When you're taking lithium for bipolar disorder, even small changes in your body can push your lithium levels into dangerous territory. It's not just about the pill you take every morning-it's about what else you're taking, how much water you're drinking, and even how much salt you're eating. Lithium has a very narrow window where it works safely: between 0.6 and 1.2 mmol/L. Go just a little above that, and you risk serious, even life-threatening toxicity. And the biggest threats? Common medications like NSAIDs and diuretics-and something as simple as not drinking enough water.
Why Lithium Is So Sensitive
Lithium doesn't break down in your body. About 95% of it leaves through your kidneys, unchanged. That means anything that affects how your kidneys work can change how much lithium stays in your blood. If your kidneys slow down-even a little-lithium builds up. And because the difference between a therapeutic dose and a toxic one is so small, even minor changes can be dangerous. This is why people over 65, those with kidney problems, or anyone with heart failure are at much higher risk. Studies show older adults have more than three times the risk of lithium toxicity compared to younger patients. It’s not just age-it’s how the body changes with age. Kidneys don’t filter as well. Blood volume drops. And the body holds onto sodium and water differently.NSAIDs: The Silent Lithium Boosters
NSAIDs-like ibuprofen, naproxen, and diclofenac-are among the most common drugs people take for headaches, arthritis, or back pain. But if you're on lithium, they can be risky. These drugs block prostaglandins, chemicals your kidneys use to keep blood flow steady. When prostaglandins drop, your kidneys filter less blood. That means less lithium gets flushed out. Lithium levels can jump 25% to 60% within just a few days of starting an NSAID. Not all NSAIDs are the same. Indomethacin is the worst offender-it can spike lithium levels by up to 60%. Ibuprofen raises them by 25-40%. Celecoxib is a bit safer, but still risky, with increases of 15-30%. Even occasional use can be dangerous, but regular use is far more problematic. One fatal case in New Zealand involved a 72-year-old woman taking lithium, an ACE inhibitor, and an NSAID. Her lithium levels weren't checked regularly. She developed severe toxicity and died. That’s not rare. It’s a warning.Diuretics: The Big Problem with Thiazides
Diuretics help lower blood pressure by making you pee more. But they also change how your kidneys handle lithium. Thiazide diuretics-like hydrochlorothiazide-are the biggest concern. They cause lithium levels to rise by 25-50% within 7 to 10 days. That’s fast. And the rise doesn’t stop after a few days-it keeps climbing if you keep taking them. Loop diuretics like furosemide are less likely to cause big spikes, but they still raise lithium levels by 10-25%. That’s enough to cause symptoms like dizziness, tremors, or confusion. Potassium-sparing diuretics like spironolactone? The data is mixed. Some studies show small increases, others show no effect. But because the risk isn’t zero, doctors still advise caution. And then there are the ones that actually lower lithium: osmotic diuretics like mannitol and carbonic anhydrase inhibitors like acetazolamide. These reduce lithium levels by 15-30%. That’s dangerous too-because now your mood might become unstable.Herbal Diuretics? Don’t Be Fooled
You might think “natural” means safe. But herbal weight-loss teas, supplements labeled as “detox” or “water pills,” and even some traditional remedies can contain diuretic herbs like dandelion, parsley, or hibiscus. These work the same way as prescription diuretics-they make you lose fluid and salt. In one case, a patient on lithium started taking a popular herbal tea for weight loss. Within two weeks, her lithium levels doubled. She ended up in the hospital with confusion and vomiting. She didn’t tell her doctor about the tea because she thought it was “just herbal.” If you’re on lithium, assume every herbal product that makes you pee more is risky. Always check with your prescriber before taking anything labeled as a “natural diuretic.”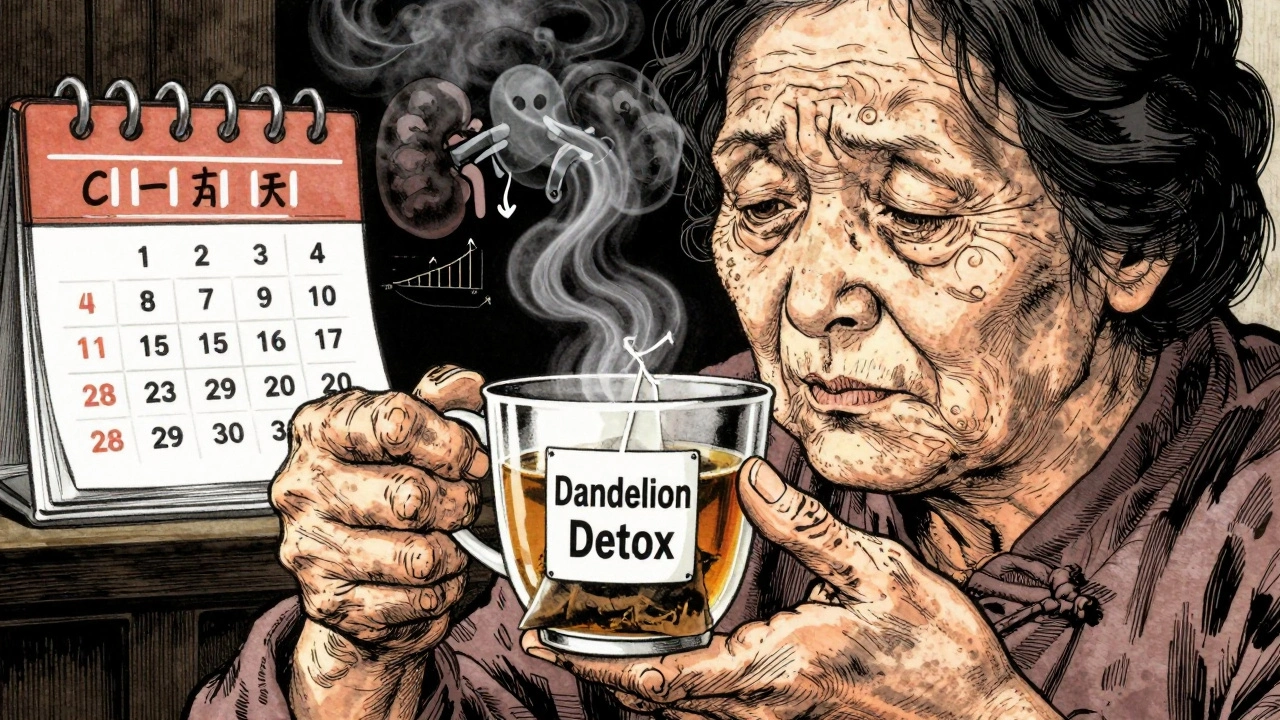
Dehydration: The Hidden Trigger
Lithium is carried in your blood. When you lose water-through sweating, vomiting, diarrhea, or just not drinking enough-your blood gets thicker. That means the same amount of lithium is now in less fluid. Your lithium concentration rises. Even mild dehydration-losing just 2-3% of your body weight in water-can increase lithium levels by 15-25%. That’s enough to trigger symptoms. This is why travel is risky. Long flights, hot weather, or illness like gastroenteritis can leave you dehydrated without you realizing it. The NHS and Medsafe both warn that people on lithium traveling to hot climates or with stomach bugs need extra care. You don’t need to drink 10 glasses of water a day. But you do need to drink enough to keep your urine pale yellow. If it’s dark, you’re not drinking enough.Salt Matters More Than You Think
Your body holds onto lithium when it holds onto sodium. So if you suddenly eat less salt-maybe you’re trying to go low-sodium for your heart-your lithium levels can climb. Conversely, eating more salt can lower lithium levels. A change of 20-30 mmol of sodium per day (about 1-1.5 teaspoons of salt) can shift lithium levels by 10-20%. That’s why consistency matters. Don’t go from eating lots of salty snacks to a strict low-salt diet without telling your doctor. And don’t suddenly start using salt substitutes-they often contain potassium, which can also interfere with lithium.What to Do If You Need an NSAID or Diuretic
Sometimes you can’t avoid these drugs. Maybe you have arthritis and need ibuprofen. Or you have high blood pressure and your doctor says you need a diuretic. Here’s what to do:- Always tell your psychiatrist or GP you’re on lithium before starting any new medication-even over-the-counter ones.
- Ask if there’s a safer alternative. For pain, acetaminophen (paracetamol) is usually fine with lithium.
- If you must take an NSAID or diuretic, your lithium level should be checked within 5-7 days and again at 2-4 weeks.
- Reduce your lithium dose before starting the new drug if your doctor advises it.
- Never stop your lithium suddenly. Even if you feel fine, stopping can cause a relapse of mania or depression.
Recognizing Lithium Toxicity Early
Toxicity doesn’t always come with a siren. Early signs are easy to miss:- Diarrhea (68% of early cases)
- Lightheadedness or dizziness (52%)
- Drowsiness or fatigue (47%)
- Tremors in your hands
- Nausea or vomiting
- Blurred vision (31%)
- Ringing in the ears (tinnitus, 29%)
- Loss of coordination
- Seizures or coma (in severe cases)
Monitoring Is Non-Negotiable
Regular blood tests are the only way to know your lithium level is safe. Guidelines say:- Check lithium levels before starting any new medication that could interact.
- Test again 5-7 days after starting an NSAID or diuretic.
- Test again at 2-4 weeks.
- Test every 3-6 months if you’re stable, but more often if you’re elderly or have kidney issues.
Bottom Line: Stay Informed, Stay Hydrated, Stay Connected
Lithium saves lives. But it demands respect. It’s not just a mood stabilizer-it’s a drug that reacts to your body’s changes. NSAIDs, diuretics, dehydration, and salt changes aren’t small things. They’re red flags. If you’re on lithium:- Drink water regularly, especially when sick, hot, or traveling.
- Avoid NSAIDs unless your doctor says it’s safe-and even then, use the lowest dose for the shortest time.
- Never start a new diuretic, herbal product, or salt substitute without checking in.
- Know the early signs of toxicity.
- Keep your blood tests on schedule.
Can I take ibuprofen if I’m on lithium?
Ibuprofen can raise lithium levels by 25-40%, increasing your risk of toxicity. It’s not completely off-limits, but only use it if absolutely necessary, at the lowest dose, and for the shortest time. Always check your lithium level 5-7 days after starting it. Ask your doctor about acetaminophen (paracetamol) as a safer alternative for pain.
Do all diuretics affect lithium the same way?
No. Thiazide diuretics like hydrochlorothiazide are the most dangerous-they can spike lithium levels by 25-50%. Loop diuretics like furosemide cause smaller increases (10-25%). Potassium-sparing diuretics like spironolactone have unclear effects, but caution is still advised. Osmotic and carbonic anhydrase inhibitors like mannitol or acetazolamide actually lower lithium levels, which can make your mood unstable.
How much water should I drink daily if I’m on lithium?
There’s no magic number, but aim to keep your urine pale yellow. Drink regularly throughout the day, especially if you’re sweating, sick, flying, or in hot weather. Losing just 2-3% of your body weight in water can raise lithium levels by 15-25%. Don’t wait until you’re thirsty-thirst means you’re already slightly dehydrated.
Can I use herbal diuretics like dandelion tea while on lithium?
No. Herbal diuretics-whether in teas, capsules, or weight-loss supplements-work the same way as prescription ones. They increase urine output and reduce sodium, which can cause lithium levels to rise dangerously. Many people don’t realize these products are risky because they’re labeled “natural.” Always tell your doctor about every supplement you take.
What should I do if I start feeling dizzy or shaky on lithium?
Stop taking any new medications or supplements immediately. Drink water and contact your doctor or go to urgent care. Dizziness, tremors, nausea, or diarrhea are early signs of lithium toxicity. Don’t wait for worse symptoms. Early action can prevent permanent kidney damage or worse.
Does salt intake really affect lithium levels?
Yes. Your body holds onto lithium when it holds onto sodium. Eating less salt can raise lithium levels by 10-20%. Eating more salt can lower them. That’s why consistency matters. Don’t suddenly switch from a salty diet to a low-salt one-or vice versa-without telling your doctor. Avoid salt substitutes too; they often contain potassium, which can interfere with lithium.
How often should lithium levels be checked?
When starting lithium, levels are checked weekly until stable. After that, every 3-6 months is typical. But if you start a new medication like an NSAID or diuretic, check within 5-7 days and again at 2-4 weeks. If you’re over 65, have kidney issues, or take multiple interacting drugs, check every 1-3 months. Never skip tests just because you feel fine.


Jennifer Taylor
December 12, 2025 AT 05:38So let me get this straight - if I drink a cup of coffee and forget my water bottle on a flight, I could OD on lithium? 😳 I’m not even on it and I’m sweating just reading this. Who the hell thought it was a good idea to make a mood stabilizer this finicky? It’s like your brain is a microwave and lithium is the soup - one wrong setting and BOOM, you’re a human volcano.
Jade Hovet
December 13, 2025 AT 02:17OMG I JUST REALIZED I TOOK IBUPROFEN LAST WEEK FOR MY HEADACHE 😭 I’M SO SCARED RN. I’M ON LITHIUM AND I THOUGHT IT WAS JUST ‘NORMAL PAIN RELIEF’ 😫 I’M CALLING MY DOCTOR RIGHT NOW. THANK U FOR THIS POST!! 💕🙏
Ronan Lansbury
December 13, 2025 AT 12:05Of course the pharmaceutical-industrial complex wants you to believe this is about ‘safety.’ Meanwhile, the real agenda is to keep you dependent - lithium is cheap, but monitoring? Blood tests? Doctor visits? That’s where the money is. And don’t get me started on how NSAIDs are ‘dangerous’ - they’re just cheaper than the patented alternatives. They want you scared, docile, and paying for unnecessary labs every month. Wake up.
nithin Kuntumadugu
December 14, 2025 AT 16:15LMAO so now even dandelion tea is a bioweapon? 🤡 I’m from India, we’ve been drinking this since before your great-grandma was born. And now some American psychiatrist says ‘avoid herbal diuretics’? Bro, if your meds break because of a leaf, maybe your meds are the problem. Also, who checks lithium levels every 3 months? My doctor forgot I exist after the first refill.
sharon soila
December 14, 2025 AT 17:26Thank you for sharing this with such clarity. This is not just medical advice - it’s life-saving wisdom. If you're on lithium, your body is a delicate ecosystem. Water, salt, sleep, stress - they all matter. You are not broken for needing this care. You are brave for managing it. Please, please, drink that water. Get your labs. Tell your doctor about that tea. You deserve to feel stable - not scared.
Keasha Trawick
December 14, 2025 AT 22:38Let’s talk about renal clearance kinetics and sodium-lithium cotransport in the distal tubule - because this isn’t just ‘drink more water,’ it’s about nephron-level pharmacodynamics. NSAIDs inhibit COX-1/2 → reduce PGE2 → afferent arteriole vasoconstriction → GFR drop → lithium retention. Thiazides? They upregulate ENaC channels in the collecting duct, mimicking aldosterone. And don’t even get me started on how osmotic diuretics alter tubular fluid osmolality. This is why we need nephrology consults, not just ‘take a pill.’
Webster Bull
December 16, 2025 AT 21:06Drink water. Don't take random pills. Tell your doc everything. Simple. Done.
Bruno Janssen
December 18, 2025 AT 03:56I didn’t even know I was on lithium until my mom found the bottle in my drawer. She cried. I didn’t. I just took it. Now I’m scared to drink coffee. Or sweat. Or breathe. What if I die in my sleep because I didn’t drink enough water? I’m not even sure I want to live anymore.
Tommy Watson
December 19, 2025 AT 16:10So you’re telling me I can’t take Advil for my back pain? What am I supposed to do, just suffer? And now I can’t even have a beer because it makes me pee? This is ridiculous. I’ve been on lithium for 10 years and I’m fine. Why are you scaring people? This feels like fear-mongering.
Donna Hammond
December 20, 2025 AT 14:41Thank you for writing this with such precision and care. I’m a nurse who works with geriatric psych patients, and I see this every day - people on lithium who don’t realize their joint pain meds are slowly poisoning them. The most heartbreaking part? They never tell their doctors because they think it’s ‘just a little ibuprofen.’ Please, if you’re reading this - speak up. Your life depends on it. And if you’re a provider - don’t assume they know. Ask. Always ask.
Sheldon Bird
December 22, 2025 AT 02:26Hey, I get it - lithium is tricky. But don’t let fear stop you from living. I’ve been on it for 8 years. I drink water, I check my labs, I tell my doc about every new thing I take. It’s not perfect, but it’s manageable. You’re not alone. And yes, you can still enjoy life - just be smart about it. 💪💧
Karen Mccullouch
December 23, 2025 AT 10:33Who let this article get published? This is anti-American propaganda. In the US, we don’t need to be told what to drink or what pills to avoid. We’re free! If you want to take lithium, fine - but stop trying to control everyone else’s choices with fear tactics. This is just Big Pharma’s way of keeping you weak and dependent. America doesn’t need this.
Michael Gardner
December 25, 2025 AT 01:44Actually, I’ve been on lithium for 15 years and I take ibuprofen weekly. My levels are always fine. I’ve had 12 blood tests. All normal. So maybe the real problem isn’t the drugs - it’s the overcautious medical culture that treats patients like fragile glass. Not everyone’s a 72-year-old with kidney disease. Some of us are young and healthy. Don’t generalize.
Willie Onst
December 27, 2025 AT 00:02Hey, I’m from the U.S., but my grandma’s from Nigeria - she used to say, ‘If your medicine needs a whole book to explain how not to kill you, maybe it’s not the medicine - it’s the system.’ I don’t know if that’s true, but I do know I drink water, I check in with my doc, and I don’t let fear rule me. We’re all just trying to stay human in a world that makes it hard. Keep it real, keep it safe.