Getting the timing right on your medications isn’t just about remembering to take them-it’s about keeping you safe. If you’re taking five or more drugs a day, you’re at serious risk. A 2019 study in the Journal of the American Geriatrics Society found that 82% of people on multiple medications experience at least one harmful interaction. That’s not a small number. It’s a daily threat. But here’s the good news: a simple, well-structured schedule can cut those risks by more than half. You don’t need a PhD to do this. You just need a clear plan.
Start with a Complete Medication List
Before you even think about timing, you need to know exactly what you’re taking. Not just the prescriptions. Not just the vitamins. Everything. That includes over-the-counter painkillers, herbal teas, supplements, and even antacids. Most people forget at least three things when they try to list their meds. I’ve seen it a hundred times: someone says they take “just three pills,” but when they bring their medicine cabinet to the pharmacist, there are 11 bottles. That’s why the Universal Medication Schedule (UMS) starts with a full inventory. Write down every item, including:
- Brand and generic name
- Dosage (e.g., 10 mg, 500 mg)
- How often you take it (e.g., once daily, twice a week)
- Why you take it (e.g., “for blood pressure,” “for joint pain”)
- Any special instructions (e.g., “take on empty stomach,” “avoid grapefruit”)
Do this in writing. Don’t rely on memory. Keep a printed copy in your wallet and another taped to your bathroom mirror. Update it every time your doctor changes something-even if it’s just adding one new pill. A 2021 study in Patient Education and Counseling showed that patients who kept a written list had 45% fewer dosing errors than those who didn’t.
Use the Universal Medication Schedule (UMS) Timeframes
“Take twice daily” is a recipe for disaster. A 2016 study found that 34% of patients with low health literacy misunderstood what that meant. Did they mean 8 a.m. and 8 p.m.? Or 7 a.m. and 7 p.m.? Or maybe 8 a.m. and 8 p.m. but they took one at midnight? Confusion like that leads to missed doses, double doses, or dangerous timing conflicts.
The UMS fixes this by replacing vague phrases with clear, standardized time windows:
- Morning: 6 a.m. to 10 a.m.
- Noon: 10 a.m. to 2 p.m.
- Evening: 2 p.m. to 6 p.m.
- Bedtime: 8 p.m. to 12 a.m.
This system works because it gives you a window, not a clock. If your doctor says “take in the morning,” you have four hours to do it. You don’t have to wake up at 6:30 a.m. just because someone said “take it at 7.” This simple shift reduced misinterpretation rates from 34% to just 6% in a JAMA Internal Medicine trial. And adherence jumped by over 12 percentage points.
Group Medications by Time Window
Now that you know your time windows, start grouping. Don’t just line up pills in order of size or color. Think about how your body absorbs them.
For example:
- Thyroid medication (like levothyroxine) must be taken on an empty stomach, at least 30-60 minutes before food. That means it belongs in the morning window-right after you wake up, before coffee or breakfast.
- Statins (cholesterol drugs) work best when taken at night because your liver makes the most cholesterol while you sleep. So even if you take them with food, they belong in the bedtime window.
- Certain antibiotics (like amoxicillin) need to be taken every 8 hours. If you take one at 8 a.m., the next should be at 4 p.m., and the last at midnight. That’s tricky with UMS windows. For these, you may need to break the rules slightly and use alarms.
- Calcium supplements interfere with thyroid meds. If you take both, space them at least 2 hours apart. So if you take thyroid at 7 a.m., take calcium at noon or later.
Use color-coded stickers or labels on your pill bottles to match your time windows. Red for morning, blue for noon, green for evening, purple for bedtime. It sounds simple, but a 2020 case study from Harmony Healthcare showed that a patient taking 12 medications went from having monthly side effects to none after using this system.

Use a Pill Organizer-But Choose the Right One
A pill organizer isn’t just a box with compartments. It’s your safety net. A 2018 meta-analysis in the Annals of Internal Medicine found that using a pill organizer with AM/PM or 7-day compartments reduced dosing errors by 45%.
Here’s what to look for:
- 4-compartment daily: Best for people taking meds at 4 different times (morning, noon, evening, bedtime).
- 7-day with 4 slots per day: Best for complex regimens. Lets you fill a whole week at once.
- Large, easy-to-read labels: If you can’t read the labels, it’s useless. Choose ones with bold text or tactile markers.
- Lockable lid: Prevents accidental spills or kids from getting into them.
Don’t use a basic pill box with just 2 compartments (AM/PM) if you’re taking more than 3 meds. It’s not enough. And never fill your organizer more than a week in advance-some meds lose potency or become unsafe if stored too long.
Watch for Dangerous Interactions
Not all interactions are obvious. The American Geriatrics Society’s Beers Criteria (updated in 2023) lists 30 high-risk combinations that older adults should avoid. Here are the most common and dangerous ones:
- NSAIDs (ibuprofen, naproxen) + blood thinners (warfarin, apixaban): Increases bleeding risk by 60-70%.
- Statin + grapefruit juice: Can cause muscle damage and kidney failure.
- Antibiotics (fluoroquinolones) + antacids or iron supplements: Blocks absorption. Take them 2 hours apart.
- SSRIs (antidepressants) + NSAIDs: Raises risk of internal bleeding.
- Diuretics + potassium supplements: Can spike potassium to dangerous levels.
When in doubt, ask your pharmacist. They use tools like Lexicomp that screen for over 150 common interactions. A single 10-minute review can catch problems your doctor might miss. Pharmacists who run medication therapy management programs reduce drug-related ER visits by 24%, according to the American Journal of Health-System Pharmacy.
Sync Your Refills
If your meds are due on different days, you’re setting yourself up for missed doses. That’s why the American Medical Association recommends “90 x 4” prescribing: get a 90-day supply of each medication, refilled four times a year-on the same day.
For example: instead of refilling your blood pressure pill on the 5th, your cholesterol pill on the 12th, and your diabetes pill on the 20th, you get them all on the 1st of every three months. It saves you time. It cuts down on errors. And according to the AMA’s STEPS Forward toolkit, it saves clinicians two hours per day in administrative work. That’s not just convenient-it’s lifesaving.
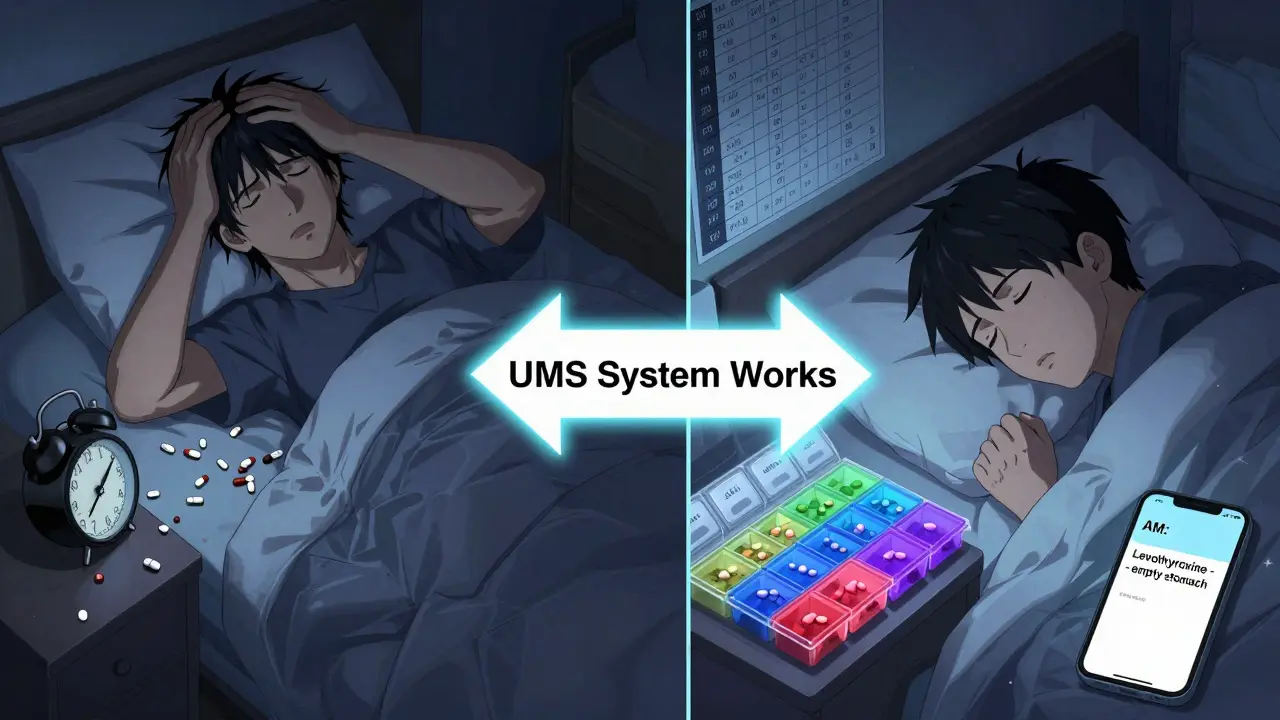
Use Visual Aids and Reminders
Memory fails. Especially when you’re tired, stressed, or overwhelmed. That’s why the most successful users rely on visuals.
- Hang a large chart near your medication area. Include each drug, time window, purpose, and special note (e.g., “take with food,” “avoid alcohol”).
- Set smartphone alarms labeled clearly: “AM: Levothyroxine (empty stomach),” “PM: Statin (with dinner).”
- Apps like Medisafe and MyTherapy send reminders and track adherence. A 2021 JMIR study found they improve adherence by 20-35% over paper systems.
- But if you’re over 65, don’t assume apps will work. Only 38% of seniors use them consistently. For many, a printed calendar with checkmarks is still the best tool.
One patient on Reddit said: “I take 7 meds with specific food rules. Coloring each pill by condition and using morning/noon/evening/bedtime made my dizziness disappear.” That’s the power of clarity.
Get Help When You Need It
You don’t have to do this alone. Pharmacists are trained to spot interactions. Ask for a “brown bag review”-bring all your meds (including supplements) to your pharmacist. They’ll compare what you’re taking with what’s in your chart. On average, they find 3.2 medication discrepancies per person. That’s more than three mistakes per visit.
If you’re seeing multiple specialists, ask your primary care doctor to coordinate your meds. Fragmented care is the biggest problem. A 2022 JAMA Internal Medicine study found that patients see an average of 13.1 specialists over five years. Each one might prescribe something that clashes with what another one gave you.
And if you’re ever unsure-pause. Don’t guess. Call your pharmacist. They’re the experts on how drugs behave in your body. Not your doctor. Not Google. Not a friend.
What to Do If You Miss a Dose
Everyone misses a dose. It happens. But how you respond matters.
- If you miss a dose by less than 2 hours: take it as soon as you remember.
- If it’s more than 2 hours late: skip it. Don’t double up. That’s when overdoses happen.
- If you’re unsure: call your pharmacist. Don’t guess.
Never assume “I’ll just take it later.” That’s how people end up in the ER.
Can I take all my pills at once to make it easier?
No. Many medications need to be taken separately to work properly or avoid harm. For example, taking calcium with thyroid medication blocks absorption. Taking NSAIDs with blood thinners increases bleeding risk. Even if it seems easier, combining pills without knowing the interactions can be dangerous. Always check with your pharmacist before changing your routine.
What if my doctor changes my dose but doesn’t tell me about interactions?
That’s more common than you think. A 2022 NEHI report found that 67% of patients received conflicting timing instructions from different specialists. Always ask: “Does this change affect how I take my other meds?” Then, bring your updated list to your pharmacist for a quick review. It takes five minutes and could prevent a hospital visit.
Are generic drugs safer or riskier than brand names for interactions?
Generic drugs have the same active ingredients as brand names, so they carry the same interaction risks. The difference is in inactive ingredients-like fillers or dyes-which rarely cause issues. But if you notice new side effects after switching to a generic, talk to your pharmacist. It’s not always the drug-it could be the filler.
Do I need to track supplements like vitamins and herbs?
Absolutely. Over 70% of adults take at least one supplement. Many interact with medications. For example, St. John’s Wort reduces the effectiveness of birth control, blood thinners, and antidepressants. Garlic and ginkgo can thin your blood. Vitamin K can interfere with warfarin. Treat supplements like real drugs-list them, time them, and ask your pharmacist about each one.
How long does it take to set up a good medication schedule?
Most people get their system working in 2-4 weeks. The first week is about gathering all your meds and writing them down. The second week is sorting them into time windows. The third week is filling your pill organizer and setting alarms. By week four, it becomes routine. The key is consistency-not perfection. Even if you mess up once, get back on track the next day.
Creating a medication schedule that minimizes interactions isn’t about being perfect. It’s about being smart. It’s about using clear time windows, writing everything down, using a pill organizer, and asking for help when you need it. The system works. It’s been tested. It’s saved lives. And it can save yours too.

THANGAVEL PARASAKTHI
February 8, 2026 AT 09:26man i just started using this u-m-s thing last month and holy crap it changed everything. used to mix up my blood pressure and diabetes pills all the time. now i just look at the color stickers-red for morning, purple for bed-and boom, no more confusion. also started writing everything on a sticky note taped to my fridge. my wife says i’m obsessed but hey, i’m alive.
Frank Baumann
February 9, 2026 AT 00:12let me tell you something-this whole system is a godsend but nobody talks about the REAL issue: pharmacies. i had a pharmacist accidentally give me my neighbor’s blood thinner because the bottles looked similar. i didn’t catch it until i started bleeding from my gums. now i label every single bottle with my name, date of birth, and a QR code that links to my med list. if you’re not doing this, you’re playing russian roulette with your kidneys. and yes, i’m still mad about it.
Scott Conner
February 9, 2026 AT 20:09so i tried the 4-compartment organizer but kept forgetting what each color meant. ended up using a cheap whiteboard and dry erase markers-morning, noon, evening, bed. i update it every time my doc changes something. also started using a voice memo on my phone: 'levothyroxine, empty stomach, wait 30 min before coffee.' it’s weird but it works. my cat even seems to know when it’s pill time now.
Susan Kwan
February 10, 2026 AT 07:42oh wow, another 'life-changing' med hack. next you’ll tell us to chant affirmations while swallowing pills. also, who wrote this? a pharmaceutical rep with a thesaurus? 'universal medication schedule' sounds like something a startup named after a failed yoga retreat.
Random Guy
February 11, 2026 AT 21:31my mom took 17 pills a day. 17. she called them her 'rainbow army.' one day she mixed up her blood thinner with her calcium and ended up in the ER screaming about 'the green pills attacking her.' we got her a pill organizer with alarms that scream 'YOU’RE NOT DEAD YET, TAKE YOUR PILLS!' it’s loud. it’s obnoxious. it saved her life. i’m not sorry.
Tasha Lake
February 11, 2026 AT 23:11the statin + grapefruit interaction is critical-seriously, if you’re on a statin, avoid grapefruit, pomelo, Seville oranges, and even some juices labeled 'natural.' the furanocoumarins in them inhibit CYP3A4, which leads to elevated plasma concentrations and increased rhabdomyolysis risk. also, if you're on a CYP2D6 substrate like metoprolol, don't take it with SSRIs unless you're ready for QT prolongation. pharmacogenomics isn’t optional anymore.
Brett Pouser
February 13, 2026 AT 07:38i’m 72 and i never thought i’d be this organized. but after my wife passed, i almost lost myself in the pills. this system? it gave me structure. i color-code, i use a big calendar, i set alarms, and i call my pharmacist every time something changes. they don’t charge me. they just care. i’m not just surviving anymore. i’m living. thank you for writing this. seriously.
Karianne Jackson
February 14, 2026 AT 08:36my grandma uses a shoebox full of pill bottles and calls it her 'medication zoo.' she says if it fits, it sits. i tried to get her a fancy organizer. she told me i was trying to turn her into a robot. now i just check in every day and say, 'which pill did you forget today?' she laughs. we laugh. we live.
Andy Cortez
February 16, 2026 AT 06:26oh sure, follow this 'science'... but what about the 2015 study where 60% of people using pill organizers still overdosed because they couldn’t read the tiny labels? and don’t get me started on 'color-coding'-what if you’re colorblind? or blind? or just lazy? this whole thing is a luxury for people who have time, money, and a daughter who does their laundry. most of us are just trying not to die before lunch.
Jacob den Hollander
February 16, 2026 AT 09:48you know what? this post? it’s not perfect. but it’s real. i’ve been helping my dad manage his meds since he got diagnosed with heart failure. we did the brown bag review. the pharmacist found 4 meds he wasn’t even supposed to be on. one of them was a 10-year-old prescription from a doctor who retired. we cried. then we laughed. now he uses a 7-day organizer with big letters, alarms, and a list taped to his coffee maker. he says he feels like a boss. and honestly? so do i. you don’t need a PhD. you just need someone who cares enough to help you write it down.