When you pick up a prescription at the pharmacy, you might not think about who decided whether you get the brand-name drug or the cheaper generic version. But that decision isn’t random. It’s governed by state laws, federal rules, and the legal authority granted to pharmacists - and those rules vary wildly from one state to the next.
What Pharmacists Can and Can’t Do
Pharmacists aren’t just pill counters. In many states, they have the legal right to swap one drug for another - but only under strict conditions. The two main types of substitution are generic substitution and therapeutic substitution.
Generic substitution means replacing a brand-name drug with an FDA-approved generic that has the same active ingredient, strength, and dosage form. This is allowed in all 50 states and D.C. The FDA requires generics to be within 80-125% of the brand’s absorption rate in the body - a range called bioequivalence. As of January 2024, the FDA’s Orange Book lists over 13,700 drug products with confirmed therapeutic equivalence ratings.
Therapeutic substitution is more complex. It means switching to a different drug in the same class - like swapping one blood pressure medication for another, even if they’re chemically different. This is where things get messy. Only 27 states allow pharmacists to do this without a doctor’s direct order. And even in those states, the rules differ. In Colorado, pharmacists must write “Intentional Therapeutic Drug Class Substitution” on the prescription. In California, it’s only allowed for insulin under very specific clinical conditions.
State-by-State Differences Matter
If you move from Texas to Oklahoma, your pharmacist might be able to swap your medication without calling your doctor. In Texas, pharmacists need to contact the prescriber for approval before making therapeutic substitutions - adding 15-20 minutes per prescription. In Oklahoma, they can make the swap with just documentation. That’s not a minor difference. It affects how quickly you get your meds, how much your pharmacy staff is overloaded, and even whether you skip a refill because the process is too slow.
Some states have gone further. Colorado lets pharmacists prescribe birth control, manage tobacco cessation, and administer vaccines under statewide protocols - no individual doctor’s approval needed. Maryland now allows pharmacists to prescribe birth control directly, with Medicaid covering it. New Mexico and Oregon give pharmacists the broadest independent authority in the country, with 87% of pharmacies actively using therapeutic substitution protocols.
But in Alabama? Pharmacists can’t substitute therapeutically unless the doctor explicitly says so on the prescription. That’s not an oversight - it’s the law. And it’s the same in many other states with restrictive scope-of-practice rules.
Federal Moves Change the Game
In July 2022, the FDA made a historic move: it allowed all licensed pharmacists nationwide to prescribe Paxlovid, the antiviral for high-risk COVID-19 patients. This wasn’t just about substitution - it was about pharmacists stepping into a prescribing role, even if temporarily. To do it, pharmacists had to check the patient’s age (12+), weight (over 40kg), test result, and kidney/liver function - using electronic records or direct consultation with a provider. This federal exception bypassed state restrictions, showing that when public health demands it, the system can adapt.
It’s a sign of things to come. More than 19 states are currently pushing legislation to expand pharmacist authority. Virginia and Illinois are likely to pass major reforms by the end of 2024. The American Pharmacists Association sees four big trends emerging: standardizing rules across state lines, expanding authority for mental health meds, linking substitution to value-based care, and creating national competency standards.
Why This Isn’t Just About Saving Money
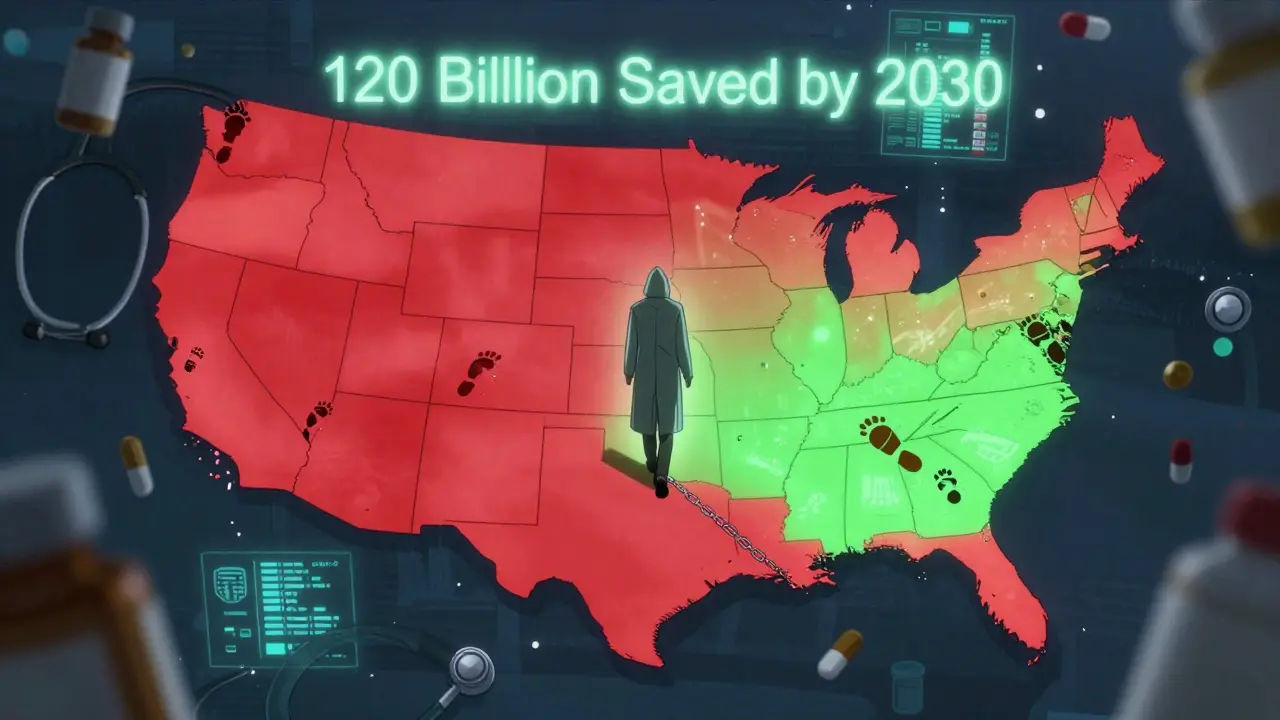
People often think generic substitution is just about cutting costs - and it is. The U.S. healthcare system saves about $253 billion a year just from switching to generics. Over the last decade, that number adds up to $1.97 trillion. But therapeutic substitution? That’s where the real potential lies.
Expanding pharmacists’ ability to switch medications for chronic conditions like hypertension, diabetes, or asthma could save $45-60 billion annually, according to the National Pharmaceutical Association. In rural areas, where doctors are scarce, pharmacist-led substitution has cut medication access gaps by 34% - nearly double the improvement seen in cities.
It’s not just economics. A 2023 survey of 1,247 pharmacists found that 68% in states with strong substitution authority reported better patient outcomes. Patients get meds faster. They’re more likely to stick with their treatment. And pharmacists - who see patients more often than doctors - can catch dangerous interactions or side effects early.
What Gets in the Way
Even where the law allows it, practical barriers block progress. Electronic health records don’t talk to each other. A pharmacist in New York can’t easily see what a patient’s doctor in Florida prescribed. Insurance companies sometimes refuse to cover substituted drugs unless the prescriber reissues the script. And patients? Many don’t understand why their medication changed.
One pharmacy chain reported that 78% of patient complaints were about confusion over substitutions. Another found that 63% of pharmacists struggled with outdated or incompatible pharmacy software. In multi-state chains, pharmacists need up to 40 extra hours of training just to keep up with different state rules.
And then there’s resistance from some doctors. The American Medical Association warns that without full access to medical records, therapeutic substitution could fragment care - especially for patients juggling multiple chronic conditions. They’re not wrong. A diabetic patient on five medications could easily get a drug that interacts badly with another if the pharmacist doesn’t see the full picture.
What Good Practice Looks Like
The best-run pharmacies don’t just follow the law - they build systems around it. Kroger Health reduced substitution-related errors by 37% by creating standardized, cross-state documentation templates and training staff on consistent protocols. Colorado’s statewide model uses a simple, uniform form that takes about five minutes per patient. That’s it. No phone calls. No delays. Just clear, documented decisions.
Successful substitution requires three things: training, documentation, and communication. Pharmacists need ongoing education on therapeutic equivalence, state-specific rules, and how to explain changes to patients. Documentation must be immediate, clear, and stored where other providers can find it. And when possible, pharmacists should notify prescribers - not just because the law says so, but because it keeps care coordinated.
Where This Is Headed
The future of pharmacy isn’t just about filling prescriptions. It’s about managing health. With over 316,000 pharmacists working in the U.S. - most in retail settings - and dispensing 6.34 billion prescriptions a year, they’re already on the front lines. Giving them the legal authority to make therapeutic substitutions isn’t about replacing doctors. It’s about using every trained professional in the system to keep people healthy.
The Congressional Budget Office estimates that smart expansion of pharmacist substitution authority could save $120-150 billion annually by 2030 - while helping 25-30 million Americans who currently can’t get their meds on time. That’s not speculation. It’s data. And it’s happening now, one state at a time.
Can a pharmacist legally substitute my brand-name drug for a generic?
Yes, in all 50 U.S. states and D.C., pharmacists can substitute a brand-name drug with a generic version that the FDA has rated as therapeutically equivalent. Most states require the pharmacist to notify you - either verbally or in writing - before making the switch. The generic must meet FDA bioequivalence standards (80-125% of the brand’s absorption rate).
What’s the difference between generic and therapeutic substitution?
Generic substitution replaces a brand-name drug with an identical generic version - same active ingredient, same dose, same form. Therapeutic substitution swaps one drug for another in the same class - like switching from lisinopril to losartan for high blood pressure. The drugs aren’t identical, but they treat the same condition. Generic substitution is allowed everywhere. Therapeutic substitution is only allowed in 27 states, and even then, with strict rules.
Which states let pharmacists do therapeutic substitution without a doctor’s approval?
As of 2024, 27 states allow pharmacists to perform therapeutic substitution without direct prescriber authorization. These include Colorado, New Mexico, Oregon, Maryland, and California (for insulin only). Each state has its own rules: some require patient consent, others require detailed documentation, and a few limit it to specific drug classes like blood pressure or diabetes meds.
Do I have to give consent for a therapeutic substitution?
It depends on your state. In 17 states, pharmacists must get your written consent - usually a signature on the prescription or a form. Nine states require only verbal consent, and 14 states don’t require any explicit consent but still demand thorough documentation. Even if your state doesn’t require consent, pharmacists should explain the change and answer your questions before swapping your medication.
Why can’t my pharmacist just switch my meds if it’s cheaper?
Because not all drugs in the same class work the same way for everyone. A drug that works for one person might cause side effects or interact badly with another medication you’re taking. Pharmacists are trained to spot these risks, but they can’t make those decisions alone in most states. The law requires them to follow specific protocols - and in many places, they still need a doctor’s okay before changing your prescription.
Can pharmacists prescribe any medication now?
Not broadly - but in some states, yes, for specific conditions. Colorado, New Mexico, Maryland, and Oregon allow pharmacists to prescribe birth control. Some states let them prescribe nicotine replacement therapy or emergency contraception. The 2022 federal authorization for Paxlovid was a major exception - it let all pharmacists prescribe one specific drug for a limited time. But pharmacists still can’t prescribe antibiotics, opioids, or most chronic disease meds without a collaborative agreement or state protocol.


Anjula Jyala
January 27, 2026 AT 10:10Generic substitution is baseline. Therapeutic substitution is where the real clinical judgment kicks in. FDA bioequivalence is a statistical mirage-80-125% range means a drug can be 25% weaker or 25% stronger and still be ‘equivalent.’ That’s not medicine, that’s actuarial math. And pharmacists aren’t trained to interpret pharmacokinetic variability across polypharmacy patients. You’re trading convenience for risk. And no, I don’t care if it saves $45B. Lives aren’t line items.
Kirstin Santiago
January 29, 2026 AT 06:38Really appreciate this breakdown. I’ve seen firsthand how confusing substitutions can be for elderly patients. One of my neighbors got switched from metformin to glipizide and had a hypoglycemic episode because she didn’t realize the mechanism changed. Documentation and clear communication matter more than the law allows. Simple things like a printed handout or a quick call to the pharmacy help so much.
Kathy McDaniel
January 31, 2026 AT 00:11so like… i just got my blood pressure med switched last week and thought my pharmacy messed up? turns out its legal?? lol i had no idea. glad theyre trying to save money but also kinda scared i got the wrong stuff. hope my doc knows
Patrick Merrell
February 1, 2026 AT 04:56Let’s be real-pharmacists aren’t doctors. They’re not trained to manage complex chronic disease interactions. This ‘expansion of authority’ is a corporate cost-cutting scheme dressed up as healthcare innovation. The AMA isn’t being obstructive. They’re being responsible. You don’t hand a wrench to someone who’s never fixed a car and call it ‘progress.’
Conor Flannelly
February 1, 2026 AT 10:06There’s a philosophical tension here: autonomy vs. safety. Pharmacists are the most accessible healthcare professionals-yet we restrict them from acting on their knowledge. If we trust them to dispense opioids, why not antihypertensives? The system isn’t designed for efficiency-it’s designed for liability. But liability shouldn’t override access, especially in rural communities where the nearest PCP is 90 minutes away.
Conor Murphy
February 1, 2026 AT 12:53I work in a pharmacy in rural Maine. We do therapeutic substitutions all the time. We call the doctor’s office, document everything, and explain it to the patient. It’s not hard. What’s hard is when insurance denies the new med and the patient walks out empty-handed. We’re not trying to replace doctors-we’re trying to keep people alive between visits.
Desaundrea Morton-Pusey
February 2, 2026 AT 11:26Oh great, now pharmacists are gonna be prescribing birth control AND switching my diabetes meds? Next they’ll be doing my colonoscopies. This is why America’s healthcare is a joke. Let the doctors do their job and stop turning pharmacies into mini-clinics. I don’t need a pharmacist telling me what my body needs. I need a real MD.
Kegan Powell
February 2, 2026 AT 16:58It’s not about replacing doctors, it’s about using every tool we’ve got. Pharmacists are the most consistent point of contact for chronic disease patients. If they can catch a dangerous interaction before it happens, why not let them? The data shows better adherence, fewer ER visits, lower costs. This isn’t radical-it’s just smart. We’ve been underutilizing pharmacists for decades. Time to catch up.
April Williams
February 3, 2026 AT 17:46My mom died because her pharmacist swapped her anticoagulant without telling her doctor. She had atrial fibrillation. The new med didn’t show up in the system. They didn’t even call. Now you want to give pharmacists even more power? That’s not progress, that’s negligence with a badge.
Harry Henderson
February 4, 2026 AT 13:49STOP WHINING. We have 316,000 trained pharmacists sitting idle while doctors are overworked and patients are dying because they can’t get meds. If you’re too scared to let them help, you’re part of the problem. This isn’t a debate-it’s a moral imperative. Let pharmacists do their job or get out of the way.
suhail ahmed
February 5, 2026 AT 20:18In India, we’ve had community pharmacists managing hypertension and diabetes for years-no doctor needed, just training and protocols. It works. People trust their local pharmacist more than distant specialists. Why does America act like this is some radical idea? We’re not talking about brain surgery-we’re talking about filling gaps in a broken system. Let’s stop reinventing the wheel and start building on what works.
Candice Hartley
February 7, 2026 AT 15:51My pharmacist switched my asthma med last month. She wrote a note, called my doctor, and gave me a one-pager. I felt safe. No drama. Just good care.