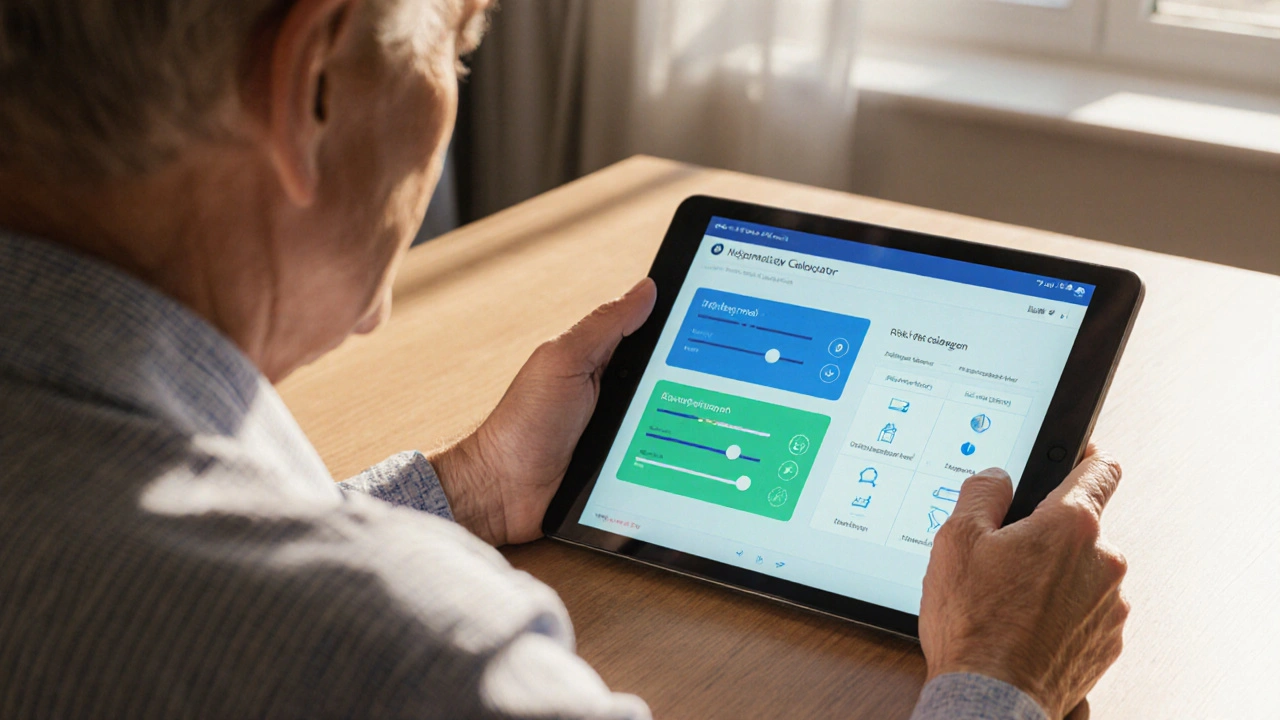
COPD Heart Disease Risk Calculator
Your COPD Risk Factors
Enter information about your COPD status and lifestyle factors to see how they affect your heart disease risk.
Key Facts
- COPD increases heart disease risk by 30-40%
- Inflammation and low oxygen levels are major causes
- Smoking and sedentary lifestyle worsen both conditions
Risk Assessment Form
Your Risk Results
Enter your details and click "Calculate Your Risk" to see your personalized risk assessment.
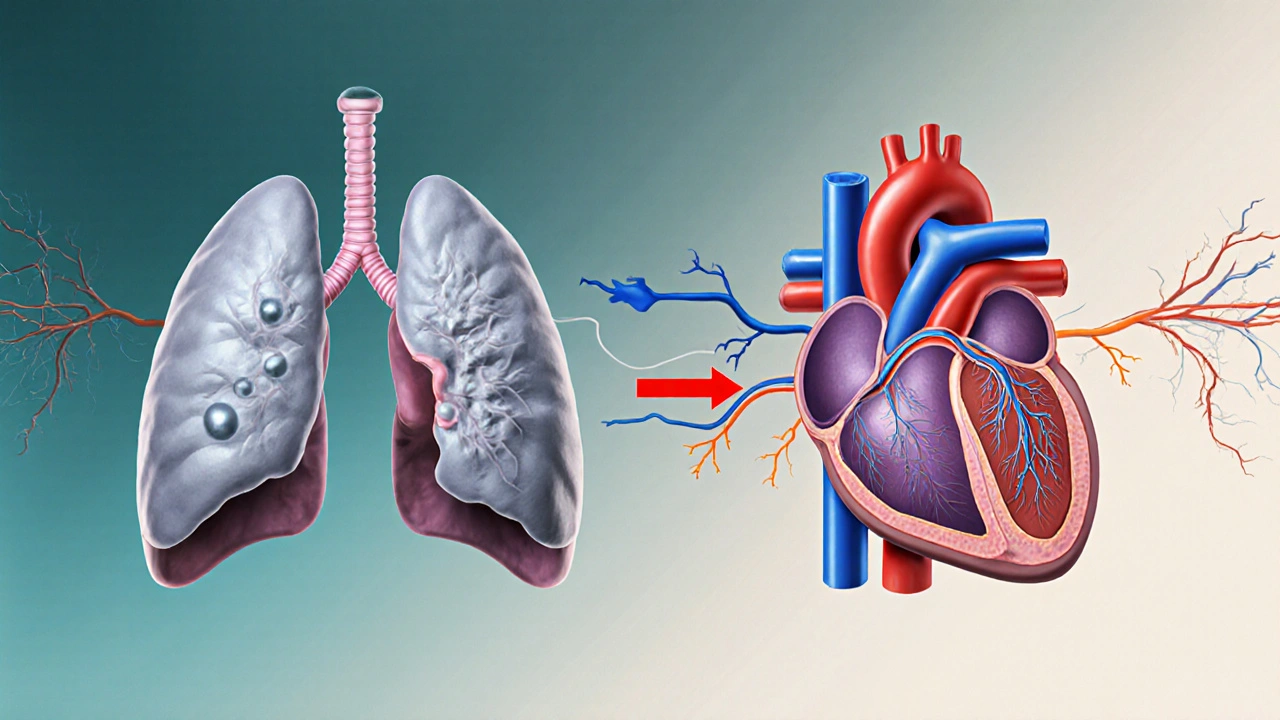
How COPD Affects Heart Health
COPD increases heart disease risk through multiple pathways:
- Inflammation: Chronic lung inflammation spreads to the cardiovascular system
- Low Oxygen Levels: Hypoxia forces the heart to work harder
- Right Heart Strain: Increased pressure in lung arteries affects the right side of the heart
- Shared Risk Factors: Smoking, lack of exercise, and poor diet contribute to both conditions
Quick Take
- COPD raises the chance of heart disease by 30‑40%.
- Inflammation, low oxygen and strain on the right heart are the main culprits.
- Smoking, lack of activity and poor diet feed both illnesses.
- Regular lung and heart tests can catch problems early.
- Targeted meds, exercise and quit‑smoking programs improve outcomes.
What is Obstructive Pulmonary Disease?
Obstructive Pulmonary Disease is a group of chronic lung disorders, most commonly chronic obstructive pulmonary disease (COPD), that cause airflow limitation and make breathing hard. The condition typically develops after years of exposure to irritants like tobacco smoke, dust, or chemicals. According to the World Health Organization, about 251million people worldwide live with COPD, and it claims roughly 3million deaths each year.
The disease progresses through three stages-mild, moderate and severe-based on spirometry results (FEV1/FVC<0.70). Symptoms include chronic cough, mucus production, and shortness of breath, especially during exertion.
What is Heart Disease?
Heart disease refers to any condition that impairs the heart’s ability to pump blood effectively, including coronary artery disease, heart failure, arrhythmias and valve problems. In Australia, heart disease is the leading cause of death, responsible for one in five fatalities.
Cardiovascular disease (CVD) often begins with atherosclerosis-plaque buildup inside arteries-leading to reduced blood flow, chest pain, and eventually heart attacks or chronic heart failure.
How the Two Conditions Interact
Researchers have identified several pathways that tie COPD to heart disease:
- Systemic Inflammation: COPD triggers chronic release of inflammatory markers (CRP, IL‑6, TNF‑α). These circulate in the bloodstream, accelerating arterial plaque formation.
- Chronic Hypoxia: Persistently low oxygen levels force the heart to work harder, especially the right ventricle, which can develop pulmonary hypertension and right‑sided heart failure.
- Oxidative Stress: Smoke‑related free radicals damage both lung tissue and blood vessel walls, promoting atherosclerosis.
- Autonomic Imbalance: COPD flare‑ups raise sympathetic activity, raising heart rate and blood pressure, which strain the heart.
COPD and heart disease share several biological pathways that amplify each other's damage.
Shared Risk Factors
Many lifestyle and environmental factors increase the odds of developing both diseases:
| Risk Factor | Impact on COPD | Impact on Heart Disease |
|---|---|---|
| Smoking | Primary cause; damages airway walls | Accelerates atherosclerosis and raises blood pressure |
| Air Pollution | Triggers exacerbations | Linked to arterial plaque and hypertension |
| Physical Inactivity | Worsens dyspnea, reduces lung capacity | Promotes obesity, raises cholesterol |
| Obesity | Increases breathlessness | Raises strain on heart, leads to diabetes |
| Diabetes | Associated with higher COPD mortality | Damages blood vessels, raises heart failure risk |
Recognizing Overlapping Symptoms
Because both illnesses affect breathing and energy levels, patients often misinterpret warning signs. Look for these red flags that suggest heart involvement:
- Swelling in ankles or lower legs (sign of right‑heart strain).
- Chest tightness that worsens when lying flat.
- Sudden worsening of breathlessness at rest, not explained by a COPD flare‑up.
- Palpitations or irregular heartbeats.
If any of these appear, a cardiac evaluation should follow the pulmonary assessment.
Diagnosis and Monitoring
Effective care requires coordinated testing:
- Spirometry: Confirms airflow limitation; helps stage COPD.
- Pulse Oximetry & Arterial Blood Gases: Detect chronic hypoxia.
- Echocardiogram: Assesses right‑ventricular pressure and overall heart function.
- CT Scan of Chest: Can reveal pulmonary hypertension and emphysema extent.
- Blood Tests: CRP, lipid profile, HbA1c to gauge inflammation, cholesterol and diabetes control.
Regular monitoring-every 6‑12months for stable patients-allows early detection of cardiac changes.
Managing Both Conditions
Therapy must address the lungs, the heart, and the shared risk factors.
Medication Strategies
- Bronchodilators (LABA/LAMA): Improve airflow, reduce COPD exacerbations.
- Inhaled Corticosteroids: Lower lung inflammation but watch for increased infection risk.
- Statins: Proven to lower cardiovascular events and may reduce COPD‑related inflammation.
- ACE Inhibitors or ARBs: Helpful for hypertension and can improve right‑ventricular function.
- Diuretics: Manage fluid buildup in heart failure, especially if pulmonary edema develops.
Lifestyle Interventions
- Quit Smoking: The single most effective step; nicotine replacement or varenicline can double success rates.
- Pulmonary Rehabilitation: Combines exercise, breathing techniques, and education; also improves cardiac fitness.
- Heart‑Healthy Diet: Emphasize fruits, vegetables, whole grains, lean protein, and limit sodium.
- Regular Physical Activity: Aim for 150minutes of moderate aerobic exercise weekly, adjusted for lung capacity.
Prevention Checklist
- Schedule annual spirometry and blood pressure checks.
- Track oxygen saturation at home during flare‑ups.
- Maintain a healthy BMI (18.5‑24.9kg/m²).
- Vaccinate against flu and pneumococcal disease to avoid respiratory infections.
- Use a peak flow meter to spot early lung function decline.
- Discuss statin therapy with your doctor if you have high cholesterol or a history of COPD exacerbations.
- Enroll in a quit‑smoking program within 30days of diagnosis.

Frequently Asked Questions
Can COPD cause a heart attack?
Yes. The chronic inflammation and low‑oxygen environment in COPD accelerate atherosclerosis, raising the likelihood of a myocardial infarction, especially in smokers.
Is pulmonary hypertension the same as heart failure?
No. Pulmonary hypertension is high blood pressure in the lungs’ arteries, often a consequence of COPD. Over time it can strain the right ventricle and lead to right‑sided heart failure.
Do inhaled steroids increase heart risk?
Evidence suggests inhaled steroids do not raise cardiovascular risk and may actually lower systemic inflammation, though high doses should be monitored for infections.
How often should I see a cardiologist if I have COPD?
If you have moderate‑to‑severe COPD or any cardiac symptoms, an annual cardiology review is advisable. Otherwise, a check‑up every 2‑3years may suffice.
Can exercise worsen my breathing?
When guided by a pulmonary rehab program, exercise actually strengthens respiratory muscles and improves oxygen utilization, reducing breathlessness over time.

John Petter
October 1, 2025 AT 22:00COPD definitely ups your heart risk.
Annie Tian
October 9, 2025 AT 06:28The link between COPD and cardiac events is striking; inflammation seeps into the vasculature, and low oxygen forces the heart to overwork. Keep tracking those numbers, and stay proactive-your lungs and heart thank you!
April Knof
October 16, 2025 AT 14:56From a global health standpoint, COPD remains a leading cause of morbidity across continents, and its cardiovascular sequelae echo the same pattern worldwide. Recognizing cultural lifestyle factors can help tailor prevention strategies beyond the typical Western focus.
Tina Johnson
October 23, 2025 AT 23:25Empirical studies indicate that patients with moderate to severe COPD exhibit a 30‑40 % increase in myocardial infarction incidence, a fact corroborated by longitudinal cohorts. Ignoring this data undermines evidence‑based practice, and clinicians must integrate cardiopulmonary monitoring into standard care.
Sharon Cohen
October 31, 2025 AT 06:53Seems like everyone’s shouting about the risk, yet I’m not convinced the numbers are as dire as advertised.
Rebecca Mikell
November 7, 2025 AT 15:21Great summary! It’s helpful to see the mechanisms laid out clearly, and it reminds us that lifestyle adjustments can truly mitigate risk.
Ellie Hartman
November 14, 2025 AT 23:49I appreciate the concise breakdown; it encourages me to ask my doctor about targeted exercises that support both lung capacity and heart health.
Alyssa Griffiths
November 22, 2025 AT 08:17What if the pharmaceutical industry is downplaying the true heart danger to keep us dependent on inhalers?; the data might be selectively reported, and we should stay skeptical.
Cierra Nakakura
November 29, 2025 AT 16:46Love the interactive tool! 🎉 It makes the abstract numbers feel personal, and seeing the impact of quitting smoking right away is super motivating. Keep the updates coming! 👍
Sharif Ahmed
December 7, 2025 AT 01:14Alas, the mere mention of risk percentages fails to capture the tragic poetry of a heart laboring under suffocating breath; we must elevate discourse beyond bland statistics.
Charlie Crabtree
December 14, 2025 AT 09:42Super helpful! 😄 Knowing that a simple tweak in daily activity can shave off risk points makes me want to hit the park tomorrow. Thanks for the clear guide!
RaeLyn Boothe
December 21, 2025 AT 18:10While enthusiasm is admirable, remember that incremental changes seldom produce dramatic outcomes without sustained commitment.
Fatima Sami
December 29, 2025 AT 02:39Correction: the phrase “low oxygen forces the heart to overwork” should be phrased as “hypoxia imposes increased workload on the heart.” Accuracy matters.
Arjun Santhosh
January 5, 2026 AT 11:07lol i think the calculator is cool but kinda confusing sometimes.. maybe add some tooltips?
Stephanie Jones
January 12, 2026 AT 19:35When one contemplates the intimate dialogue between lung and heart, it becomes evident that disease is not merely a collection of isolated symptoms, but a narrative of systemic imbalance. COPD, in its relentless constriction of airflow, initiates a cascade of hypoxic stress that reverberates through the circulatory system. The heart, ever the diligent sentinel, compensates by elevating cardiac output, a physiological adaptation that, over time, exacts a toll on myocardial tissue. Inflammation, the silent architect of vascular degeneration, spreads from pulmonary alveoli to arterial walls, eroding endothelial integrity. Consequently, atherosclerotic plaques find fertile ground, accelerating the march toward coronary artery disease. Moreover, the right ventricle, tasked with propelling blood through obstructed pulmonary arteries, undergoes hypertrophic remodeling, a condition known as cor pulmonale, further straining cardiac function. Lifestyle choices, such as tobacco use and sedentary habits, serve as accelerants, amplifying both pulmonary and cardiac deterioration. Yet, within this bleak tableau lies agency: smoking cessation restores microvascular function, and regular aerobic exercise enhances oxygen delivery, attenuating hypoxic signaling. Psychological resilience also plays a subtle role, modulating neurohormonal pathways that influence inflammation. It is therefore insufficient to view COPD and heart disease as parallel epidemics; they are intertwined threads of a single tapestry of health. Preventive medicine must adopt a holistic lens, addressing respiratory therapy, cardiovascular monitoring, and behavioral counseling in concert. Only through such integrative stewardship can we hope to disrupt the feedback loop of damage. As clinicians and patients alike internalize this interconnectedness, the prospect of reducing morbidity transforms from a distant ideal into a tangible objective. Let us, therefore, champion interdisciplinary care, lest we allow compartmentalized treatment to perpetuate hidden harms. In the end, the heart’s rhythm is a reflection of the lungs’ breath, and harmony between them is the epitome of vitality.
Nathan Hamer
January 20, 2026 AT 04:03Indeed, the cascade from airway obstruction to cardiac strain reads like a tragic play; each inhalation echoes a heartbeat, each exhalation a sigh of the left ventricle. 🌬️❤️ Embrace the data, act on it, and rewrite the script! 🚀
Tom Smith
January 27, 2026 AT 12:32Ah, a lyrical soliloquy on hypoxia-how original. Perhaps next you’ll compose an ode to cholesterol?
Kyah Chan
February 3, 2026 AT 21:00After exhaustive review of the presented calculator, I must conclude that the methodology suffers from oversimplification, lacking multivariate adjustment for comorbidities. The absence of peer‑reviewed validation renders the tool academically dubious.