Protein Calculator for Immune Support
Calculate Your Daily Protein Needs
Based on the article guidelines for immunodeficiency patients (1.2-1.5g protein per kg body weight)
Why Protein Matters
Protein provides amino acids needed to build antibodies and white blood cells. For immunodeficiency patients, optimal protein intake supports immune cell production and repair.
- Recommended range 1.2 - 1.5g per kg body weight
- Example 70kg person: 84-105g/day
Your Results
Recommended protein range
When it comes to staying healthy, Nutrition is the process of obtaining and using food nutrients to support body functions, including immune defense and the Immune System is the network of cells, tissues, and organs that protects you from infections and disease are inseparable. For people with immunodeficiency, every bite can either strengthen or weaken that protection. This guide walks you through the science, the key nutrients, practical meal ideas, and the pitfalls to avoid, so you can turn your plate into a powerful ally.
Quick Takeaways
- Protein, vitamins C & D, zinc, and omega‑3 fats are the top immune‑supporting nutrients.
- Eat a colorful variety of whole foods at least five times a day.
- Stay hydrated; aim for 2‑3 L of water or herbal tea daily.
- Limit processed sugars, excess alcohol, and high‑sodium foods, which can suppress immunity.
- Work with your healthcare team to tailor supplements to your specific deficiency.
Why Nutrition Matters for the Immune System
The immune system relies on a constant supply of building blocks. White blood cells need amino acids from protein to grow and replicate. Micronutrients act as co‑factors for enzymes that launch the body’s defense mechanisms. For example, vitamin C assists in producing collagen, which helps maintain skin barriers-the first line of defense against pathogens. Vitamin D regulates the activity of T‑cells, preventing them from overreacting. When you’re missing these nutrients, the system can’t respond efficiently, making infections more frequent and severe.
Key Nutrients and Their Immune Roles
Below is a snapshot of the most critical nutrients, what they do, and where you can find them. This table is designed for quick reference during grocery trips.
| Nutrient | Primary Immune Role | Top Food Sources |
|---|---|---|
| Protein (amino acids) | Builds antibodies & white blood cells | Lean meat, fish, eggs, legumes, Greek yogurt |
| Vitamin C | Enhances phagocyte function & skin barrier | Citrus fruits, strawberries, bell peppers, broccoli |
| Vitamin D | Modulates T‑cell response & reduces inflammation | Fatty fish, fortified milk, sunlight‑exposed mushrooms |
| Zinc | Supports enzyme activity for immune cell signaling | Oysters, pumpkin seeds, beef, chickpeas |
| Omega‑3 Fatty Acids | Anti‑inflammatory; help regulate cytokine production | Salmon, mackerel, chia seeds, walnuts |
| Probiotics | Maintain healthy gut microbiome, a key immune organ | Yogurt, kefir, sauerkraut, kimchi |
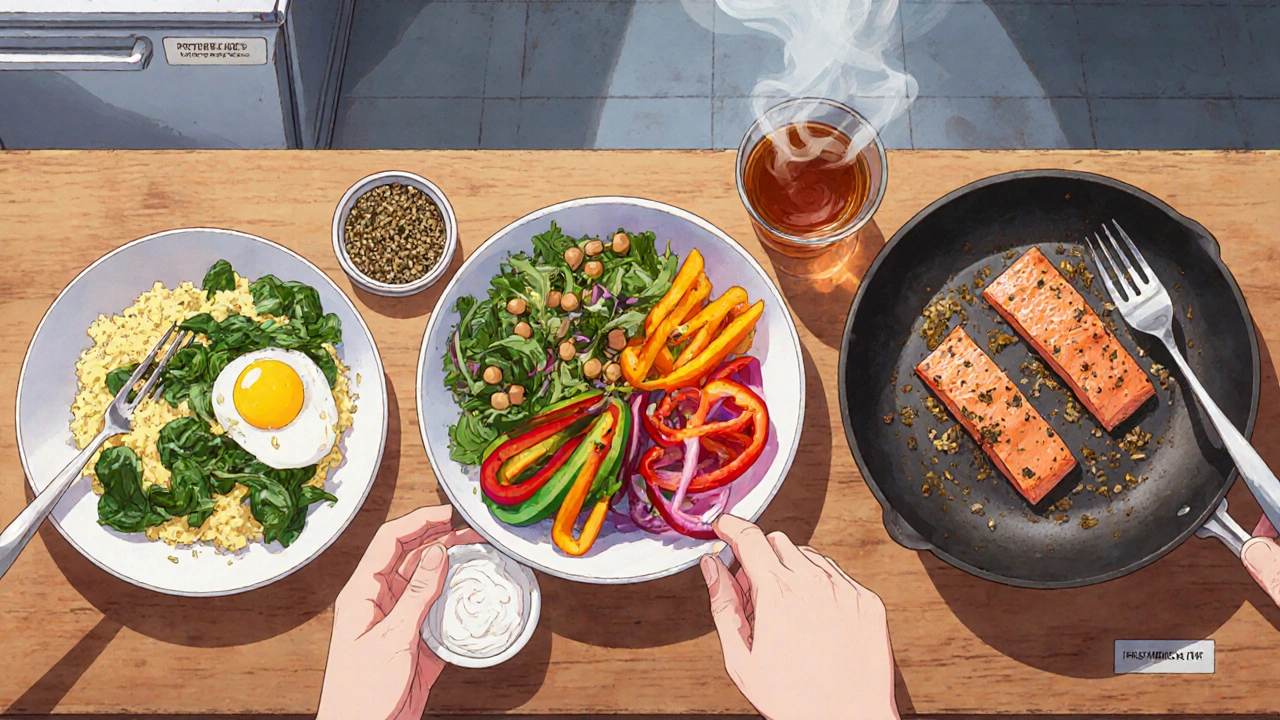
Building an Immune‑Friendly Daily Plate
Think of each meal as a mini‑boost for your defense system. Aim for a balance of macronutrients (protein, carbs, fats) plus a rainbow of micronutrient‑rich foods.
- Start with protein. Include at least 20‑30 g of quality protein at breakfast and dinner. For an easy option, scramble two eggs with spinach and a sprinkling of feta.
- Add a colorful veg side. Fill half the plate with vegetables of differing colors-red tomatoes, orange carrots, green kale-to cover a broad spectrum of vitamins and antioxidants.
- Incorporate healthy fats. Drizzle olive oil over salads or add a handful of nuts to a snack. Omega‑3‑rich fish two to three times a week is ideal.
- Choose whole‑grain carbs. Swap white bread for whole‑grain toast or quinoa; complex carbs sustain energy without spiking blood sugar, which can impair immune function.
- Don’t forget fluids. Aim for 2-3 L of water, herbal tea, or diluted fruit juice. Hydration allows lymph to travel freely, delivering immune cells where they’re needed.
Special Considerations for Immunodeficiency Patients
Immunodeficiency isn’t one‑size‑fits‑all. Some patients have specific nutrient absorption problems, while others need to avoid foods that could trigger infections.
- Monitor calorie needs. Chronic infections raise metabolic demand; you might need 10‑20 % more calories than a healthy adult of the same age.
- Watch for food‑borne pathogens. Choose pasteurized dairy, cooked eggs, and well‑washed produce to reduce the risk of bacterial contamination.
- Consider gut‑health supplements. A probiotic with multiple strains (e.g., Lactobacillus rhamnosus + Bifidobacterium longum) can help maintain a healthy microbiome, especially after antibiotics.
- Tailor vitamin D dosage. Many immunodeficiency patients have low serum levels. A typical maintenance dose ranges from 1,000 IU to 4,000 IU daily, but always verify with your doctor.
- Limit high‑sugar snacks. Sugar can suppress neutrophil activity for up to three hours after consumption. Opt for fruit‑based desserts instead.
One‑Week Sample Meal Plan
Below is a practical, balanced menu that hits all the key nutrients. Adjust portion sizes to meet your personal calorie goal.
| Day | Breakfast | Lunch | Dinner | Snack |
|---|---|---|---|---|
| Mon | Greek yogurt + berries + chia seeds | Quinoa salad with chickpeas, bell peppers, olive oil | Grilled salmon, steamed broccoli, sweet potato | Handful of almonds |
| Tue | Scrambled eggs, spinach, whole‑grain toast | Turkey wrap with avocado, lettuce, tomato | Lentil soup, side of sauerkraut | Apple slices with peanut butter |
| Wed | Oatmeal topped with sliced kiwi and walnuts | Grilled chicken Caesar salad (no croutons) | Stir‑fried tofu, mixed veggies, brown rice | Carrot sticks + hummus |
| Thu | Smoothie (spinach, pineapple, Greek yogurt, flaxseed) | Salmon sushi bowl with edamame and seaweed | Beef stew with carrots and peas | Mixed berries |
| Fri | Whole‑grain pancakes, fresh strawberries | Vegetable minestrone soup, side of whole‑grain roll | Baked cod, quinoa pilaf, sautéed kale | Cottage cheese with peach slices |
| Sat | Egg white omelet with mushrooms, tomato | Chicken gyro on whole‑wheat pita, tzatziki | Pork tenderloin, roasted Brussels sprouts, millet | Greek yogurt with honey |
| Sun | Fruit salad (orange, pomegranate, banana) + pumpkin seeds | Black bean burrito bowl, salsa, guacamole | Shrimp stir‑fry, snap peas, soba noodles | Dark chocolate (70% cacao) square |
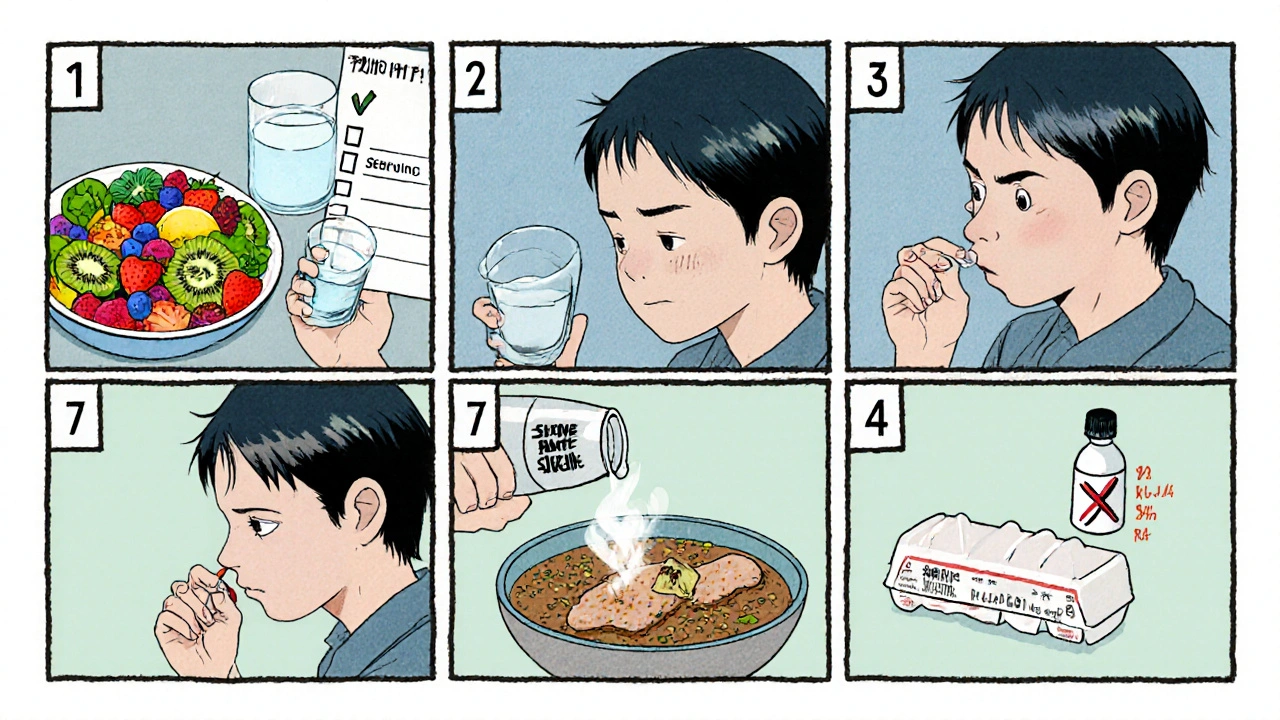
Daily Immune‑Support Checklist
- ✅ Eat at least 5 servings of colorful fruits/vegetables.
- ✅ Include a protein source in every main meal.
- ✅ Take a daily probiotic (check strain count).
- ✅ Get 800-1,000 IU of vitamin D if labs are low.
- ✅ Drink 2-3 L of fluid; limit sugary drinks.
- ✅ Avoid raw or undercooked eggs/meat; choose pasteurized dairy.
Frequently Asked Questions
Can I rely solely on supplements instead of food?
Supplements can fill gaps, but they don’t provide the fiber, phytonutrients, and synergistic effects you get from whole foods. Most experts recommend getting nutrients from a varied diet first, then adding supplements only where deficiencies are proven.
How much protein should an immunodeficiency patient consume?
A good target is 1.2-1.5 g of protein per kilogram of body weight daily. For a 70 kg adult, that’s roughly 84-105 g of protein spread across meals.
Is a low‑carb diet safe for me?
Very low‑carb diets can reduce the intake of fruits and whole grains, which are rich in vitamins C, A, and fiber. Unless prescribed for a specific medical reason, a moderate‑carb, high‑fiber plan is usually better for immune health.
What’s the role of hydration in immunity?
Adequate fluids keep lymph fluid flowing, which transports immune cells throughout the body. Dehydration can thicken mucus, making it easier for pathogens to settle in the respiratory tract.
Should I avoid all dairy because of infection risk?
Only unpasteurized dairy poses a significant risk. Pasteurized milk, cheese, and yogurt are safe and also provide protein, calcium, and probiotics that support immunity.


Alex Lineses
October 18, 2025 AT 17:23Great overview! The guide nails the concept of immunometabolic coupling, where amino‑acid flux fuels leukocyte proliferation and the antioxidant network hinges on vitamin C‑dependent enzymes. For patients with primary immunodeficiency, aligning protein intake with an anabolic window can offset catabolic stress during infections. Incorporating omega‑3‑rich phospholipids further dampens pro‑inflammatory cytokine cascades via resolvin pathways. Don't forget that zinc chelation can impair NF‑κB signaling, so a balanced intake from oysters or pumpkin seeds is crucial. Overall, the synergy between macro‑ and micronutrients creates a robust immunological scaffold.
Brian Van Horne
October 31, 2025 AT 14:12In a nutshell, the protocol is both systematic and adaptable, offering a clear roadmap for clinicians and patients alike. Its emphasis on whole‑food diversity aligns with evidence‑based dietary patterns. The concise bullet points serve as an effective quick‑reference sheet.
Norman Adams
November 13, 2025 AT 12:01Oh sure, swapping soda for kombucha will instantly fix everything.
Margaret pope
November 26, 2025 AT 09:50Lets keep it simple folks nutrition is the foundation for immune health you cant overstate the power of a balanced plate it should include protein colourful veg and healthy fats each meal matters. Staying hydrated is non negotiable it keeps lymph fluid moving and supports cellular function. Small consistent changes add up over time and build resilience.
Karla Johnson
December 9, 2025 AT 07:40The interplay between diet and immune competence is far more intricate than most lay articles suggest. While the guide correctly flags protein, vitamins C and D, zinc, and omega‑3s as cornerstone nutrients, it does not fully explore the mechanistic pathways through which these micronutrients modulate both innate and adaptive immunity. For instance, vitamin D acts as a transcriptional regulator for antimicrobial peptide genes, such as cathelicidin, which directly neutralize bacterial pathogens at mucosal surfaces. Similarly, zinc is a co‑factor for numerous thymic enzymes that shape T‑cell receptor repertoires, and even modest deficiencies can skew the Th1/Th2 balance toward a less effective response. The guide's suggestion to consume 20‑30 g of protein per meal is appropriate, but patients with chronic infections often suffer from protein‑losing enteropathy, necessitating a higher intake-potentially up to 2 g per kilogram of body weight. Moreover, timing matters: distributing protein evenly across the day optimizes muscle protein synthesis and provides a steady supply of amino acids for immunoglobulin production. Regarding omega‑3 fatty acids, the anti‑inflammatory eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) not only dampen cytokine storms but also enhance the resolution phase through specialized pro‑resolving mediators. The inclusion of probiotic strains such as Lactobacillus rhamnosus GG and Bifidobacterium longum is prudent, yet strain‑specific efficacy data indicate that multi‑strain formulations may offer broader colonization and immune modulation. Hydration, as noted, supports lymphatic circulation, but electrolytic balance-especially adequate magnesium and potassium-also underpins cellular immunity by stabilizing membrane potentials of leukocytes. Patients should be cautioned about the hidden sodium in processed foods, which can exacerbate hypertension and indirectly impair microvascular perfusion of immune organs. The recommendation to limit high‑sugar snacks is well‑grounded; hyperglycemia can impair neutrophil chemotaxis and oxidative burst capacity for up to three hours post‑ingestion. In practice, replacing refined sugars with low‑glycemic fruit alternatives not only curtails glucose spikes but also delivers additional phytonutrients that act as antioxidant cofactors. The sample meal plan is a solid template, yet flexibility is key: individuals with gastrointestinal malabsorption may need to substitute dairy‑based calcium sources with fortified plant milks enhanced with bioavailable vitamin D3. Finally, regular monitoring of serum micronutrient levels-especially 25‑hydroxyvitamin D and serum zinc-should guide supplementation, as supra‑physiological dosing can be counterproductive. Collaboration with a registered dietitian familiar with immunodeficiency syndromes ensures that caloric density, nutrient timing, and food safety protocols are meticulously tailored. In sum, a dynamic, evidence‑driven nutrition strategy that adapts to clinical status will materially boost immune resilience in this vulnerable population.
Rohit Sridhar
December 22, 2025 AT 05:29Absolutely spot‑on! Your deep dive really highlights how every bite can tip the balance. For anyone feeling overwhelmed, start small-maybe add a handful of pumpkin seeds to a salad each day and watch the energy shift. Keep tracking how you feel; the body often rewards consistent, thoughtful choices.
Sarah Hanson
January 4, 2026 AT 03:18I completely concur with the recommendations; implementing them will surely enhance patient outcomes, and your articulation of the evidence is both precise and persuasive.
Nhasala Joshi
January 17, 2026 AT 01:07Sure thing, but remember that big pharma deliberately hides the truth about hidden additives in “pasteurized” dairy 🕵️♀️💊 they embed micro‑particles that can sabotage gut flora 😱🚨 stay vigilant and opt for truly raw sources whenever possible 🌱🧪
Matthew Miller
January 29, 2026 AT 22:56Love the energy here – let’s turn those plates into armor! 💪
Liberty Moneybomb
February 11, 2026 AT 20:45Don’t be fooled by the hype – the wellness industry is a cash‑grab machine pushing “immune‑boosting” trends while they secretly stockpile the very toxins they claim to eliminate. Wake up and question every so‑called “superfood” they push on social media.