Over 700,000 vertebral fractures happen each year in the U.S. alone, mostly due to osteoporosis. For many patients, traditional treatments like bracing or pain meds don’t cut it. That’s where kyphoplasty and vertebroplasty come in-two minimally invasive procedures that can restore mobility and relieve pain in just hours.
Vertebroplasty is a procedure where doctors inject medical-grade bone cement directly into a fractured vertebra. Using live X-ray guidance (fluoroscopy), a needle is threaded through the skin into the broken bone. The cement, made of polymethylmethacrylate (PMMA), hardens in 10-20 minutes to stabilize the fracture. The whole process takes 30-60 minutes. Patients typically go home the same day.
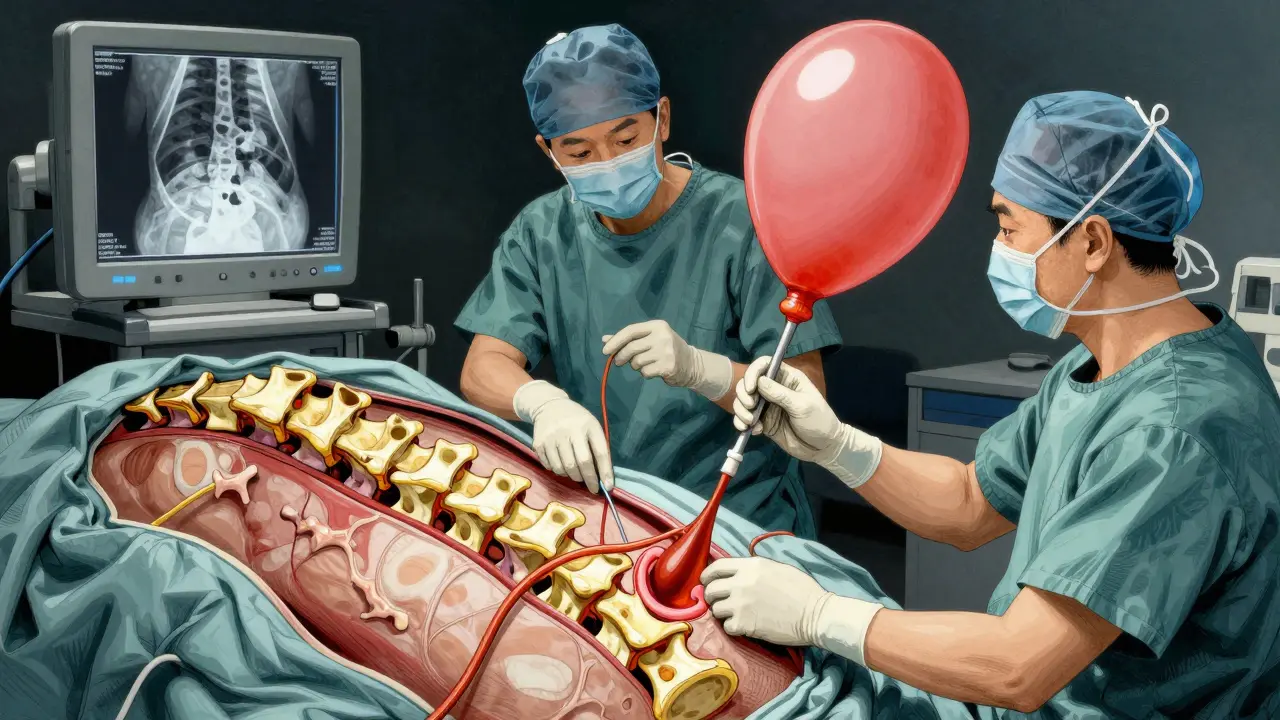
Kyphoplasty adds a step before cement injection. A small balloon is inserted into the fractured vertebra and inflated to lift the bone back into place and create a cavity. Once the balloon is deflated and removed, cement is injected into the space. This extra step helps restore height to the collapsed vertebra and reduces the risk of cement leakage.
Key Differences Between Kyphoplasty and Vertebroplasty
| Aspect | Kyphoplasty | Vertebroplasty |
|---|---|---|
| Height Restoration | 40-60% restoration of lost height | Minimal height restoration |
| Cement Leakage Risk | 9-33% | 27-68% |
| Average Cost (2023 Medicare) | $3,850 | $2,950 |
| Best For | Fractures with significant height loss (>30%) or deformity | Stable fractures without major deformity |
Both procedures use fluoroscopy for real-time imaging during the procedure. Radiation exposure averages 3-5 mSv-similar to standard lumbar spine X-rays. The cement used in both cases is PMMA, which hardens quickly to provide immediate stability. However, kyphoplasty’s balloon step creates a controlled cavity, lowering cement leakage risk compared to vertebroplasty’s direct injection under higher pressure.
Who Is a Candidate for Each Procedure?
Doctors consider several factors when choosing between kyphoplasty and vertebroplasty. For vertebral compression fracture patients with significant height loss (over 30%) or visible spinal deformity (kyphosis), kyphoplasty is usually preferred. The balloon step helps restore height and correct the curve, which vertebroplasty can’t do.
Vertebroplasty works well for stable fractures without major height loss. It’s often chosen when cost is a concern or when the fracture is less severe. Both procedures require confirmation of an acute fracture-usually through MRI showing bone marrow edema-to ensure the fracture is active and treatable. Chronic fractures without inflammation aren’t suitable for either procedure.
Recovery and Outcomes
Most patients go home the same day after both procedures. Light activities like walking are encouraged within 24 hours. Full recovery typically takes 1-2 weeks. Studies show 85-90% of patients experience immediate pain relief, dropping from an average pre-procedure pain score of 8.2 to 1.5 on a 10-point scale within 24 hours.
On Healthgrades, kyphoplasty averages 4.6/5.0 from 1,247 reviews, with 89% reporting immediate pain relief. Vertebroplasty averages 4.4/5.0 from 842 reviews, with 86% reporting similar relief. A Reddit user shared, "Kyphoplasty felt like flipping a switch-I went from 9/10 pain to 2/10 within hours." Another noted, "Vertebroplasty reduced my pain, but didn’t fix my hunched posture."
Risks and Complications
The biggest risk for both procedures is bone cement leakage. Vertebroplasty has a higher leakage rate (27-68%) compared to kyphoplasty (9-33%). Symptomatic leakage-where cement causes nerve compression or other issues-occurs in about 1.1% of vertebroplasty cases versus 0.6% for kyphoplasty.
Other rare risks include infection (less than 0.5%), nerve damage, or new fractures in adjacent vertebrae (5-10% within 12 months). Both procedures are considered safe when performed by trained specialists. The Society of Interventional Radiology recommends at least 15-20 supervised cases for doctors to become proficient, with kyphoplasty having a slightly steeper learning curve due to balloon manipulation.
Insurance and Cost Considerations
Medicare covers both procedures with approval rates over 95% when patients have tried conservative treatments (like bracing or physical therapy) for 4-6 weeks without success. Kyphoplasty costs about 20-30% more than vertebroplasty-$3,850 vs. $2,950 in 2023 Medicare reimbursement rates. However, this cost difference often reflects the added complexity of the balloon step and potential for better height restoration.
For patients with osteoporosis, managing the underlying condition is critical. Both procedures treat the fracture but don’t prevent future ones. Doctors usually recommend bone-strengthening medications and lifestyle changes after the procedure to reduce recurrence risk.
Frequently Asked Questions
Which procedure is better for osteoporosis-related fractures?
Both work well, but kyphoplasty is often preferred for fractures with significant height loss or deformity. Vertebroplasty is suitable for stable fractures without major collapse. Pain relief is similar in both cases-around 85-90% of patients experience immediate improvement.
How long does recovery take?
Most patients go home the same day. Light activities like walking are possible within 24 hours. Full recovery typically takes 1-2 weeks. Studies show 92% of patients return to normal activities within 72 hours. Avoid heavy lifting for 4-6 weeks to let the cement fully set.
What are the main risks?
Cement leakage is the most common risk (27-68% for vertebroplasty, 9-33% for kyphoplasty). Serious complications like nerve damage or pulmonary embolism are rare (under 1%). New fractures in adjacent vertebrae occur in 5-10% of cases within a year. Proper patient selection and skilled surgeons minimize these risks.
Are these procedures covered by insurance?
Yes, Medicare and most private insurers cover both if conservative treatments (bracing, physical therapy, pain meds) failed for at least 4-6 weeks. Approval rates exceed 95% with proper documentation. Always check with your insurer beforehand-some require pre-authorization.
Do these procedures prevent future fractures?
No, they treat existing fractures but don’t prevent new ones. Osteoporosis management is essential-this includes calcium/vitamin D supplements, bone-strengthening medications like bisphosphonates, and fall prevention strategies. Without addressing the root cause, future fractures are likely.


Dr. Sara Harowitz
February 5, 2026 AT 09:29Kyphoplasty is clearly superior! Vertebroplasty is outdated and dangerous!! It's irresponsible to still use it. Kyphoplasty should be the standard!
Kieran Griffiths
February 6, 2026 AT 08:13Both procedures have their place. For stable fractures, vertebroplasty is cost-effective. For deformities, kyphoplasty is better. Always consult your specialist!
Tehya Wilson
February 6, 2026 AT 16:51The data shows higher cement leakage in vertebroplasty. However, the procedure remains common. Perhaps due to cost factors. Not ideal.
anjar maike
February 7, 2026 AT 04:33Kyphoplasty's balloon step helps restore height 😊 but costs more. Vertebroplasty has higher leakage risk 😕
Bella Cullen
February 8, 2026 AT 17:21Kyphoplasty is better for height loss, but vertebroplasty is cheaper. Not sure if it's worth it. Meh.
Cullen Bausman
February 10, 2026 AT 12:32The cost difference is negligible for the improved outcomes of kyphoplasty. It's the responsible choice.
Arjun Paul
February 11, 2026 AT 01:06Vertebroplasty's high leakage rate (27-68%) is unacceptable. Kyphoplasty should be standard.
divya shetty
February 12, 2026 AT 12:00Patients must be informed about the risks. Both procedures carry dangers. The healthcare system prioritizes profit over patient safety.
Phoebe Norman
February 14, 2026 AT 02:21PMMA cement leakage risk is significantly higher in vertebroplasty.
Albert Lua
February 14, 2026 AT 08:11In India, kyphoplasty is becoming popular. But access is limited. Cost is a barrier. We need more affordable options globally.
Lana Younis
February 14, 2026 AT 16:10Kyphoplasty's balloon step is a game-changer for height restoration. But cost-wise, vertebroplasty is still a solid choice for some cases. Just need to manage expectations. Oh and, the cement leakage rates are way different. But overall, both are great options.
Samantha Beye
February 15, 2026 AT 08:48These procedures offer hope for patients with vertebral fractures. Each has its strengths depending on the patient's needs. Always best to discuss with your doctor.
Diana Phe
February 16, 2026 AT 20:12Insurance companies push kyphoplasty solely for profit.
Andre Shaw
February 17, 2026 AT 10:51Actually, most people don't realize that vertebroplasty is just as effective as kyphoplasty for many cases. The balloon step is overhyped. Plus, the higher cost is just a money grab. Call me crazy, but I've seen better results with vertebroplasty.
Kate Gile
February 17, 2026 AT 18:54Both procedures have their merits. It's all about the individual patient's situation. We should celebrate advancements in minimally invasive care!