Quick Takeaways
- Spironolactone blocks aldosterone, reducing sodium retention and lowering blood pressure.
- It works best when combined with other antihypertensive agents.
- Regular monitoring of potassium and kidney function is essential.
- Common side effects include mild hormone‑related changes and increased potassium.
- Patients with severe kidney disease should avoid it unless closely supervised.
What Is Spironolactone?
When doctors treat high blood pressure, Spironolactone is an aldosterone antagonist diuretic that interferes with the body’s ability to hold onto salt and water. By doing so, it helps the cardiovascular system stay relaxed and the blood vessels widen.
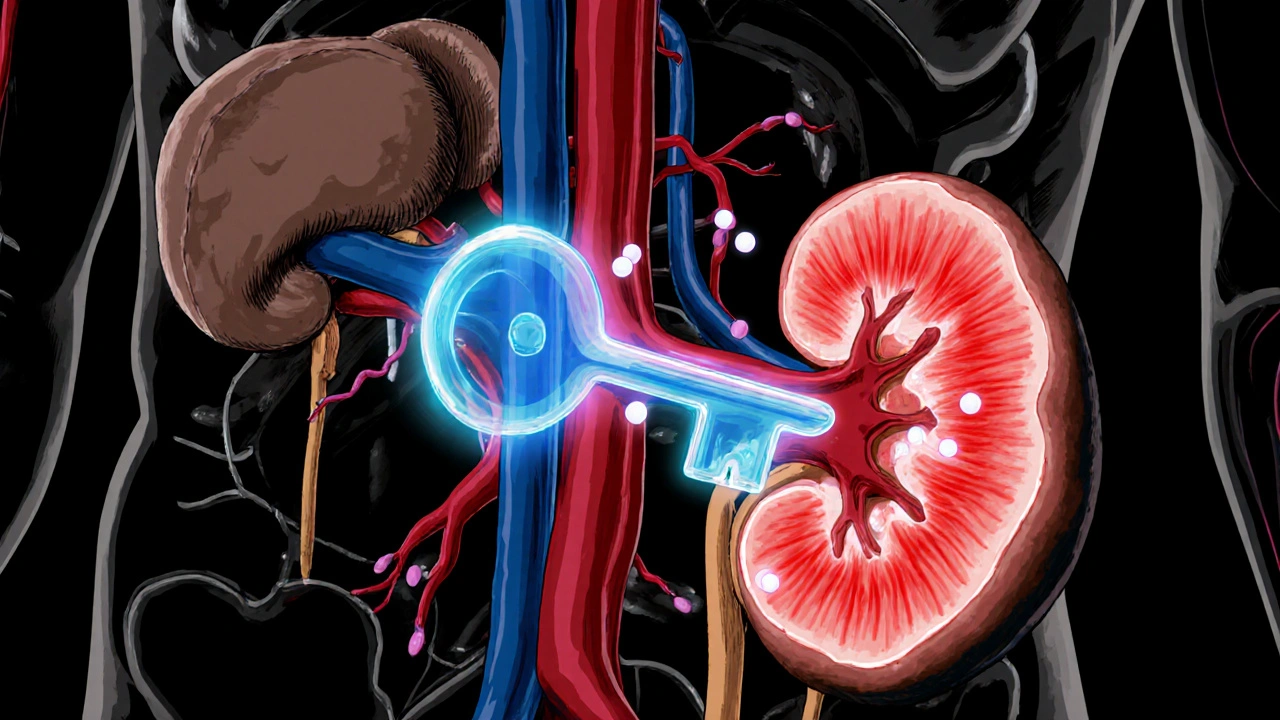
Why Aldosterone Matters for Blood Pressure
The hormone Aldosterone is produced in the adrenal glands and tells the kidneys to re‑absorb sodium while shedding potassium. More sodium means more water stays in the bloodstream, which pushes up the pressure against vessel walls. In people with Hypertension, this system often runs too hot, leading to chronic high readings.
How Spironolactone Interrupts the Renin‑Angiotensin‑Aldosterone System (RAAS)
The RAAS is a loop that starts with the kidneys sensing low blood flow. They release renin, which converts angiotensinogen into angiotensin I, then into angiotensin II. Angiotensin II narrows blood vessels and triggers aldosterone release. Spironolactone blocks aldosterone’s receptor, preventing the final step of sodium re‑absorption. The result is less fluid volume, lower vascular resistance, and a drop in blood pressure.
Clinical Scenarios Where Spironolactone Shines
Doctors often reserve spironolactone for patients who:
- Have resistant hypertension-blood pressure stays high despite three drugs from different classes.
- Show signs of primary aldosteronism, a condition where excess aldosterone drives the problem.
- Need additional potassium‑sparing effects because they’re already on a thiazide diuretic.
In these cases, adding spironolactone can cut systolic numbers by 10‑15 mm Hg, a clinically meaningful reduction.
Comparison With Other Diuretics
| Feature | Spironolactone | Thiazide Diuretics |
|---|---|---|
| Mechanism | Aldosterone receptor blocker | Inhibits sodium‑chloride transporter in distal tubule |
| Potassium Effect | Spares potassium (risk of hyper‑kalemia) | Can cause potassium loss (hypokalemia) |
| Typical Use | Resistant hypertension, primary aldosteronism | First‑line for uncomplicated hypertension |
| Common Side Effects | Gynecomastia, menstrual irregularities, hyper‑kalemia | Elevated uric acid, low potassium, glucose intolerance |
| Monitoring Needs | Serum potassium, renal function every 1-2 months initially | Electrolytes mainly potassium, less frequent |
Safety Checklist Before Starting Therapy
- Check baseline serum potassium and creatinine. Values above 5.0 mmol/L or eGFR below 30 mL/min/1.73 m² usually rule out use.
- Review current medications. ACE inhibitors, ARBs, or potassium supplements increase hyper‑kalemia risk.
- Discuss hormone‑related side effects. Women may notice breast tenderness; men might experience gynecomastia.
- Plan follow‑up labs at 2 weeks, then monthly for the first quarter.
- Set realistic blood pressure goals - typically <130/80 mm Hg for most adults with cardiovascular risk.
Managing Common Side Effects
If a patient notices mild breast tenderness, a temporary dose reduction often helps. For more pronounced gynecomastia, switching to eplerenone-a similar blocker with fewer hormonal effects-can be an option.
Elevated potassium can be tamed by lowering the dose, adding a low‑dose thiazide, or advising a diet lower in high‑potassium foods such as bananas and oranges.
Regular exercise and a balanced diet support the medication’s pressure‑lowering effect without adding extra strain on the kidneys.

What to Expect After Starting Spironolactone
Most patients notice a gradual drop in blood pressure within two weeks. The drug’s half‑life is about 1.5 hours, but its active metabolites linger for up to 10 days, which is why steady effects appear slowly.
Because spironolactone works best when paired with agents that block other parts of the RAAS-like ACE inhibitors or ARBs-doctors often prescribe it as a third‑line drug after a calcium‑channel blocker and a thiazide.
Special Populations
Pregnant Women: Spironolactone is generally avoided due to potential anti‑androgen effects on the fetus.
Elderly Patients: Kidney function tends to decline with age, so lower starting doses (12.5 mg daily) and close lab monitoring are prudent.
Patients with Diabetes: They already face higher potassium retention; a cautious approach is necessary, especially if they’re on ACE inhibitors.
Frequently Asked Questions
Can spironolactone be used alone for hypertension?
It can be used alone, but guidelines usually recommend it as an add‑on after a thiazide, calcium‑channel blocker, or ACE inhibitor because the combined effect is stronger.
How often should blood tests be done?
First check at 2 weeks, then monthly for three months, and every 3-6 months thereafter, unless kidney function changes.
What foods should I avoid?
Limit high‑potassium foods like bananas, oranges, potatoes, and tomatoes while you’re on the drug. Stay hydrated and keep sodium moderate.
Is it safe to take with an ACE inhibitor?
Yes, the combination is common and often more effective, but it raises hyper‑kalemia risk, so lab checks become critical.
What is the difference between spironolactone and eplerenone?
Both block aldosterone, but eplerenone is more selective and causes fewer hormone‑related side effects, though it can be pricier.
Bottom Line
For people struggling to tame stubborn blood pressure, spironolactone offers a unique way to knock down sodium, keep kidneys happy, and let the heart relax. Pair it with the right companions, watch the labs, and you’ll likely see a steady improvement without dramatic swings.

Jennifer Stubbs
October 25, 2025 AT 14:55Spironolactone’s potassium‑sparing effect is a double‑edged sword; while it helps avoid hypokalemia, you still have to watch labs like a hawk. In resistant hypertension it can shave 10‑15 mm Hg off systolic numbers, which is clinically meaningful. However, the hormone‑related side effects aren’t trivial-gynecomastia in men and menstrual irregularities in women can affect adherence. Pairing it with an ACE inhibitor or ARB amplifies hyper‑kalemia risk, so dose adjustments are a must. Bottom line: it works, but only if you respect the monitoring checklist.
Abhinav B.
October 25, 2025 AT 17:09Listen, using spironolactone without checking k+ first is like driving without brakes-dangerous!!! The drug blocks aldosterone so you cant hold onto sodium, but if your kidneys are already weak you’ll end up with potasium overload quick. Make sure your eGFR is above 30 and your potassium is under 5 before you even think about starting. Also, dont mix it with other potassium‑sparing meds unless your doc is on top of it.
Lindy Hadebe
October 25, 2025 AT 19:22Honestly, if you can’t even keep track of a simple lab test, you’re not cut out for spironolactone.
Abby W
October 25, 2025 AT 21:35😂 Totally feel you on the “no brakes” vibe! Just a heads‑up: some folks get mild breast tenderness and it can be a real mood‑killer 🙁. Keep those potassium checks on the calendar and you’ll dodge most drama.
Lisa Woodcock
October 25, 2025 AT 23:49Thanks for breaking it down so clearly! I’ve been on spironolactone for a few months and the regular blood work really gave me peace of mind. The side‑effects were manageable, and I’ve noticed my BP finally staying in the right zone. It helped me feel less “on edge” about my numbers.
Sarah Keller
October 26, 2025 AT 02:02Spironolactone illustrates a fascinating paradox in modern pharmacology: a molecule that both simplifies and complicates the management of hypertension. By antagonizing the aldosterone receptor, it directly interrupts the final act of the RAAS cascade, thereby reducing sodium re‑absorption and expanding intravascular volume. This mechanistic clarity gives clinicians a powerful lever, especially when conventional agents fail to achieve target pressures. Yet the very simplicity of its target masks a web of downstream consequences that demand vigilant oversight. Hyper‑kalemia, for instance, is not merely a lab anomaly; it can precipitate arrhythmias that jeopardize life. Moreover, the hormonal spillover into estrogenic pathways can manifest as gynecomastia in men or menstrual disturbances in women, disturbing quality of life. The ethical dimension emerges when we consider prescribing this drug to patients whose renal function hovers near the threshold-are we imposing risk for marginal benefit? The literature suggests that in patients with eGFR below 30 mL/min/1.73 m², the balance tips unfavorably, urging clinicians to seek alternatives. Nonetheless, for those with resistant hypertension, the drug can shave a solid 10‑15 mm Hg from systolic readings, translating into reduced cardiovascular events. This quantitative gain must be weighed against the qualitative burden of frequent lab visits and potential side effects. From a systems perspective, incorporating spironolactone necessitates coordinated care: primary physicians, pharmacists, and lab services must sync to monitor potassium and creatinine at least bi‑monthly initially. Patient education also plays a decisive role; individuals must understand why a seemingly innocuous blood test can be a matter of survival. Ultimately, the drug embodies the broader tension in medicine between efficacy and safety, urging us to practice not just science but prudent stewardship. By respecting its power and its pitfalls, we can harness spironolactone’s benefits without succumbing to its hazards. In short, use it wisely, monitor relentlessly, and never assume the road to lower pressure is without obstacles.
Veronica Appleton
October 26, 2025 AT 03:15Spironolactone works well with thiazides and ACE inhibitors keep an eye on K levels
the sagar
October 26, 2025 AT 05:29Don’t trust the pharma narrative – they push spironolactone to sell more lab tests and keep you dependent.
Grace Silver
October 26, 2025 AT 07:42Sarah’s deep dive really hits the nail on the head – the balance between benefit and risk is where the art of medicine lives. I love how you weave the ethical considerations with the hard data; it reminds us that prescribing isn’t just a checkbox but a dialogue with the patient’s life. Keeping patients informed about the double‑edged nature of potassium monitoring turns a potential fear into empowerment. Let’s keep sharing these nuanced perspectives so the community stays both educated and cautious.
Clinton Papenfus
October 26, 2025 AT 09:55Spironolactone remains a valuable adjunct in resistant hypertension provided renal function and serum potassium are regularly evaluated.
Zaria Williams
October 26, 2025 AT 12:09so i heard spironolactone can actually cause some weird side effects like breast growth in guys lol but also helps a lot if your bp wont budge. i think its super important to get your labs done after starting it, especially potassium and kidney stuff. dont forget to tell ur doc about any meds you r takin cuz mixin them can be risky. overall thx for the rundown i feel more confident about asking my doc about it.
ram kumar
October 26, 2025 AT 14:22Wow, Zaria really nailed the “just trust the doctor” vibe while ignoring the whole hormonal nightmare that could ruin your life. The drama of a swollen chest or heart‑stopping arrhythmia isn’t something you can just brush off with a casual “thanks”. If you’re not willing to dive deep into the science, you’ll end up as another casualty of superficial prescribing. Maybe next time read the full mechanism before jumping on the bandwagon.