When you’re facing a cancer diagnosis, one of the most confusing decisions isn’t just what treatment to get - it’s when. Should you start chemotherapy or immunotherapy before surgery, or wait until after? This isn’t just a matter of preference. It’s a strategic choice that can change your chances of survival, your recovery time, and even your quality of life. For many cancers - especially lung and breast cancer - doctors now have two clear paths: neoadjuvant therapy (before surgery) or adjuvant therapy (after surgery). And the answer isn’t always the same for everyone.
What’s the Difference Between Neoadjuvant and Adjuvant Therapy?
Think of it this way: neoadjuvant therapy is like preparing the ground before building a house. You clear out the big obstacles, make the foundation stronger, and see how the materials react. That’s what neoadjuvant therapy does - it’s treatment given before surgery to shrink the tumor, kill hidden cancer cells, and test how your body responds. If the tumor shrinks dramatically, that’s a good sign. If it doesn’t, your doctors can switch strategies before cutting into you.
Adjuvant therapy, on the other hand, is like cleaning up after the house is built. Surgery removes the visible tumor, but there might still be stray cancer cells hiding in your body. Adjuvant therapy - chemo, immunotherapy, or radiation - comes after surgery to mop up those leftovers. It’s preventative. You’re not trying to shrink anything anymore. You’re trying to stop it from coming back.
The big difference? Neoadjuvant lets you see how your cancer responds in real time. Adjuvant doesn’t.
Why Neoadjuvant Therapy Is Changing the Game
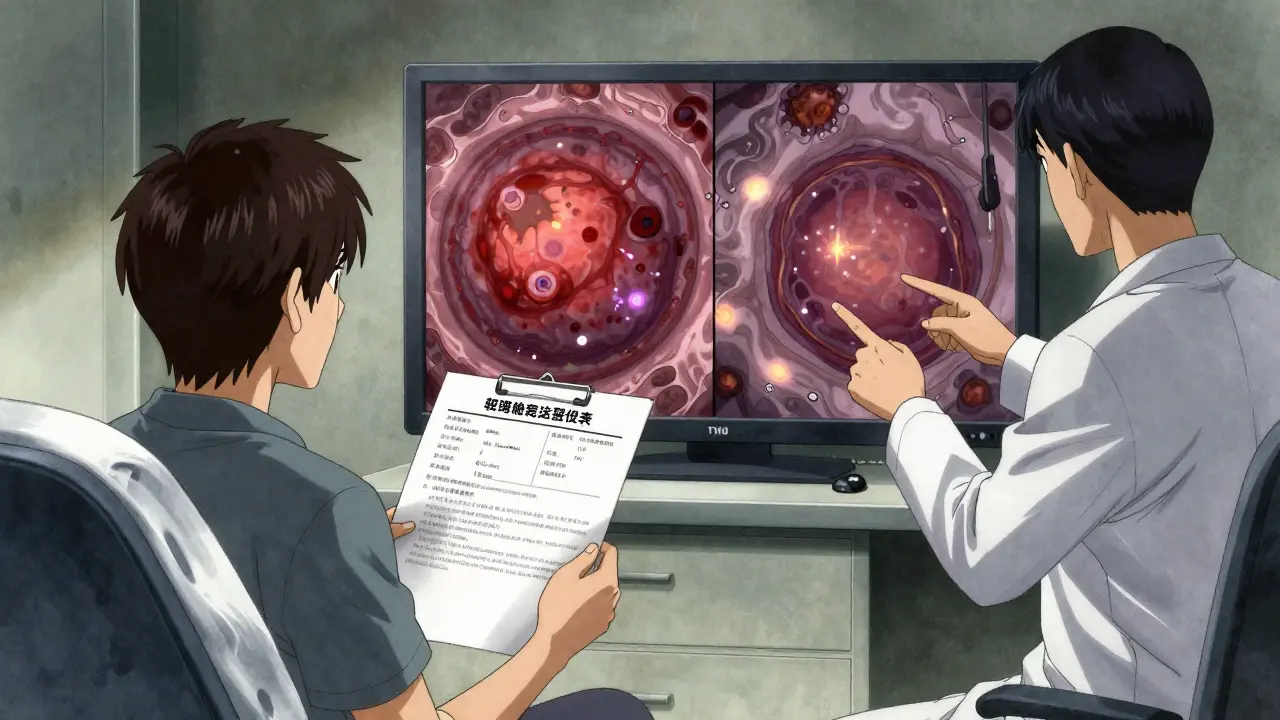
In the past, doctors mostly used adjuvant therapy. But over the last decade, especially with the rise of immunotherapy, neoadjuvant has become a game-changer. The landmark CheckMate 816 trial, published in 2022, showed that for patients with resectable non-small cell lung cancer (NSCLC), giving nivolumab (an immunotherapy drug) plus chemotherapy before surgery led to a 24% pathologic complete response (pCR) rate - meaning no live cancer cells were found in the removed tumor. That’s compared to just 2.2% with chemo alone.
That’s huge. A pCR doesn’t just mean the tumor shrank - it means your body’s immune system is actively fighting the cancer. And patients who achieve pCR have significantly better long-term survival. In fact, the same trial showed a 37% improvement in event-free survival compared to chemo-only.
For triple-negative breast cancer (TNBC), another aggressive type, neoadjuvant chemo leads to pCR in 30-40% of cases. And those patients? They’re far less likely to relapse than those who don’t respond. That’s why oncologists now use neoadjuvant therapy not just to shrink tumors, but to predict outcomes. If your tumor doesn’t respond, you know early - and you can plan your next steps without delay.
When Adjuvant Therapy Still Makes Sense
But neoadjuvant isn’t right for everyone. Some patients prefer to get surgery done first - especially if they’re worried about the cancer spreading while waiting for treatment. Others have tumors that are already small and easy to remove. In those cases, adjuvant therapy is simpler and avoids the risks of delaying surgery.
There’s also the issue of side effects. Neoadjuvant therapy can cause fatigue, low blood counts, or immune-related reactions. About 10-15% of patients end up needing surgery delayed because their body can’t handle the treatment. And in 5-10% of lung cancer cases, the cancer keeps growing during neoadjuvant therapy - meaning surgery might not even be possible anymore.
For some patients, especially those with early-stage, low-risk tumors, the benefits of waiting don’t outweigh the risks. Adjuvant therapy avoids that uncertainty. You get the tumor out, then hit the leftovers. No waiting. No anxiety about progression.

Is More Better? The Big Question: Neoadjuvant + Adjuvant?
Here’s where things get tricky. After seeing how well neoadjuvant immunotherapy works, many doctors started adding more - giving immunotherapy after surgery too. The idea? Double down. Keep the immune system fired up.
But a major 2024 meta-analysis of over 3,200 patients across four major trials found something surprising: adding adjuvant immunotherapy didn’t improve survival. It didn’t help event-free survival. It didn’t help overall survival. What it did do? Increase severe side effects. Patients on the combo therapy had nearly twice the rate of serious treatment-related problems compared to those who stopped after neoadjuvant.
One oncologist put it bluntly: “If you already saw your tumor shrink dramatically with neoadjuvant therapy, why keep giving toxic drugs after?”
Now, guidelines are shifting. The American Society of Clinical Oncology (ASCO) updated its 2023 recommendations to say that for many patients, neoadjuvant therapy alone may be enough. The goal isn’t just to treat - it’s to treat smart.
Who Gets Which Treatment? The Rules Are Getting Clearer
There’s no one-size-fits-all, but here’s what current guidelines say:
- For NSCLC (lung cancer): If you have stage IB (tumor ≥4 cm) to IIIA, neoadjuvant chemoimmunotherapy is now the standard. The FDA approved nivolumab + chemo for this in 2022. PD-L1 expression ≥1% helps predict who benefits most.
- For breast cancer: Neoadjuvant therapy is recommended for triple-negative, HER2-positive, or large hormone-receptor-positive tumors. It’s not just about shrinking - it’s about finding out if the cancer is aggressive. If you get a pCR, your prognosis is much better. If not, your doctor can switch to stronger drugs after surgery.
- For other cancers: Melanoma, esophageal, and some colorectal cancers are also starting to use neoadjuvant approaches, especially with immunotherapy.
And timing matters. Neoadjuvant therapy usually lasts 3-4 cycles over 9-12 weeks. Surgery follows 3-6 weeks after the last dose - giving your body time to recover. Adjuvant therapy typically runs for 4-6 months after surgery.
What Patients Are Saying
Real people are making these choices every day. One lung cancer patient from Ohio said: “My oncologist said, ‘Let’s see if the drugs work before we cut.’ I was scared - what if it doesn’t work? But when the pathology report came back showing 90% tumor kill, I felt like I’d already won.”
Another, with early-stage breast cancer, chose adjuvant chemo because she didn’t want to wait. “I just wanted it gone,” she said. “Later, I learned I might have benefited from knowing how my tumor responded. But I didn’t want to risk anything.”
A 2023 survey found 62% of NSCLC patients on neoadjuvant therapy felt anxious about the waiting period. But 78% of oncologists now offer it - up from 42% just three years ago. That shift tells you something: doctors are seeing the results, and patients are trusting the process.
The Future: Personalized Sequencing
The next big leap isn’t just choosing neoadjuvant or adjuvant. It’s using biomarkers to decide who needs what - and when.
Right now, doctors look at tumor size, type, and PD-L1 levels. Soon, they’ll be checking circulating tumor DNA (ctDNA) in your blood. If ctDNA is still present after neoadjuvant therapy, that’s a red flag - your cancer might be hiding. You’d get more treatment. If it’s gone? You might not need adjuvant at all.
Trials like NeoADAURA (testing osimertinib for EGFR-mutant lung cancer) and KEYNOTE-867 (comparing neoadjuvant-only vs. neoadjuvant-plus-adjuvant) are already underway. Results will be out by 2025-2026.
Experts predict that within five years, 70% of early-stage lung cancer patients will get neoadjuvant therapy tailored to their tumor’s genetics - and adjuvant therapy will be reserved only for those who show signs of lingering disease.
Bottom Line: It’s Not About Which Is Better - It’s About Which Is Right for You
Neoadjuvant therapy isn’t “better” than adjuvant. It’s different. It’s more informative. It’s more proactive. But it’s not for everyone.
If your tumor is large, aggressive, or hard to remove, neoadjuvant gives you a chance to shrink it, test the drugs, and improve your odds. If your cancer is small and slow-growing, adjuvant therapy might be simpler and just as effective.
The key is to ask your oncology team: What are we trying to achieve here? Are we trying to shrink the tumor? Predict outcomes? Prevent recurrence? The answer will guide the sequencing.
And remember - this isn’t a one-time decision. Your treatment plan can change based on what we learn along the way. That’s the power of modern oncology. It’s not just about fighting cancer. It’s about learning from it.
Is neoadjuvant therapy always better than adjuvant therapy?
No. Neoadjuvant therapy isn’t always better - it’s just more informative. It’s best for larger, more aggressive tumors where shrinking the cancer before surgery improves outcomes. For small, low-risk tumors, adjuvant therapy after surgery can be just as effective with fewer delays and less risk of treatment-related complications. The choice depends on cancer type, stage, biomarkers, and patient preference.
What is a pathologic complete response (pCR), and why does it matter?
A pathologic complete response (pCR) means no live cancer cells are found in the tumor after neoadjuvant therapy and surgery. It’s the strongest predictor of long-term survival in cancers like triple-negative breast cancer and non-small cell lung cancer. Patients who achieve pCR have significantly lower chances of recurrence and better survival rates - sometimes doubling their odds compared to those who still have cancer cells present.
Does immunotherapy after surgery improve survival?
Recent large studies show it doesn’t - at least not for most patients. A 2024 meta-analysis of over 3,200 patients found no improvement in survival when immunotherapy was added after neoadjuvant therapy. Instead, it increased serious side effects. For patients who already had a strong response to neoadjuvant immunotherapy, continuing treatment after surgery may be unnecessary and harmful. Guidelines now suggest stopping after neoadjuvant unless there’s evidence of remaining cancer.
How long does neoadjuvant therapy last before surgery?
Typically, neoadjuvant therapy lasts 3 to 4 cycles over 9 to 12 weeks. For example, in lung cancer, patients receive chemotherapy and immunotherapy every 3 weeks for 3-4 cycles. Surgery is scheduled 3 to 6 weeks after the last dose to allow recovery from side effects like fatigue or low blood counts. Timing is critical - too soon and your body isn’t ready; too late and the cancer might start growing again.
Can I still have surgery if the tumor doesn’t shrink during neoadjuvant therapy?
Yes - but the decision depends on whether the cancer is still operable. Even if the tumor doesn’t shrink much, surgery may still be possible and beneficial. The key is whether the cancer is stable or growing. If it’s growing during treatment, doctors may switch therapies before surgery. If it’s stable, surgery can proceed. The goal isn’t just shrinkage - it’s to see how the cancer behaves, which helps guide future treatment.
What are the risks of delaying surgery for neoadjuvant therapy?
The main risk is that the cancer could progress during treatment - which happens in about 5-10% of lung cancer cases. Also, side effects like low blood counts or immune reactions can delay surgery in 10-15% of patients. That’s why close monitoring with scans and blood tests is essential. If the tumor grows or you develop severe side effects, your team may move forward with surgery earlier than planned. The benefits usually outweigh the risks, but it’s not risk-free.
What Comes Next?
If you’re considering neoadjuvant therapy, ask your team about:
- What’s the goal of treatment - shrinkage, response assessment, or both?
- What biomarkers are being tested? (PD-L1, ctDNA, tumor mutational burden)
- What happens if the tumor doesn’t respond?
- Will you need adjuvant therapy after surgery - and why?
- How will your response be tracked during treatment?
The future of cancer treatment isn’t about choosing between before or after. It’s about using every tool - surgery, drugs, and data - to personalize the sequence. And that’s exactly what makes today’s oncology so powerful.

Pawan Chaudhary
December 17, 2025 AT 22:34Really helpful breakdown! I’ve been through this with my mom and the whole before/after thing felt overwhelming until I read this. Glad to see doctors are finally thinking smarter, not just harder.
Linda Caldwell
December 18, 2025 AT 20:31YES. I had neoadjuvant for TNBC and got a pCR. That report was the best day of my life. No chemo after. Just healing. Trust the process, trust your docs, trust your body.
Salome Perez
December 19, 2025 AT 06:45It’s fascinating how oncology has evolved from a blunt instrument to a precision art. The shift from reactive to predictive medicine isn’t just clinical-it’s philosophical. We’re no longer treating disease; we’re engaging in a dialogue with biology. The tumor, in its response, speaks volumes. And we’re finally learning to listen.
Philippa Skiadopoulou
December 21, 2025 AT 01:45The data supporting neoadjuvant immunotherapy in NSCLC is robust and should inform standard practice. Adjuvant continuation lacks benefit and adds toxicity. Guidelines reflect this. Patients deserve evidence-based sequencing, not protocol inertia.
Kaylee Esdale
December 22, 2025 AT 13:09My aunt got neoadjuvant for stage III breast cancer. She didn’t get a pCR but they changed her post-op plan based on what they saw. She’s now in remission. This isn’t one-size-fits-all. It’s one-size-fits-HER2-or-TNBC-or-PD-L1. Knowledge is power.
Kent Peterson
December 24, 2025 AT 09:42Wait… so you’re telling me the FDA approved this based on a single trial? And now we’re all supposed to just trust it? What about the patients who got worse? What about the ones who died waiting? Where’s the transparency? This feels like corporate medicine pushing a product… again.
Marie Mee
December 26, 2025 AT 05:17They’re lying about the side effects. I know someone who got neoadjuvant and then the cancer spread during waiting. They said it was rare but it happened. And now they won’t admit it. They just want to sell more drugs. They don’t care about us.
Naomi Lopez
December 26, 2025 AT 14:27It’s amusing how the lay public latches onto terms like ‘pCR’ as if it’s some mystical cure. The truth is, even with a complete response, metastasis can still occur. The real breakthrough isn’t the therapy-it’s the marketing. You can’t sell ‘wait and see’ as a breakthrough. But ‘immunotherapy revolution’? That’s a TED Talk.
Jody Patrick
December 27, 2025 AT 15:56Neoadjuvant only. No extra chemo after. Done. Saved my life.
Radhika M
December 29, 2025 AT 09:07I’m from India and we don’t have access to all this testing. But my doctor told me if tumor is big, do chemo before. If small, do after. Simple. Works. Thank you for explaining why.
Meghan O'Shaughnessy
December 29, 2025 AT 15:24My sister is in a trial for ctDNA monitoring after neoadjuvant. They take blood every 2 weeks. If they see tumor DNA, they hit it again. If not, she’s done. It feels like sci-fi. But it’s real. And it’s saving lives.
Nishant Desae
December 30, 2025 AT 00:10As someone who’s watched a friend go through this, I just want to say: every decision is hard. There’s no perfect path. But what matters is that you’re not alone. Talk to your team. Ask questions. Write things down. Even if you’re scared, even if you’re tired, even if you don’t understand all the words-keep showing up. That’s courage.
Joe Bartlett
December 31, 2025 AT 08:50US doctors push neoadjuvant because they’re paid more. In the UK, we do surgery first. Simpler. Cheaper. Safer. Why copy the American mess?
Jonathan Morris
January 1, 2026 AT 22:15CheckMate 816? That’s funded by Bristol Myers Squibb. The pCR rate is statistically significant but clinically meaningless for 80% of patients. The survival benefit? Marginal. The side effects? Unacceptable. This is a profit-driven illusion masked as progress. ctDNA? A fancy blood test that gives false hope. They’re selling snake oil with peer-reviewed labels.