Why Reading Prescription Labels for Inhalers, Patches, and Injectables Matters
It’s not just about knowing what medicine you’re taking. With inhalers, patches, and injectables, a small mistake on the label can mean the difference between relief and an emergency. You might think, "I’ve read labels before-I know how this works." But these aren’t pills you swallow. Each one has unique rules. Get it wrong, and you could underdose, overdose, or damage your health without even realizing it.
In 2023, over 1,400 serious adverse events in the U.S. were linked to people misreading labels on these delivery systems. That’s not rare. It’s common. And the biggest problem? People don’t know what to look for. The label says "25 mcg/hour" on a patch. But what does that mean? Does it mean you wear it for 24 hours? 48? What if you forget and leave it on too long? What if you cut it? What if you think the inhaler is empty because it doesn’t rattle? You’re not alone. Three in five patch users don’t realize "change every 72 hours" means exactly 72 hours-not "about three days." And nearly half of insulin users misread "100 units/mL" as "100 total units." That’s a dangerous mix-up.
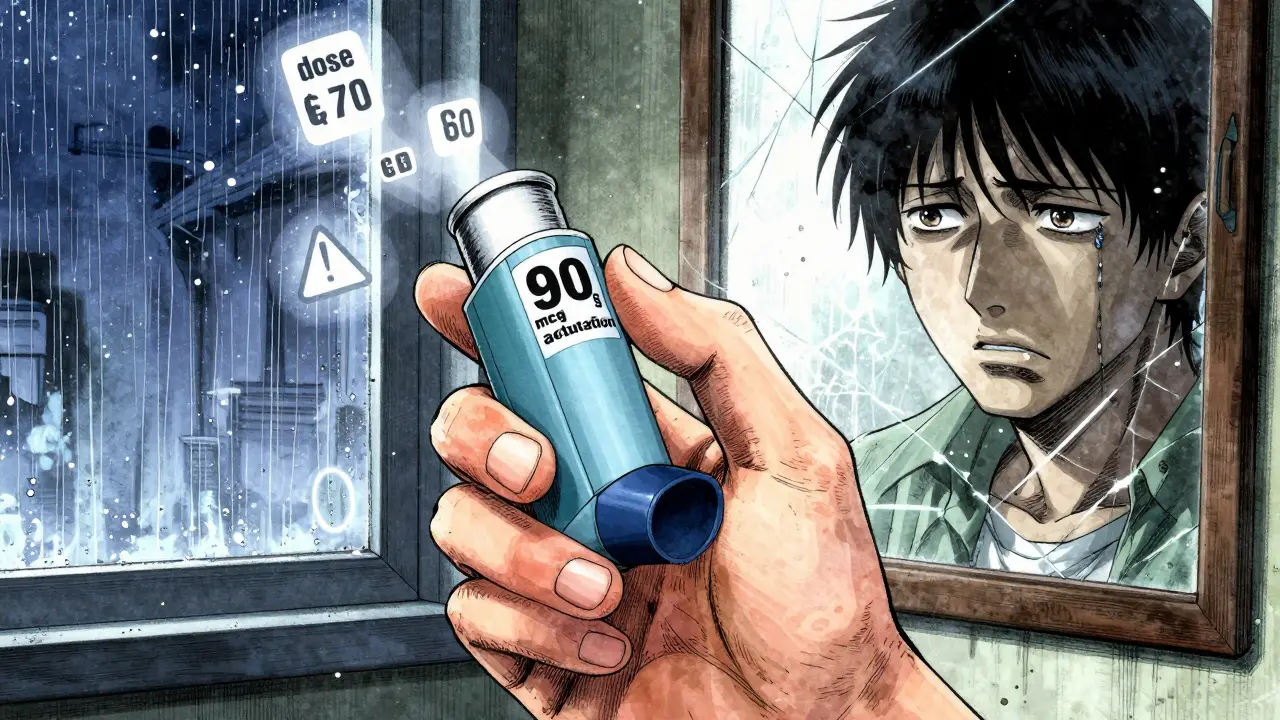
Inhaler Labels: More Than Just a Canister
Inhalers look simple. A metal canister, a mouthpiece, maybe a cap. But the label holds critical details most people miss. First, check the dosage per actuation. It’s usually written like "albuterol sulfate 90 mcg per actuation." That’s the amount released with one press. Never assume it’s the same across brands. Even if two inhalers look alike, their doses can be totally different.
Next, find the total number of actuations. This tells you how many doses are left. Some older inhalers don’t have counters. New ones must have them by 2024, per FDA rules. But even with a counter, don’t trust how it feels. The canister might still rattle even when it’s empty. That’s because the propellant is still inside. The medication? Gone. Always count your puffs. If the label says "200 doses" and you’ve used 190, it’s almost out-don’t wait for it to feel empty.
Look for "prime" instructions. New inhalers need to be sprayed into the air four times before first use. So do ones you haven’t used in over two weeks. Skip this, and you might get nothing. Also, check if it says "shake well." That only applies to suspension inhalers-those with cloudy liquid. Clear solutions don’t need shaking. Mixing them up can mess up your dose.
And here’s a big one: pictograms. Since 2020, 78% of inhaler labels now include step-by-step pictures showing how to use it. These cut technique errors by over 20%. If yours doesn’t have them, ask your pharmacist for a printed guide. Or scan the QR code on the box-it might link to a video. That’s now on 67% of new inhalers.
Transdermal Patches: Heat, Skin, and Disposal Risks
Patches seem easy. Stick it on, wait, feel better. But they’re among the most dangerous if misused. The label must show the delivery rate, like "fentanyl 25 mcg/hour." That’s how much drug your body gets every hour. If you wear it longer than directed-say, 72 hours instead of 48-you’re doubling your dose. That’s how overdoses happen.
Watch for heat warnings. Since 2021, Health Canada and the FDA require patches to say "avoid heat sources." That means no hot tubs, saunas, heating pads, or even sitting near a radiator. Heat can boost absorption by up to 50%. One study found people using fentanyl patches near a heating pad ended up in the ER with respiratory depression. It’s not rare. It’s predictable.
Application site matters too. Labels tell you where to put it-upper arm, chest, back. Never apply it to irritated skin or areas with cuts. Rotate sites each time. Putting it in the same spot can cause skin damage or uneven absorption. And never, ever cut a patch. Fentanyl patches are designed to release slowly. Cut one, and you get a sudden rush of drug. The FDA says cutting increases overdose risk by nearly five times.
Disposal is another hidden risk. Used patches still have half their drug left. The label must say how to dispose of them safely. Some say "fold sticky sides together" and flush. Others say "return to pharmacy." In 2022, 147 cases of accidental exposure-mostly in kids-came from patches thrown in the trash. Don’t risk it. Follow the label. If it doesn’t say, call your pharmacist.

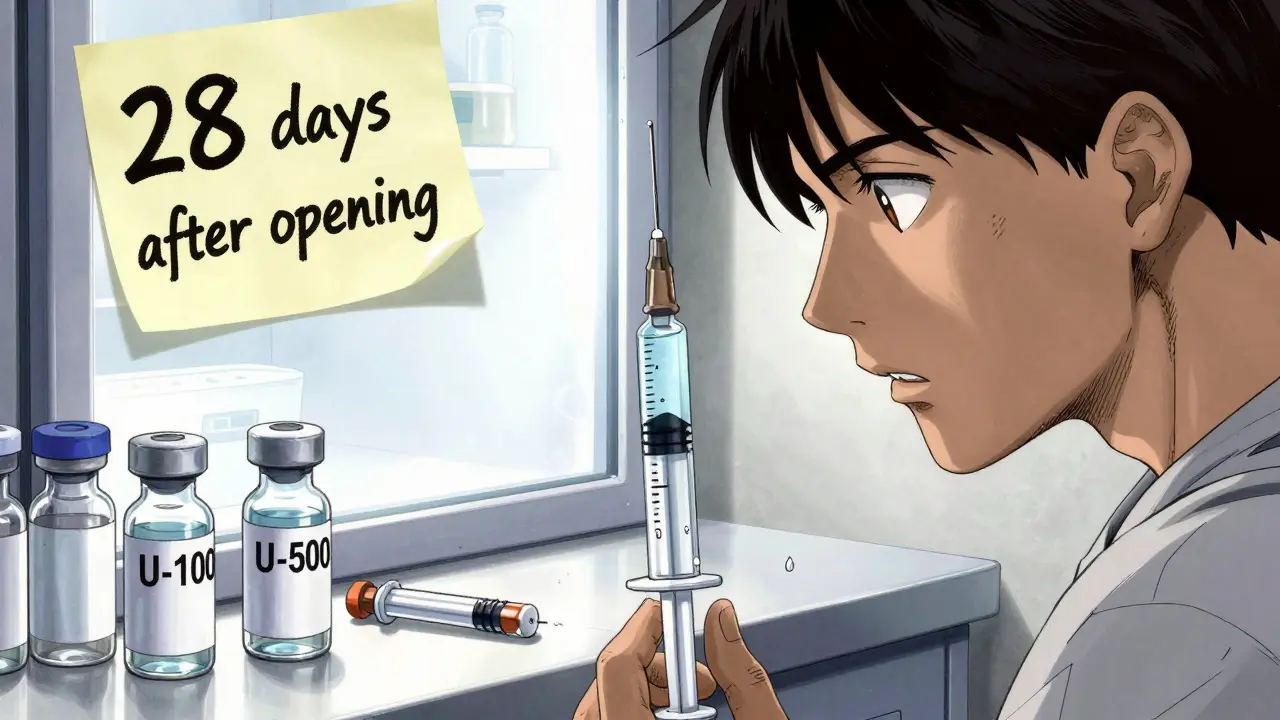
Injectables: Concentration Is Everything
Injectables are the trickiest. One misread number can kill. The most common error? Misreading concentration. Insulin labels say "U-100." That means 100 units per milliliter. But some insulins are U-200, U-500, or even U-1,000. If you think you’re giving 10 units of U-100 but grab U-500 by mistake? You just gave 50 units. That’s five times too much. It can send you into a coma.
Look for the concentration right after the drug name. It’s always there. For example: "insulin glargine 100 units/mL" or "octreotide 200 mcg/mL." If it’s not written clearly, ask. Don’t guess. Many injectables also need reconstitution-mixing powder with liquid. The label will say how much liquid to add and how to mix it. Use the right syringe. Use the right water. Skip a step, and the dose is wrong.
Storage matters too. Some injectables need refrigeration. Others must be kept at room temperature. If you leave insulin in the sun or freeze it, it breaks down. It won’t work. The label says "store between 36°F and 46°F"? That’s fridge temp. "Store at room temperature"? Keep it away from heat, light, and moisture. Never use a vial that looks cloudy unless it’s supposed to be.
And don’t ignore auxiliary labels. Those little stickers on the bottle? They say things like "shake before use," "do not use if discolored," or "use within 28 days after opening." These aren’t optional. They’re safety rules. A 2023 study found 92% of injectable prescriptions have these. If you don’t see one, ask why.
Why You Can’t Rely on Memory or Assumptions
You’ve used the same inhaler for years. You know how it works. But labels change. New versions come out. Your doctor might switch your brand. Even small changes-like switching from albuterol 90 mcg to 108 mcg-can affect how you feel. And if you’re on multiple devices? You’re at higher risk. A 2023 study found 43% of patients using more than one type of delivery system mixed them up. One person applied a patch meant for inhalation. Another used an insulin syringe for a different injectable. That’s not a fluke. It’s the result of similar-looking packaging and inconsistent labeling.
Pharmacists aren’t always able to explain everything. A 2023 JAMA study found only 38% of patients get a full 15-20 minute counseling session on how to use their device. That means you’re left to figure it out yourself. Don’t assume. Don’t guess. Always read the label. Even if you’ve used it before. Every time.
What to Do When the Label Is Confusing
If you’re unsure, don’t wing it. Call your pharmacist. Bring the actual device and label. Ask: "What does this number mean?" "How do I know when it’s empty?" "What happens if I leave it on too long?" Don’t feel silly. These questions save lives.
Use technology. Many new labels have QR codes. Scan them. Watch the video. It’s faster than reading. If your device doesn’t have one, ask if your pharmacy can give you a printed guide or link. Some pharmacies now offer free video consultations just for these devices.
Write it down. Keep a small card in your wallet or phone notes with: drug name, dose, how often, how to use, and what to watch for. For example:
- Inhaler: Albuterol 90 mcg, 2 puffs every 4-6 hours as needed. Shake before use. Prime before first use. Count puffs.
- Pad: Fentanyl 25 mcg/hr. Change every 72 hours. No heat. Fold sticky sides together before trash.
- Injection: Insulin glargine U-100. 10 units nightly. Store in fridge. Use within 28 days after opening.
Update this card every time your prescription changes. Even a small change matters.
The Future Is Clearer-But You Still Need to Read
Things are improving. By 2025, all new inhalers and patches will have standardized pictograms. By 2026, pharmacies will start using AI tools to double-check labels before you leave. By 2027, you might be able to point your phone at a patch and see a 3D animation showing how to apply it. That’s great. But it won’t replace your responsibility.
Technology helps. But you’re still the last line of defense. If you don’t read the label, no app or AI can stop you from making a mistake. The WHO says standardized labeling could prevent 2.1 million errors a year. But only if patients actually use the information.
So next time you pick up an inhaler, patch, or injectable-stop. Read the label. Even if you think you know it. Because the next time you use it, it might be different. And your health depends on getting it right.

Solomon Ahonsi
February 2, 2026 AT 08:46George Firican
February 4, 2026 AT 04:37Matt W
February 4, 2026 AT 16:20Anthony Massirman
February 5, 2026 AT 18:29Bob Hynes
February 6, 2026 AT 23:46Eli Kiseop
February 7, 2026 AT 16:22Ellie Norris
February 8, 2026 AT 02:24Sandeep Kumar
February 9, 2026 AT 21:31Bridget Molokomme
February 10, 2026 AT 14:23