Taking medication regularly isn’t just about remembering-it’s about making it automatic. If you’ve ever forgotten your pill, skipped a dose because it felt like a chore, or felt overwhelmed by a complex schedule, you’re not alone. Nearly half of people with chronic conditions don’t take their meds as prescribed. The result? More hospital visits, worse health, and avoidable suffering. But here’s the good news: you don’t need willpower to stick with it. You need behavioral tricks.
Turn Medication Into a Routine, Not a Task
Your brain doesn’t like decisions. It loves routines. When something becomes automatic, you don’t have to think about it. That’s the goal: make taking your medicine as natural as brushing your teeth. Start by tying your pill to an existing habit. This is called habit stacking. If you brush your teeth every morning at 7 a.m., take your pill right after. Same with dinner-take your evening meds right after washing your plate. These cues already live in your day. You’re not adding a new habit. You’re attaching your pill to one that’s already wired into your brain. A 2020 study in Patient Preference and Adherence found that people who paired their medication with a daily routine improved adherence by 15.8%. That’s not small. That’s the difference between missing a dose once a week versus once a month.Simplify Your Regimen
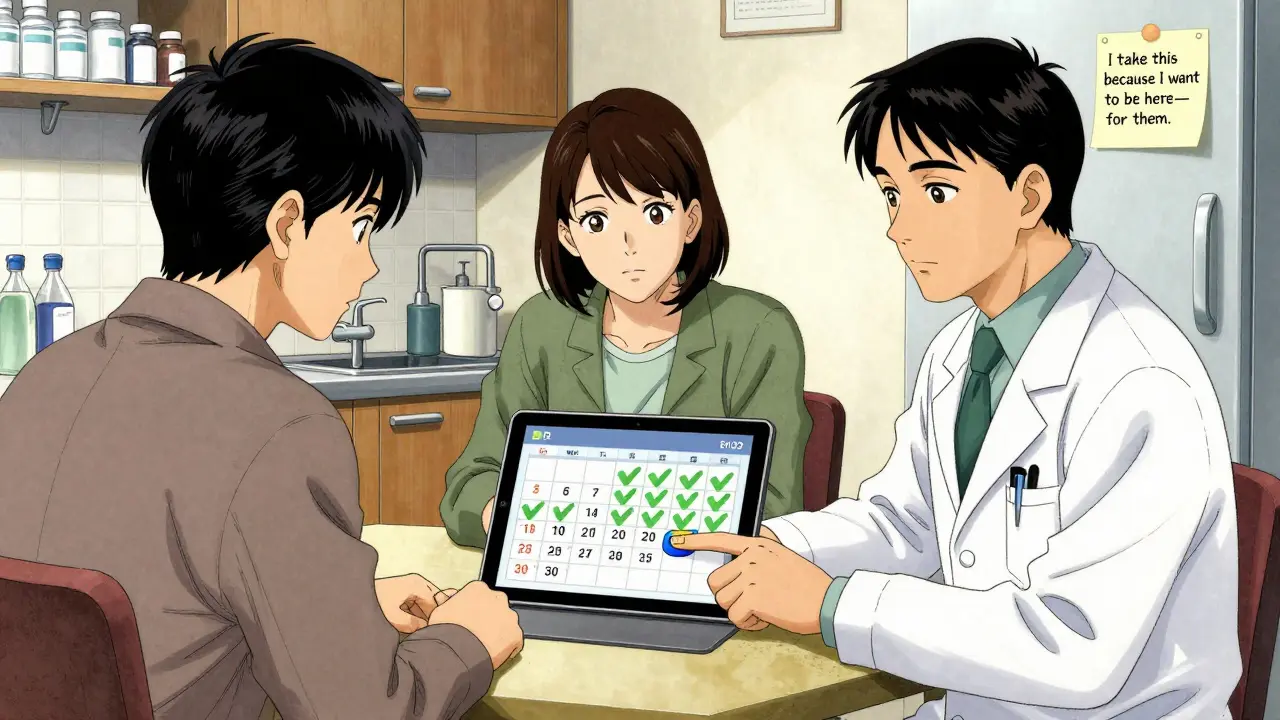
More pills = more chances to mess up. If you’re taking five different meds at three different times a day, your brain is overloaded. The solution isn’t just trying harder-it’s asking your doctor if you can simplify. Single-pill combinations (like a tablet that contains two drugs in one) cut down the number of pills you handle. A 2011 meta-analysis of over 21,000 patients showed these combinations increased adherence by 26%. That’s because fewer pills mean fewer decisions, fewer chances to forget, and less confusion. Ask: Can I reduce the number of daily doses? Some meds can be taken once instead of twice. Others can be switched to long-acting versions. A 2022 study in Schizophrenia Bulletin found that long-acting injectables (LAI) reduced non-adherence by 57% in patients with serious mental illness. That’s not magic-it’s design.Use Visual Cues and Tracking
Out of sight? Out of mind. A pill organizer isn’t just a container-it’s a memory tool. Use a seven-day pill box with clear labels. Fill it once a week. When you see an empty slot, you know you missed a dose. No guesswork. The Journal of the American Geriatrics Society found that elderly patients using weekly pill organizers reduced missed doses by 27%. But don’t stop there. Add a checklist. Every time you take your pill, mark an X on a calendar or in a small notebook. Visual feedback builds momentum. You’re not just taking medicine-you’re building a streak. Digital tools work too. Apps with customizable alarms, progress charts, and sync with your calendar can boost adherence by up to 28.7%, according to a 2021 meta-analysis in JMIR mHealth and uHealth. The best ones let you see your progress: a growing bar, a calendar filled with green checkmarks. It feels good to see progress.Set Specific Goals and Solve Problems Before They Happen
Vague goals like “I’ll take my meds better” don’t work. Specific ones do. Try this: “I will take my blood pressure pill at 7:15 a.m., right after I finish my coffee.” That’s measurable. That’s doable. Now, anticipate the obstacles. What happens if you’re traveling? If you’re out of pills? If you feel fine and think you don’t need it? Write down answers ahead of time:- If I’m traveling: I’ll pack a week’s supply in my carry-on with a copy of my prescription.
- If I run out: I’ll call my pharmacy 3 days before I’m empty.
- If I feel fine: I’ll remind myself that meds work even when I don’t feel symptoms.
Get Support That Actually Helps
You don’t have to do this alone. Pharmacists, nurses, and even family members can help-but only if they’re part of a team. A 2018 study in Patient Preference and Adherence found that when doctors, pharmacists, and nurses all give the same message-consistent timing, same reminders, same reasons-adherence jumps to 68%. Fragmented advice? It drops to 49%. Ask your pharmacist to set up auto-refills. A 2022 study in Medical Care showed this improved continuity by 33.4%. No more running out. No more last-minute trips. If cost is a problem, talk to your doctor. Financial incentives work. A 2022 study in Health Affairs found low-income patients improved persistence by 34.2% when they received small rewards for consistent refills. It’s not bribery-it’s removing a barrier.