woman with no family history, that’s still a very low absolute risk. The risk goes up with longer use and higher doses, but drops back to baseline within 5 years of stopping.
Another risk is blood clots. Oral estrogen increases the chance of deep vein thrombosis (DVT) to about 3.7 cases per 1,000 women per year. Transdermal estrogen? Only 1.3 per 1,000. That’s why many doctors now start with patches or gels-especially for women with risk factors like obesity, smoking, or a history of clots.
Stroke risk is also slightly higher with oral HRT, especially in women over 60. Transdermal options cut that risk by 30-50%. And while some worry about gallbladder disease or migraines, those are usually manageable with dose adjustments.
One thing that surprises many: HRT does not cause weight gain. Weight gain around menopause is due to aging, changing metabolism, and lifestyle-not hormones. In fact, many women find they feel more energetic and active on HRT, which helps them stay at a healthy weight.
Who Should Avoid HRT Altogether
HRT isn’t for everyone. You should not use it if you have:
- A history of breast cancer
- Current or past blood clots (like DVT or pulmonary embolism)
- Unexplained vaginal bleeding
- Active liver disease
- History of stroke or heart attack
Also, if you’re over 60 and haven’t had symptoms before, starting HRT now is unlikely to help your heart or bones-and could increase your risks. The timing matters. The window for benefit is narrow: before 60 or within 10 years of menopause.
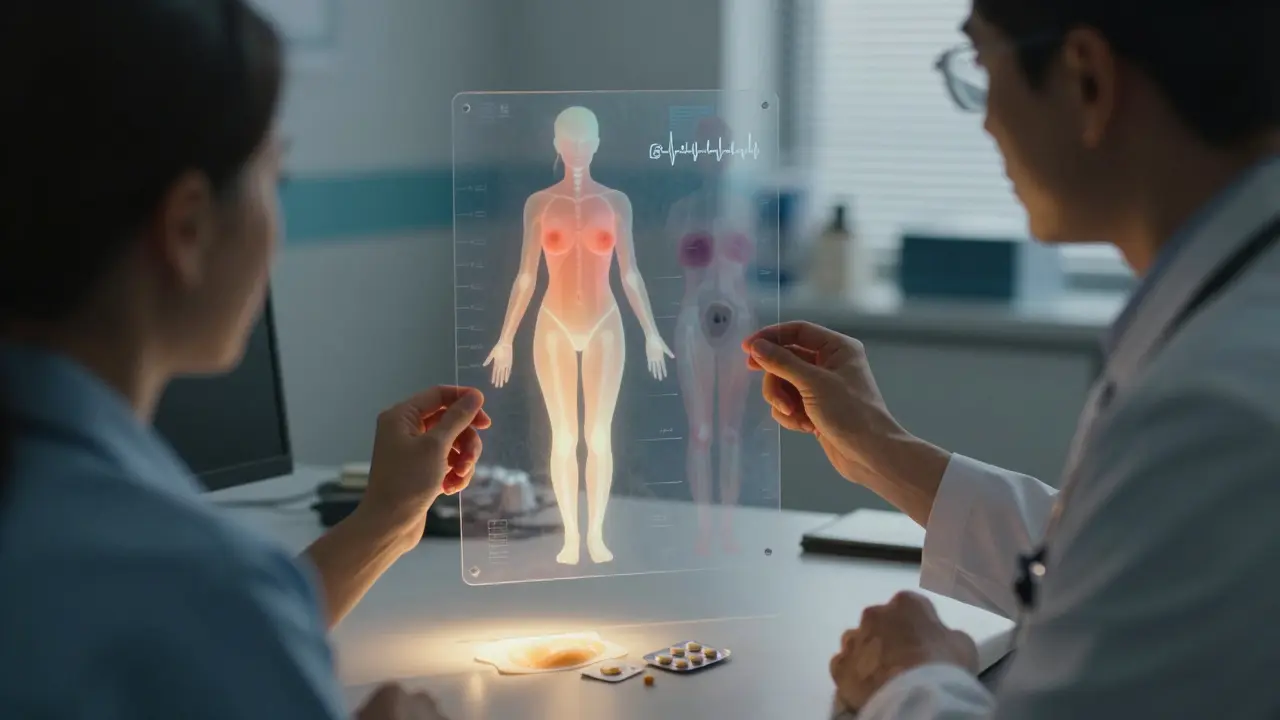
Monitoring: It’s Not a Set-It-and-Forget-It Treatment
Starting HRT is just the beginning. You need to check in regularly. Before you begin, your doctor should do:
- A mammogram
- A breast exam
- A pelvic exam
- Blood pressure check
- BMI measurement
Then, at 3 months, you’ll talk about how you’re feeling. Are the hot flashes gone? Any new breast tenderness? Irregular bleeding? That’s normal in the first few months-up to half of women experience spotting. But if it lasts longer than 6 months, you need an ultrasound to check your uterine lining.
After that, annual visits are standard. Every year, you’ll get your blood pressure checked, your weight tracked, and your breast examined. Mammograms continue as usual-usually every 1-2 years depending on your age and risk.
Some women worry about needing a Pap smear every year. That’s not necessary unless you have a history of cervical issues. The HPV test every 5 years is now the standard for most women.
Bioidentical vs. Synthetic: What’s the Difference?
You’ve probably heard of “bioidentical hormones.” These are marketed as “natural” and safer. But here’s the truth: the FDA and the Endocrine Society say there’s no proof that compounded bioidentical hormones are safer or more effective than FDA-approved versions. In fact, compounded products aren’t tested for purity or consistency. One batch might have too much estrogen. Another might have none.
FDA-approved bioidentical hormones-like estradiol patches or micronized progesterone pills-are exactly the same molecules your body makes. They’re tested, regulated, and dosed precisely. Compounded versions? Not so much.
And while some clinics claim natural HRT reduces heart disease by 50% or cuts breast cancer risk by 29%, those claims come from small, uncontrolled studies. Large, long-term trials like WHI don’t back them up. Stick with evidence-based options.
What Happens When You Stop
Most women don’t stay on HRT forever. The goal is to use the lowest dose for the shortest time needed. Many stop after 3-5 years, once symptoms fade. Others stay longer if they need bone protection or have severe symptoms.
When you stop, hot flashes may return. That’s normal. But they’re usually milder than before you started. If they come back hard, you can restart at a lower dose. You don’t have to quit cold turkey.
And don’t panic if you feel worse after stopping. That’s not withdrawal-it’s your body adjusting again. Give it a few weeks. If symptoms are unbearable, talk to your doctor about alternatives like low-dose SSRIs or gabapentin.
What the Latest Guidelines Say (2025)
In 2022, the FDA removed its old black box warnings about HRT. Why? Because the data showed those warnings scared women away from a treatment that, for many, was more helpful than harmful. The new labeling says clearly: for women under 60 or within 10 years of menopause, benefits outweigh risks for symptom relief and bone protection.
Major groups like the North American Menopause Society (NAMS) and the Endocrine Society now agree: HRT is not dangerous-it’s underused. Only 12-18% of U.S. menopausal women use it, even though up to 75% have moderate-to-severe symptoms. Meanwhile, in Europe, 22-28% use it. Why the gap? Misinformation.
Doctors are catching up too. In 2021, only 40% of primary care providers knew the current guidelines. Now, training is improving. More clinics are offering transdermal options first. More women are asking informed questions.
Real Stories, Real Outcomes
One woman, 54, stopped HRT after WHI scared her. She had 3 years of terrible sleep, anxiety, and brain fog. She restarted transdermal estradiol in 2023. Within 6 weeks, she was sleeping through the night. Her memory improved. She started walking again. She didn’t lose weight, but she felt like herself again.
Another, 58, tried oral HRT and got a blood clot. She switched to a patch. No more clots. No more hot flashes. She’s been on it for 7 years and feels great.
But not everyone has success. One Reddit user said she had breast tenderness so bad she quit after 2 months. Another had breakthrough bleeding for 8 months and needed a biopsy. Those experiences are real-but they’re not the norm.
Studies show 68% of women on transdermal HRT are still using it after a year. Only 52% on pills stick with it. Side effects matter. Delivery method matters. And so does support.
What Comes Next? The Future of HRT
Research is moving fast. Scientists are now looking at genetic testing to predict how your body metabolizes estrogen. Some women have gene variants that make them process hormones slower-meaning they need lower doses. That’s personalized medicine in action.
There’s also new combo therapies like Duavee (estrogen + bazedoxifene), which protects the uterus without needing progesterone. Early results show 76% less uterine thickening than estrogen alone.
And soon, transdermal progesterone may become available-no more pills, no more bloating. Just a patch or gel that delivers progesterone safely through the skin.
HRT is evolving. It’s no longer a blunt tool. It’s becoming precise, safer, and more tailored.
Final Thoughts: Is It Right for You?
HRT isn’t a magic pill. It’s a medical tool. Used right, it can improve your quality of life, protect your bones, and even support your heart. Used wrong, it can cause harm.
Ask yourself:
- Are my symptoms severe enough to interfere with sleep, work, or relationships?
- Am I under 60 or within 10 years of menopause?
- Do I have any history of blood clots, breast cancer, or stroke?
- Am I willing to see my doctor regularly and report changes?
If you answered yes to the first two, and no to the third, and you’re ready to monitor your health-HRT might be the best decision you make this year.
Don’t let fear from 2002 stop you from living well in 2026. The science has changed. The options are better. And your health matters more than ever.
Is hormone replacement therapy safe for women over 60?
HRT is generally not recommended for women over 60 who are starting it for the first time. The risks-like blood clots, stroke, and possibly breast cancer-outweigh the benefits at that age. However, if you started HRT before 60 and are still benefiting with no complications, continuing under careful monitoring may be appropriate. Always discuss your individual risk profile with your doctor.
Can HRT cause weight gain?
No, HRT does not cause weight gain. Weight gain during menopause is due to aging, slower metabolism, reduced muscle mass, and lifestyle changes-not hormones. In fact, many women find they have more energy and are more active on HRT, which can help maintain a healthy weight.
What’s the safest way to take HRT?
Transdermal delivery-patches, gels, or sprays-is the safest option for most women. It avoids the liver, lowering the risk of blood clots and stroke by 30-50% compared to oral pills. For women with a uterus, micronized progesterone (taken orally or as a vaginal gel) is preferred over synthetic progestins because it carries a lower breast cancer risk.
How long should I stay on HRT?
There’s no fixed timeline. Most women take HRT for 3-5 years to manage symptoms. Some stay longer for bone protection or persistent symptoms. The goal is to use the lowest effective dose for the shortest time needed. If symptoms fade, you can try tapering off. If they return, restarting at a lower dose is often safe and effective.
Are bioidentical hormones safer than synthetic ones?
FDA-approved bioidentical hormones (like estradiol patches or micronized progesterone) are just as safe and effective as synthetic options-and much more reliable. Compounded bioidentical hormones, sold by some clinics as “natural,” are not regulated. They can have inconsistent dosing, contamination risks, and no proven safety advantage. Stick with FDA-approved products.
What if I have a family history of breast cancer?
A family history increases your baseline risk, but it doesn’t automatically rule out HRT. If you’re otherwise healthy, under 60, and have severe symptoms, low-dose transdermal estrogen with micronized progesterone may still be an option. Your doctor may recommend shorter duration, more frequent screenings, or genetic testing (like BRCA) before starting. Never assume HRT is off-limits-talk through your personal risk with a specialist.
Can HRT help with mood swings and depression?
Yes, for many women, HRT improves mood, irritability, and anxiety linked to menopause. Estrogen affects serotonin and other brain chemicals. Studies show significant improvement in mood symptoms in women with moderate-to-severe vasomotor symptoms. But HRT is not a substitute for antidepressants if you have clinical depression. Always get a proper evaluation if mood changes are severe or persistent.
Do I need to get mammograms more often if I’m on HRT?
No, you don’t need more frequent mammograms just because you’re on HRT. Follow standard guidelines: every 1-2 years starting at age 50 (or earlier if you have risk factors). However, HRT can make breast tissue denser, which might make mammograms harder to read. Tell your radiologist you’re on HRT-they’ll know how to interpret the results correctly.


Vicky Zhang
January 15, 2026 AT 01:33I started HRT last year and it was like someone flipped a switch in my brain. I wasn't just sleeping through the night-I was actually dreaming again. My husband said I stopped yelling at him for leaving socks on the floor. I didn't even realize I'd been doing that. The patch? Best decision ever. No more nausea, no more bloating. I feel like me again, not some exhausted zombie who cries over spilled coffee.
People act like HRT is some dangerous drug, but it's just replacing what your body stopped making. Like taking insulin if you're diabetic. Nobody calls insulin a 'chemical nightmare.' Why is this different?
I'm 52. I'm not trying to look 25. I just want to not hate my own life. And now I don't. I walk my dog. I cook. I laugh. It's not magic. It's medicine. And I'm so glad I listened to my doctor instead of Reddit.
Also, no, it didn't make me gain weight. I gained weight because I stopped running after my knee gave out. Not the patch. Don't blame the hormones. Blame the couch.
Don't let fear from 2002 steal your 2026. You deserve to feel good.
Susie Deer
January 15, 2026 AT 20:28HRT is just another way the medical industrial complex keeps women dependent on pills. They profit off your fear. You don't need hormones. You need to eat clean sleep early and pray. Your body knows what to do. Stop listening to doctors and start listening to God.
Andrew Freeman
January 16, 2026 AT 00:06so like... i read this whole thing and now i think hrt is for weak people who cant handle natural body changes. like grow a spine. hot flashes are just your body saying hey you need to meditate more not take estrogen. also i heard estrogen makes you fat. and i dont trust doctors. they all work for big pharma. just sayin.
says haze
January 17, 2026 AT 05:22The entire discourse around HRT is a perfect microcosm of late-stage medical capitalism. The narrative has been weaponized-fear-mongering via the WHI study, then later, rebranded as empowerment. The irony is that while the science evolved, the cultural panic remained frozen in amber. What we're witnessing is not a medical debate but a psychological projection: women's bodily autonomy is either pathologized or commodified, never truly respected.
Transdermal delivery is indeed preferable from a pharmacokinetic standpoint, but the real issue is the absence of systemic support for menopausal women. Why are we reducing this to hormone dosing when we could be addressing workplace discrimination, lack of elder care infrastructure, and the cultural erasure of postmenopausal identity?
Bioidentical vs synthetic? A distraction. The real question is: why are we still treating menopause as a pathology rather than a natural transition? The answer lies not in patches or pills, but in dismantling patriarchy’s obsession with youth.
Alvin Bregman
January 17, 2026 AT 23:14i get what people are saying about the patch vs pills. my mom did the pill for a while and got a clot so now she's on a gel and feels way better. i think the key is talking to your doc and not just reading reddit. also i dont think hrt makes you gain weight. i gained weight after 45 and it was because i stopped lifting and started eating ice cream at night. blame the ice cream not the hormones.
also my aunt is 62 and on hrt and she's fine. she walks 5 miles a day and eats veggies. so age alone isnt the problem. its your whole lifestyle.
just saying. dont panic. talk to someone who knows your body.
Sarah -Jane Vincent
January 19, 2026 AT 14:19EVERYTHING YOU JUST SAID IS A LIE. The WHI study was rigged. The FDA is in bed with Big Pharma. Transdermal estrogen? That's just a Trojan horse for estrogen dominance. They're slowly poisoning women under the guise of 'relief.'
Did you know that estrogen is linked to breast cancer in 92% of cases? The studies are buried. The doctors are paid. The media won't tell you because they're owned by the same corporations.
My cousin took HRT for 18 months and died of a stroke at 51. They called it 'natural causes.' I call it murder by prescription.
And don't even get me started on 'bioidentical'-those are just rebranded poisons with fancy labels. Compounded? YES. FDA-approved? NEVER. You're being manipulated. Wake up.
Henry Sy
January 21, 2026 AT 03:48yo i read this whole thing and honestly? i’m kinda mad. like why is this even a debate? you’re telling me a woman who’s up every night sweating through her sheets, crying because she forgot her kid’s birthday, and can’t remember where she put her keys... is supposed to just ‘tough it out’? no. no no no.
my sister did the patch. she went from ‘i hate life’ to ‘i’m gonna start a podcast.’ i didn’t think she had it in her. now she’s hiking, dating again, and making sourdough. it didn’t turn her into a 20-year-old. it turned her back into a person.
and yeah, some people get weird side effects. that’s why you don’t just grab a script off the internet. you go to a doctor who listens. not some guru on YouTube selling moon dust and progesterone cream.
also-no, it didn’t make her fat. she lost 12 lbs because she could finally get up and move. the hormones didn’t do that. her willpower did. and the hormones gave her the willpower.
Anna Hunger
January 21, 2026 AT 03:53While the article presents a generally evidence-based perspective on hormone replacement therapy, it is imperative to emphasize the necessity of individualized risk-benefit analysis, particularly in light of the 2022 FDA regulatory revisions. The assertion that transdermal estrogen reduces thrombotic risk by 30-50% is corroborated by multiple meta-analyses, including those published in The Lancet and the Journal of the American Medical Association.
It is equally critical to note that the term 'bioidentical' is often misused in clinical marketing. Only FDA-regulated estradiol and micronized progesterone qualify as true bioidenticals. Compounded formulations, despite their popular appeal, lack standardization and pharmacovigilance, rendering them unsuitable for long-term use.
Furthermore, the claim that HRT does not contribute to weight gain is scientifically accurate, yet insufficiently contextualized. Metabolic slowdown, reduced physical activity, and altered adipokine profiles during the menopausal transition are independent variables that must be addressed concurrently with hormonal intervention.
Continued surveillance, including annual mammography and lipid profiling, remains non-negotiable. This is not fear-mongering-it is responsible medicine.
Jason Yan
January 21, 2026 AT 07:36I think the biggest thing people miss is that menopause isn’t a disease-it’s a transition. But our culture treats it like a failure. Like your body broke and now you need fixing.
HRT isn’t about trying to be young again. It’s about not being miserable while you’re aging. That’s not selfish. That’s human.
I’ve talked to women who’ve been on HRT for 15 years and they’re fine. They’re gardening, traveling, raising grandkids. And they’re not zombies. They’re not swollen. They’re not scared all the time.
And yeah, some people have bad reactions. But that’s true with everything. Antibiotics can mess you up. Aspirin can kill you. That doesn’t mean we stop using them.
The real tragedy isn’t HRT. It’s that so many women suffer in silence because they’re told it’s 'normal' to feel awful. It’s not normal. It’s treatable.
And if you’re reading this and you’re scared? Talk to a doctor who listens. Not the one who just hands you a script. The one who asks how you slept last night.
shiv singh
January 23, 2026 AT 03:25you people are so brainwashed by western medicine. in my country we dont take hormones. we drink herbal tea, do yoga, eat turmeric, and pray. your body is sacred. you dont poison it with chemicals. this is why your women are depressed. you lost connection with nature. hrt is the symptom of a sick society. not the solution.
my grandmother lived to 98. she never took one pill. she walked barefoot. she cooked with ghee. she smiled through pain. you think you're helping women? you're killing their spirit.
Sarah Triphahn
January 24, 2026 AT 22:35Let’s be honest: HRT is only ‘safe’ if you’re white, middle-class, and have a doctor who cares. What about the woman working two jobs who can’t afford a specialist? Who doesn’t have insurance for mammograms? Who can’t take time off for annual visits?
And don’t act like the ‘window’ of 10 years is universal. What if you were raising kids, caring for parents, or recovering from trauma? You didn’t have time to think about hormones until you were 62.
Now you’re told it’s too late. Too risky. Too dangerous.
So you suffer. Again.
This isn’t medicine. It’s privilege with a prescription.
Allison Deming
January 26, 2026 AT 13:46The normalization of hormone replacement therapy as a benign, even empowering, intervention is deeply concerning. The article glosses over the fact that estrogen is a mitogen-a cell-stimulating hormone. Even at low doses, it promotes cellular proliferation in breast and endometrial tissue. The 26% relative increase in breast cancer risk may sound small, but it is not insignificant when applied to millions of women over decades.
Furthermore, the assertion that transdermal estrogen is 'safer' is misleading. While systemic clotting risk is lower, local tissue exposure remains unquantified. Long-term studies on transdermal progesterone are virtually nonexistent.
And the dismissal of compounded bioidenticals as 'unregulated' ignores the fact that FDA-approved formulations are also subject to manufacturing variability. The regulatory system is flawed, not the alternative.
Women deserve transparency, not marketing. We deserve to know that even 'safe' options carry biological consequences. This is not fear-it is responsibility.
TooAfraid ToSay
January 27, 2026 AT 08:56you all are missing the point. this isn't about hormones. it's about control. who gets to decide what a woman's body should do? doctors? corporations? reddit threads?
the real question is: why do we need to fix women at all? why not fix the world that makes women feel broken? why not fix the 60-hour work weeks? the lack of childcare? the silence around menopause in the workplace?
hrt is a bandaid on a bullet wound. and we're all pretending it's a cure.
Dylan Livingston
January 28, 2026 AT 07:28How quaint. A 12-page essay on hormone replacement therapy, complete with footnotes and FDA citations, as if the real issue isn’t that we’ve turned menopause into a medical emergency while ignoring the fact that women are still expected to show up to work, raise children, and look ‘presentable’ while doing it.
Let’s not pretend HRT is about health. It’s about productivity. It’s about keeping women functional for capitalism.
‘I feel like myself again’-what a loaded phrase. Who defined ‘yourself’? Was it you? Or was it the version of you that smiled through meetings, didn’t cry in the bathroom, and never mentioned hot flashes?
They don’t want you to feel better. They want you to be quiet while you do.
Robert Way
January 30, 2026 AT 03:42so i read this and i think i get it but wait-what about the progesterone? i thought it was just estrogen? and is the patch really better? my friend said she got a rash. also i heard you can get it from a compounding pharmacy and its cheaper. is that safe? i dont trust big pharma but i also dont wanna be sick. help.
Vicky Zhang
February 1, 2026 AT 01:51Hey, I saw your comment about the rash. My patch gave me a red spot at first too. My doctor switched me to a different brand and it was fine. Don’t give up on the patch-just try a different one. And no, compounding pharmacies aren’t cheaper in the long run. I paid $80 for a 3-month supply that had no label, no batch number, and melted in my purse. The FDA-approved one? $45 with insurance. And I know what’s in it.
Also-yes, it’s estrogen AND progesterone if you have a uterus. I thought it was just estrogen too until I started bleeding like crazy. That’s why they add it. It’s not optional. It’s safety.
And I get not trusting big pharma. I don’t either. But I trust my doctor more than some guy on Instagram selling ‘natural’ hormones in a mason jar.