When you take a medication, you expect it to help - not hurt. But mistakes happen. A pharmacist gives you the wrong dose. A nurse administers the wrong drug. Your doctor prescribes something that clashes with another medicine you’re on. These aren’t rare accidents. In the U.S., medication errors injure about 1.3 million people every year. That’s more than car accidents or falls. The scary part? Most of these errors go unreported. And if no one reports them, nothing changes.
You don’t need to be a doctor or a nurse to make a difference. If you notice something off - a strange side effect, a label that doesn’t match your prescription, a pill that looks different than last time - you have the power to stop the next person from getting hurt. Reporting a medication error isn’t about blaming anyone. It’s about fixing the system.
Recognize the Error - Trust Your Instincts
The first step is simple: notice something’s wrong. Don’t second-guess yourself. Medication errors aren’t always obvious. Sometimes it’s a rash that appeared after starting a new pill. Other times, it’s confusion - you were told to take one tablet twice a day, but the bottle says three. Maybe your child’s school nurse gave them a medicine they don’t normally take. Or you picked up a refill and the pill color changed without explanation.
Here’s what to look for:
- The medicine looks, smells, or tastes different than before
- The dosage instructions changed without warning
- You’re told to take a medicine you’re allergic to
- You develop new symptoms right after starting a new drug
- A school or nursing home staff member gives your child or loved one the wrong medication
Don’t wait for confirmation. If it feels wrong, it probably is. A 2022 study found that 64% of patient-reported errors were dismissed until medical records backed them up. Your word matters - especially if you document everything.
Gather the Facts - Before You Talk
When you report an error, details save lives. A vague complaint like “I think I got the wrong medicine” won’t help. But a clear report with specific data can trigger a recall, fix a hospital procedure, or even change how a drug is labeled.
Collect these before you speak to anyone:
- The medication: Name (brand and generic), dosage (e.g., 500 mg), form (tablet, liquid, injection), and frequency (e.g., once daily)
- The error: What actually happened? (e.g., “I was prescribed 10 mg, but got 50 mg.”)
- The timing: When did you take it? When did symptoms start?
- Your reaction: What happened to you? Nausea? Dizziness? Swelling? Take a photo if there’s a visible reaction
- Other meds: List all other drugs, supplements, or vitamins you’re taking
- Who was involved: Pharmacy name, nurse’s name, doctor’s name, school staff member
- Proof: Keep the pill bottle, prescription label, or receipt. Don’t throw them away
One patient in a 2023 Healthgrades review submitted a photo of the wrong label on her insulin bottle. Within three days, the FDA issued a recall. That photo didn’t just help her - it stopped others from getting the same dangerous dose.
Report It - Start With Your Provider
Your first stop should be the person who caused the error - or the person who can fix it. That’s usually your doctor, pharmacist, or nurse.
Here’s how to do it without sounding confrontational:
- Call or visit their office. Say: “I need to report a medication error that happened to me. I’d like to make sure this doesn’t happen to someone else.”
- Hand them your notes. Don’t just talk - give them the facts in writing.
- Ask: “Can you file a formal internal report?” Most hospitals and clinics have a safety reporting system. They’re required to track these.
- Request a written acknowledgment. Ask for an email or letter confirming they received your report.
According to FDA data, reports submitted through healthcare providers have an 89% acknowledgment rate. Reports submitted directly by patients? Only 28%. That’s not because patients are ignored - it’s because providers have better access to the systems that track and analyze errors.
If they brush you off? Say: “I understand mistakes happen. But if this isn’t documented, it could happen again. I’m asking you to report it - not to punish anyone, but to protect others.”
Go Further - Report to External Systems
Your provider might not act. Or they might act too slowly. That’s why you need to report externally, too. Two major systems exist:
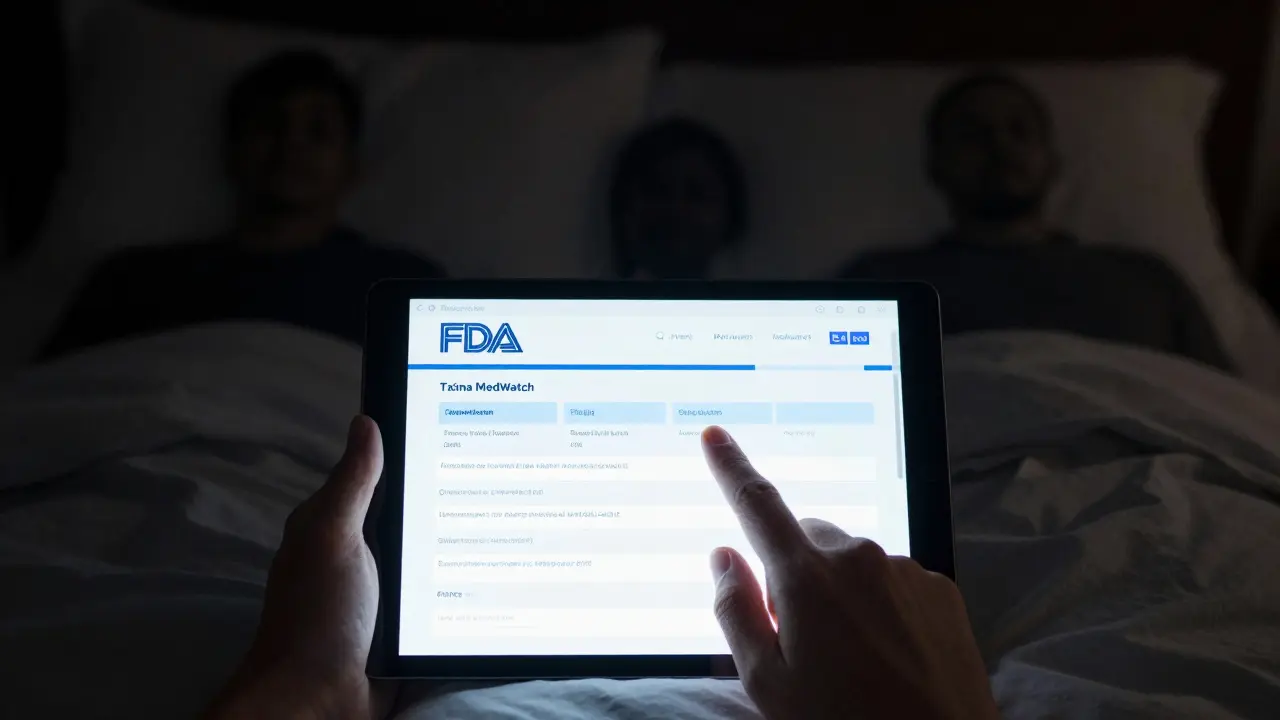
1. FDA MedWatch
The FDA handles over 140,000 medication error reports each year. Most come from doctors and pharmacists. But patients can - and should - report too. Since 2023, the online form has been redesigned to take less than 10 minutes. You don’t need a login. Just go to fda.gov/medwatch.
What the FDA does with your report:
- Tracks patterns (e.g., if 50 people report the same pill causing seizures)
- Issues safety alerts
- Forces recalls
- Changes labeling
You don’t need to be an expert. Just fill out the form honestly. Include your contact info - they might follow up.
2. ISMP National Medication Errors Reporting Program
The Institute for Safe Medication Practices (ISMP) runs a confidential, non-punitive reporting system. They’ve helped fix over 200 medication safety issues since 1991. Their reports go directly to healthcare teams - not to regulators. They’re especially good at catching errors in hospitals and pharmacies.
Visit ismp.org/report-error to file. You can report anonymously. No names. No judgment. Just facts.
What If It Happened at School?
School medication errors are terrifying - and underreported. In 48 states, schools are required to report errors. But only 32% of districts actually improve their procedures after an incident.
If your child was given the wrong medicine:
- Get the school’s incident report in writing
- Ask for a meeting with the school nurse and principal
- Request a copy of their medication administration policy
- File a report with your state’s Department of Education - most have a dedicated form
- Call the school district’s central office if you get no response
Parents who reported school errors in Iowa in 2022 said 87% of them wanted to know how the school would prevent future mistakes. Only 41% got that answer. Don’t let silence win.
Don’t Let Fear Stop You
Many people don’t report because they’re afraid:
- “I’ll get in trouble” - You won’t. Reporting is protected.
- “They’ll think I’m overreacting” - You’re not. Medication errors are the #1 cause of preventable harm in hospitals.
- “It won’t make a difference” - But it will. A 2021 study found that hospitals with non-punitive reporting cultures saw a 300-400% increase in error reports - and a 75% drop in repeat errors.
Dr. Robert Wachter, a top patient safety expert, says: “The most effective systems separate blame from learning.” That’s the goal. Not punishment. Not shame. Just improvement.
And here’s the truth: if you don’t report, someone else will get hurt. Maybe next time, it’ll be your sibling, your parent, your child.
Follow Up - And Keep Records
Reporting isn’t a one-time task. After you submit:
- Wait 7-10 days. Then call to ask if they received it
- Request a copy of any internal report filed
- Save every email, letter, or note you get
- If you don’t hear back, escalate: go to hospital administration, file a complaint with your state medical board, or report to the FDA
Patients who followed up had a 70% higher chance of seeing real change. One man reported his wife’s incorrect chemotherapy dose. He called every week for three months. Eventually, the hospital changed its entire chemo verification process.
What Happens After You Report?
Here’s the reality: not every report leads to a headline. But every report adds to the data. And data changes policy.
When enough people report the same error - like a confusing pill label or a nurse missing a double-check - hospitals are forced to fix it. The FDA doesn’t act on one report. But 50? 100? That’s when they issue a warning. That’s when pharmacies redesign their systems.
And here’s the good news: by 2025, every electronic health record system in the U.S. will be required to include a built-in medication error reporting button. That means reporting will become as easy as clicking “save.” But until then - your voice is the only tool we have.
What if my provider refuses to report the error?
If your provider refuses, report directly to the FDA’s MedWatch program or the Institute for Safe Medication Practices (ISMP). Both accept reports from patients. You don’t need permission. You also have the right to request your full medical records under HIPAA - if they delay, file a complaint with the U.S. Department of Health and Human Services. Your report matters, even if they won’t file it.
Can I report an error even if I didn’t get hurt?
Yes. In fact, you should. The most dangerous errors are the ones that almost happened - called “near misses.” Reporting these helps prevent future harm. The National Coordinating Council for Medication Error Reporting and Prevention (NCC MERP) classifies errors from Category A (no harm possible) to Category I (death). Even Category A errors are worth reporting because they reveal system flaws.
Will reporting get me or my provider in trouble?
No. Reporting is protected. The FDA and ISMP do not share personal details with regulatory agencies unless you ask. Hospitals with “just culture” policies focus on fixing systems, not punishing individuals. In fact, providers who report errors are often praised. Fear of blame is the biggest reason errors go unreported - but it’s based on outdated thinking. Modern safety systems reward reporting, not punish it.
How long does it take to hear back after reporting?
Internal hospital reports usually get a response within 7-14 days. FDA MedWatch does not guarantee a reply - but if your report helps identify a pattern, they may issue a public alert. ISMP sends acknowledgment emails and may follow up with safety alerts. If you don’t hear back in 30 days, follow up. Persistence saves lives.
Can I report an error from years ago?
Yes. The FDA and ISMP accept reports from any time. While recent reports are more useful for immediate action, historical reports still help identify long-term trends. For example, a 2020 report about a dangerous pill shape led to a redesign in 2024 because it matched other older reports. It’s never too late to speak up.
Medication errors are preventable. But only if we speak up. You’re not just protecting yourself. You’re protecting everyone who walks into a pharmacy, a clinic, or a school nurse’s office. Your report is the first step toward a safer system. Don’t wait. Don’t hesitate. Report it - today.

