When your prescription costs $500 a month and your insurance only covers $50, you’re left with a choice: skip doses, split pills, or go without. For millions of Americans, this isn’t hypothetical-it’s daily reality. That’s where prescription assistance programs come in. These aren’t charity drives or nonprofit initiatives. They’re direct support systems run by pharmaceutical companies like Pfizer, Merck, and Eli Lilly to help patients afford the drugs they need. And they’re bigger than most people realize.
Two Types of Help: Copay Cards vs. Patient Assistance Programs
There are two main ways drug makers help patients pay for meds: copay assistance programs and Patient Assistance Programs (PAPs). They sound similar, but they’re built for completely different people.Copay assistance programs are for people who have insurance but still can’t afford their out-of-pocket costs. Think of them as coupons you use at the pharmacy. When you present a copay card, the drug company pays the difference between what your insurance covers and what the drug actually costs. For a specialty drug like Humira or Dupixent, that could mean saving $200-$500 per month. These cards are easy to get-usually just a quick online form-and they’re accepted at most pharmacies. But there’s a catch: many health plans now use copay accumulators, which means the manufacturer’s payment doesn’t count toward your deductible or out-of-pocket maximum. So you might pay less each month, but it takes longer to reach catastrophic coverage.
Patient Assistance Programs (PAPs) are for people without insurance or with very limited coverage. These programs give you the medication for free-or for a tiny fee like $10-$15 per prescription-if you meet income guidelines. Most PAPs require your household income to be under 400% of the Federal Poverty Level. For a family of four in 2025, that’s about $60,000 a year. You’ll need to provide proof of income, a doctor’s letter confirming medical need, and proof of U.S. residency. The application can take 45-60 minutes. Once approved, you might get a 90-day supply mailed directly to your home.
Who Gets Help-and Who Doesn’t
Not everyone qualifies. And the rules change depending on what kind of insurance you have-or don’t have.If you’re on Medicare Part D, copay cards can help reduce your monthly cost. But here’s the problem: that help doesn’t count toward your True Out-of-Pocket (TrOOP) costs. That means you stay stuck in the coverage gap longer. PAPs can’t be used at all if you’re on Medicare Part D or Medicaid in most cases. The government doesn’t allow it-because it could inflate drug prices and create loopholes.
Even worse, 78% of state Medicaid programs ban copay assistance entirely. They see it as a trick that pushes patients toward expensive brand-name drugs instead of cheaper generics. In states like California and New York, manufacturers are now required to report how much they spend on these programs. Some states even limit how much a card can cover per year.
And if you’re uninsured? You might qualify for a PAP-but only if you don’t have any other drug coverage. That includes VA benefits, TRICARE, or even a spouse’s plan. Many PAPs require you to swear you have no other prescription coverage. That’s a problem for people who have partial coverage or are caught in the gaps between jobs.
How Much Help Is Actually Out There?
The numbers are staggering. In 2022 alone, pharmaceutical companies gave $24.5 billion in direct assistance to patients. That’s enough to cover nearly 12.7 million people. And it’s growing. By 2027, that number could hit $38 billion.Eighty-five percent of specialty drugs now come with some kind of manufacturer copay card. That includes treatments for cancer, rheumatoid arthritis, multiple sclerosis, and severe asthma. For example, Teva’s Cares program gives certain generic medications at no cost. The Asthma and Allergy Foundation of America reports that eligible patients can pay as little as $15 per prescription for Dulera, with savings up to $90 per fill.
But here’s the hidden cost: these programs may be making drug prices worse. A 2022 study in JAMA Internal Medicine found that copay assistance encourages patients to choose brand-name drugs even when generics are available. That pushed total drug spending up by $1.4 billion in one year. Critics argue these programs don’t fix the broken pricing system-they just make it more comfortable for patients to keep paying inflated prices.
How to Find and Apply for Help
You don’t have to figure this out alone. The Medicine Assistance Tool (MAT), run by PhRMA, lets you search over 900 programs by drug name, income, and insurance status. It’s free, confidential, and works on mobile.For copay cards:
- Go to the drug manufacturer’s website (search for “[Drug Name] + patient assistance”)
- Fill out a quick form-usually just name, insurance, and doctor info
- Print or download the card
- Present it at the pharmacy when you pick up your prescription
For PAPs:
- Use MAT to find programs for your drug
- Download the application
- Gather documents: last two pay stubs or tax return, proof of address, doctor’s note
- Mail or submit online
- Wait 2-4 weeks for approval
Many patients give up after the first application. But persistence pays. One woman in Ohio applied to five different PAPs for her son’s rare disease medication. Three denied her. The fourth approved her-and now she gets the drug free every three months.
What You Need to Know Before You Apply
- Not all programs work with all pharmacies. Some only ship to your home. Others only work with CVS, Walgreens, or specific chains. - Renewals are common. Most PAPs require you to reapply every 6-12 months. Set a calendar reminder. - Doctors can help. Many clinics have patient navigators who handle applications for you. Ask. - Don’t assume you’re ineligible. Even if you have a job, you might still qualify. Income limits are higher than you think. - Watch for scams. Legitimate programs never ask for credit card info upfront. If someone calls asking for payment to “process” your application, hang up.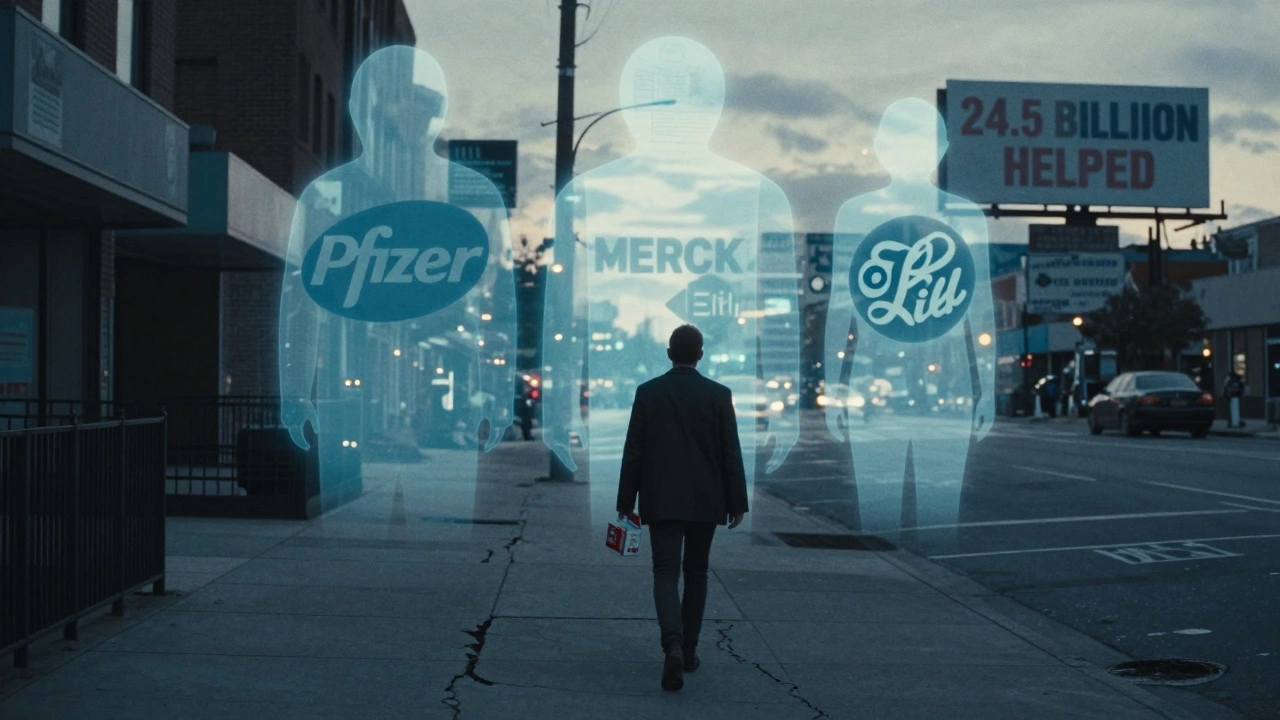
The Bigger Picture
These programs are lifesavers-but they’re also a symptom of a broken system. The fact that 28 million Americans are still uninsured, and millions more can’t afford their meds despite having insurance, shows that manufacturer assistance isn’t a solution. It’s a Band-Aid.Pharmaceutical companies say they’re doing their part. And in many cases, they are. But without real price controls, these programs will keep growing. The Congressional Budget Office predicts that by 2028, over 15 million Americans will rely on manufacturer help just to get their prescriptions. That’s more than the population of Florida.
For now, if you’re struggling to pay for your meds, don’t wait. Start with the Medicine Assistance Tool. Talk to your pharmacist. Ask your doctor. You’re not alone-and help is out there.
Can I use a copay card if I’m on Medicare?
Yes, you can use a copay card while on Medicare Part D to lower your monthly cost. But the manufacturer’s payment won’t count toward your out-of-pocket maximum. That means you’ll stay in the coverage gap longer. PAPs, however, are not available to Medicare beneficiaries.
Do I need to be poor to qualify for a Patient Assistance Program?
No. Most PAPs accept households earning up to 400% of the Federal Poverty Level. For a family of four in 2025, that’s about $60,000 a year. Many middle-income families qualify, especially if they’re paying high premiums or have multiple prescriptions.
Can I use copay assistance with Medicaid?
Almost never. In 78% of states, Medicaid prohibits the use of manufacturer copay cards. The program views them as encouraging higher drug prices. If you’re on Medicaid, your best option is to ask your doctor about generic alternatives or apply for a PAP if your drug isn’t covered.
Are there any free tools to find these programs?
Yes. The Medicine Assistance Tool (MAT), run by PhRMA, is free, confidential, and searchable by drug name, income, and insurance status. It lists over 900 programs from drug makers, nonprofits, and government sources. No sign-up required.
What if my application gets denied?
Don’t stop. Many patients get denied the first time due to missing documents or income miscalculations. Call the program directly-some have counselors who can help you reapply. You can also try applying to multiple programs for the same drug. One patient applied to seven PAPs for her insulin and got approved by two.
Can I use these programs for generic drugs?
Rarely. Most copay cards and PAPs are only available for brand-name drugs. But some manufacturers, like Teva and Mylan, offer PAPs for select generics. Check the Medicine Assistance Tool or call the drug maker directly. Some nonprofit organizations also help with generic medication costs.
Next Steps
If you’re paying more than $50 a month out of pocket for a prescription, take 10 minutes today and search the Medicine Assistance Tool. Even if you think you don’t qualify, it’s worth checking. Many people find help they didn’t know existed.Ask your pharmacist: "Does this drug have a manufacturer copay card?" They often have the cards on hand. Talk to your doctor: "Are there patient assistance programs for this medication?" They can write the letter you need.
Don’t let confusion or shame stop you. These programs exist because people need them. You’re not asking for a handout-you’re using a tool designed to make healthcare work.


James Kerr
December 1, 2025 AT 23:59This is actually super helpful, thanks for laying it out so clearly. I didn’t realize copay cards don’t count toward your deductible-that’s wild. I’ve been using one for my asthma inhaler and thought I was getting closer to hitting my out-of-pocket max. Nope. Just paying less each month while staying stuck. 😅
Cindy Lopez
December 2, 2025 AT 14:22Pharmaceutical companies giving $24.5 billion in assistance? That’s not charity-it’s PR. They inflate prices, then offer coupons to make you feel better about paying them. It’s a brilliant, cynical business model. And yes, I’m grammatically precise about this.
Katherine Gianelli
December 4, 2025 AT 13:58I’ve been there-paying $400 for insulin while working full-time, making $55k. People think you’re poor if you need help, but no, you’re just stuck in the gap. My nurse helped me apply to a PAP and now I get it free every 90 days. You’re not broken. The system is. Keep going. You’ve got this 💛
Archie singh
December 5, 2025 AT 07:22Stop pretending these programs are noble. They’re designed to keep brand-name drugs dominant. The JAMA study says it all-$1.4 billion extra spent because patients were manipulated into choosing expensive options. This isn’t help. It’s market distortion dressed as compassion. And yes, I’m being aggressively precise.
Albert Essel
December 7, 2025 AT 04:35There’s truth on both sides. The programs are a Band-Aid, but for someone choosing between food and medicine, that Band-Aid matters. I’ve seen patients cry when they get approved for a PAP. That’s real. The system is broken, yes-but we can’t wait for policy fixes while people suffer now. Let’s use the tools we have while pushing for change.
Rashi Taliyan
December 7, 2025 AT 07:44In India, we pay out of pocket for everything-no insurance, no cards, no safety nets. I cried reading this because I didn’t know people in the US had these options. It’s not perfect, but it’s something. I’m so grateful someone shared this. Thank you. 🙏
Rashmin Patel
December 7, 2025 AT 21:04Just want to add-many people don’t know that some PAPs will accept proof of unemployment benefits or even a letter from a social worker if you’re between jobs. I helped my neighbor apply for her diabetes meds after she lost her job, and we used her unemployment letter + her doctor’s note. Took 3 weeks but it worked. Also, if you’re on Medicaid in Texas or Florida, you can still apply for PAPs even if copay cards are banned. Just don’t give up. And yes, I’ve applied to 11 programs for my mom’s meds. Four approved. That’s a win. 🌟
Kara Bysterbusch
December 9, 2025 AT 03:08As someone who works in global health policy, I find this both profoundly moving and deeply troubling. The fact that a private sector-driven, patchwork system of charitable assistance has become the primary mechanism for ensuring medication access in the United States is not a triumph-it is a systemic failure of unprecedented scale. The data presented here, while statistically compelling, obscures a moral imperative: healthcare is a human right, not a product subject to corporate discretion. The Medicine Assistance Tool is a valuable resource, but it should not be necessary. We must demand structural reform-price transparency, universal coverage, and the elimination of profit-driven barriers to essential medicines. Until then, we continue to bandage a hemorrhage with glitter.