When you’re scheduled for surgery, the last thing you want is for a drug you took years ago to come back and haunt you in the operating room. But it happens - and it’s often preventable. About 1.1% of anesthesia-related deaths are tied to undiagnosed or poorly communicated drug reactions, according to the Journal of Anesthesia, Critical Care & Pain Medicine. That’s not just a statistic. It’s someone’s mother, brother, or friend who didn’t get the chance to tell their doctor about that rash they got after penicillin in 2012 - or the nausea that hit them after codeine at the dentist.
The truth? Most people don’t know how to talk about drug reactions properly. They say, "I’m allergic to painkillers," but that’s not enough. Was it codeine? Ibuprofen? Did they break out in hives? Throw up? Go into shock? The difference between a side effect and a true allergic reaction can mean the difference between a smooth surgery and a life-threatening emergency.
What Counts as a Drug Reaction?
Not every bad reaction is an allergy. A lot of patients mix up side effects with true allergies. If you got dizzy after taking aspirin, that’s likely a side effect. If your throat swelled shut after penicillin, that’s an allergic reaction - and it’s dangerous. True allergic reactions involve your immune system and can include:
- Hives or widespread rash
- Swelling of the lips, tongue, or throat
- Difficulty breathing or wheezing
- Drop in blood pressure, dizziness, or fainting
- Anaphylaxis - a full-body emergency reaction
Side effects are unpleasant but not immune-driven. Nausea from morphine, drowsiness from benzodiazepines, or stomach upset from NSAIDs aren’t allergies. But they still matter. Anesthesiologists need to know all of it. Why? Because if you’ve thrown up every time you’ve had codeine, they won’t give you any - even if it’s not an allergy. They’ll pick a safer option.
What to Write Down Before Your Appointment
Don’t rely on memory. Start writing now. Get a notebook or open a note on your phone. List every medication you’ve ever taken - not just the ones you’re on now. Include:
- Prescription drugs (even ones you stopped years ago)
- Over-the-counter painkillers like ibuprofen, naproxen, or acetaminophen
- Vitamins, supplements, and herbal products (ginkgo, garlic, St. John’s wort)
- Any drugs you took for dental work, minor procedures, or even a past C-section
- Drugs you were told you were "allergic" to - even if you’re not sure
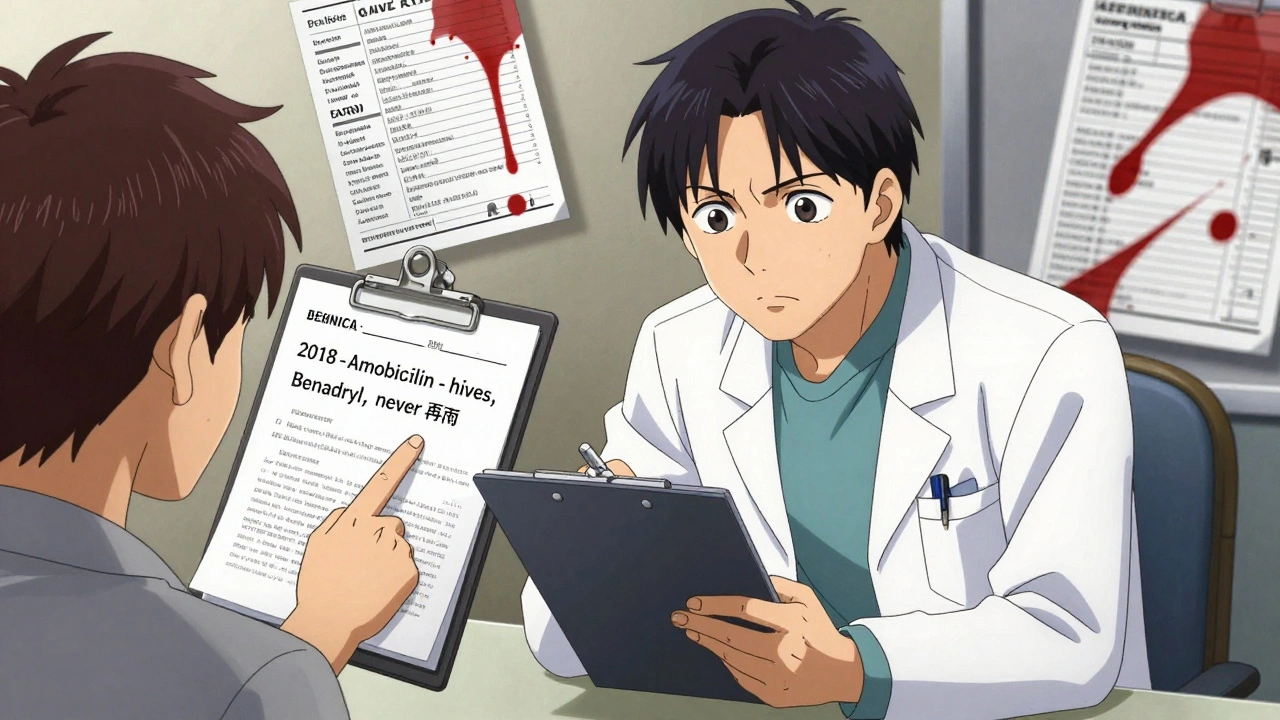
For each one, write down:
- What happened (symptoms)
- When it happened (year, approximate time after taking the drug)
- How it was treated (did you need epinephrine? Hospital visit?)
- Whether you ever took it again after that
Example: "2018 - Took amoxicillin for a tooth infection. Broke out in red, itchy rash all over chest and arms within 4 hours. Took Benadryl. Rash went away in 2 days. Never took it again."
This isn’t just for show. Hospitals like Froedtert and Stanford require this level of detail. If you just say "I’m allergic to antibiotics," they’ll assume the worst and avoid all of them - even ones that are safe for you. That means you might get a less effective, more expensive, or more risky drug.
Who You Need to Tell - and When
You’re not just talking to one person. This information needs to get to multiple teams:
- Your primary doctor or surgeon - Tell them as soon as you schedule surgery. Don’t wait for the pre-op visit.
- The pre-op nurse or pharmacist - They’ll review your list and ask follow-up questions. Bring your written list.
- The anesthesiologist - This is the most critical conversation. They’ll decide what drugs are safe to use during your surgery. They need to know about reactions to muscle relaxants (like succinylcholine or rocuronium), pain meds, antibiotics, and even latex.
Timing matters. Ideally, this should happen at least 72 hours before surgery. Why? Because if there’s a high-risk reaction, they might need to refer you to an allergist for testing. That takes time. The Spanish Journal of Anesthesia and Critical Care recommends allergist evaluation within 4-6 weeks after a reaction - but if you’re already scheduled for surgery, they’ll need to work around it.
And here’s the hard part: if you’ve had a severe reaction in the past and haven’t been evaluated by an allergist yet, your surgical team might delay non-emergency surgery. It’s not punishment - it’s protection. A 2023 study from the American Society of Anesthesiologists found that 37% of emergency surgeries had incomplete allergy records. That’s why elective cases get more time.
What Not to Say - and What to Say Instead
People say things like:
- "I’m allergic to everything."
- "I don’t know, I just felt weird."
- "I think it was the anesthesia."
These don’t help. Here’s how to fix them:
- Instead of: "I’m allergic to everything." Say: "I had a bad reaction to one drug - here’s what it was and what happened."
- Instead of: "I felt weird." Say: "I broke out in hives and couldn’t breathe 10 minutes after they gave me the shot."
- Instead of: "I think it was the anesthesia." Say: "They gave me propofol and rocuronium. The reaction started right after rocuronium."
Be specific. Even if you don’t know the drug name, describe it. "It was a green liquid they injected into my IV." That’s enough for an anesthesiologist to identify.
What Happens If You Don’t Tell Them?
There are real cases where this went wrong. In 2021, the Anesthesia Patient Safety Foundation reported a case where a patient with a known vancomycin allergy got the drug during surgery because no one checked the chart properly. The patient went into anaphylactic shock. They survived - but barely. The hospital had to shut down the OR for 45 minutes.
Another case from Mayo Clinic showed the opposite: a patient with a documented succinylcholine allergy had a smooth surgery because the anesthesiologist had the record and switched to a safer muscle relaxant. That’s the power of good communication.
Bad communication doesn’t just hurt patients - it hurts the system. A 2022 NIH study found that 4.5% of all surgical complications are linked to medication errors. Half of those could have been avoided with better pre-op screening.
Tools That Can Help
You don’t have to remember everything. Use these tools:
- Allergy cards: Many allergists give you a wallet-sized card listing your reactions. Keep it in your wallet or phone case.
- Electronic health records: If your doctor uses Epic or Cerner, ask them to add your reaction to your profile. You can usually access it through a patient portal.
- Medication lists: Apps like MyTherapy or Medisafe let you log drugs and reactions. Print a copy to bring to your appointment.
- Pharmacist check-ins: Some hospitals have pharmacists call you before surgery to review your meds. Take that call. Answer honestly.
One nurse anesthetist from AllNurses.com says: "We spend more time figuring out what patients mean by ‘allergic’ than we do doing the actual surgery." Don’t make them guess. Be clear.
What About Recreational Drugs or Alcohol?
Yes - you need to tell them. If you smoke marijuana, take opioids recreationally, or drink heavily, your anesthesiologist needs to know. These affect how your body handles anesthesia. A 2022 commentary in Anesthesia & Analgesia found that 63% of anesthesiologists delay surgery for patients with recent drug use - even if the drug isn’t directly linked to the reaction. Why? Because it changes your tolerance, breathing patterns, and heart response.
Don’t be ashamed. They’ve heard it all. Framing it as "I want to be safe" - not "I’m a bad person" - gets better results. Stanford’s guidelines say: "Framing the conversation around medical safety often encourages honesty."
After the Surgery - Don’t Stop
Even if your surgery went fine, if you had a reaction before, you need to follow up. Get referred to an allergist. They can do skin tests or blood tests to confirm what you’re truly allergic to. You might be told you’re not allergic to something you thought you were. That opens up safer options for future surgeries.
And make sure your reaction is documented in your medical records - not just in your head. Ask your doctor to add it to your file. If you go to a new hospital, bring your allergy card or printed list. Don’t assume they’ll have it.
By 2028, 95% of U.S. hospitals will have interoperable allergy systems - meaning your info will follow you. But that’s not today. Right now, you’re the only one who can make sure your history isn’t lost.
Final Checklist Before Surgery
Use this before your pre-op appointment:
- Write down every drug you’ve ever taken - including vitamins and herbs.
- For each, note the reaction: symptoms, timing, treatment.
- Separate true allergies (immune response) from side effects.
- Bring a printed list or photo of your notes to every appointment.
- Ask your surgeon or anesthesiologist: "Will you check my history before giving me anything?"
- Request an allergist referral if you’ve had a severe reaction.
- Keep an allergy card in your wallet or phone.
Surgery is stressful enough. Don’t let a simple miscommunication turn it into a crisis. You know your body better than anyone. Speak up. Write it down. Be specific. Your life might depend on it.


Annie Grajewski
December 6, 2025 AT 00:23so i took penicillin in 2007 and got a rash so i thought i was allergic but turns out it was just the soap i was using?? my mom freaked out and made me wear a medical alert bracelet for 12 years lmao. now i take it like candy. doctors are wild.
Mark Ziegenbein
December 7, 2025 AT 22:35Let me be perfectly clear-this is not merely a matter of clinical protocol, it is a metaphysical failure of the modern medical-industrial complex to recognize the sovereignty of the individual body. You are not a data point. You are not a chart. You are a sentient being whose lived experience of pharmacological trauma has been reduced to a checkbox in Epic. The anesthesiologist does not deserve your trust until they have wept over your handwritten notes. Until then, you are not safe. You are merely tolerated.
Norene Fulwiler
December 9, 2025 AT 03:52I’m a nurse in Chicago and I’ve seen this go wrong too many times. One woman came in for a C-section and just said ‘I’m allergic to meds.’ We had to pause everything while we dug through her old records. Turns out she had a mild reaction to aspirin at 16. We could’ve used it safely. But because she didn’t know how to explain it, they gave her something riskier. Please, just write it down. Even if it feels dumb. It’s not dumb. It’s saving your life.
William Chin
December 9, 2025 AT 12:53It is imperative that all patients adhere to the standardized protocol for preoperative pharmacological disclosure, as outlined in the Joint Commission’s 2023 Guidelines on Medication Safety. Failure to provide a comprehensive, chronologically indexed, and medically validated drug reaction history constitutes a breach of patient responsibility and may result in liability for adverse outcomes. I strongly recommend utilizing the FDA’s MedWatch Form 3500 for documentation prior to surgical consultation.
James Moore
December 10, 2025 AT 06:35And yet, the Left keeps telling us that ‘trust the science’-but when the science says ‘write down what happened,’ they call you a conspiracy theorist? Meanwhile, the same people who scream ‘personal freedom’ won’t lift a finger to document that they got sick after a flu shot in 2015. It’s not about vaccines. It’s about accountability. America is crumbling because people won’t take responsibility for their own damn bodies. Write. It. Down.
Kylee Gregory
December 11, 2025 AT 06:04I think the real issue here isn’t just about remembering drug names-it’s about how we’ve been trained to distrust our own bodies. We’re taught to dismiss our symptoms as ‘just anxiety’ or ‘not that bad.’ But if your body says ‘no’ to something, even if it’s not a textbook allergy, it’s worth listening to. Maybe the answer isn’t just better forms, but better listening. From everyone.
Laura Saye
December 12, 2025 AT 11:25There’s a profound epistemological gap between clinical taxonomy and phenomenological experience. Patients often lack the lexicon to articulate somatic phenomena that fall outside diagnostic criteria-yet their embodied memory remains accurate. The burden of translation is disproportionately placed on the vulnerable. Perhaps the solution isn’t more documentation, but more compassionate interrogation by clinicians who recognize that ‘I felt weird’ is a legitimate data point.
luke newton
December 13, 2025 AT 18:44People who don’t tell doctors about their weed use deserve everything that happens to them. You think the anesthesiologist wants to guess whether you’re a chronic smoker or a weekend warrior? No. You’re risking your life-and theirs-by being shady. If you’re gonna get high, own it. Don’t be a coward. Your silence isn’t privacy-it’s negligence.
Ali Bradshaw
December 14, 2025 AT 05:14I’m a paramedic in Scotland and we see this all the time. One guy came in after a fall and said ‘I think I’m allergic to something.’ We found out he’d had a bad reaction to ibuprofen in 2019 but never told anyone. He was fine after we switched meds. Just one sheet of paper saved him hours of panic. You don’t need to be perfect-just honest. Write it down. Bring it. You’ve got this.
Lynette Myles
December 15, 2025 AT 01:41They’re using your drug history to track you. The chip in your medical record is linked to the CDC’s bio-surveillance network. Don’t write anything down. Say nothing. They already know.