Introduction to Pupil Constriction and Myosis
As a blogger, I often find myself researching and writing about various topics, and I recently stumbled upon an interesting subject: pupil constriction, also known as myosis. This physiological process caught my attention, and I thought it would be a great idea to share and discuss the possible causes of myosis. So, in this article, I will explore the factors that contribute to the constriction of the pupils and provide you with a better understanding of this fascinating occurrence.
Understanding the Pupil and Its Functions
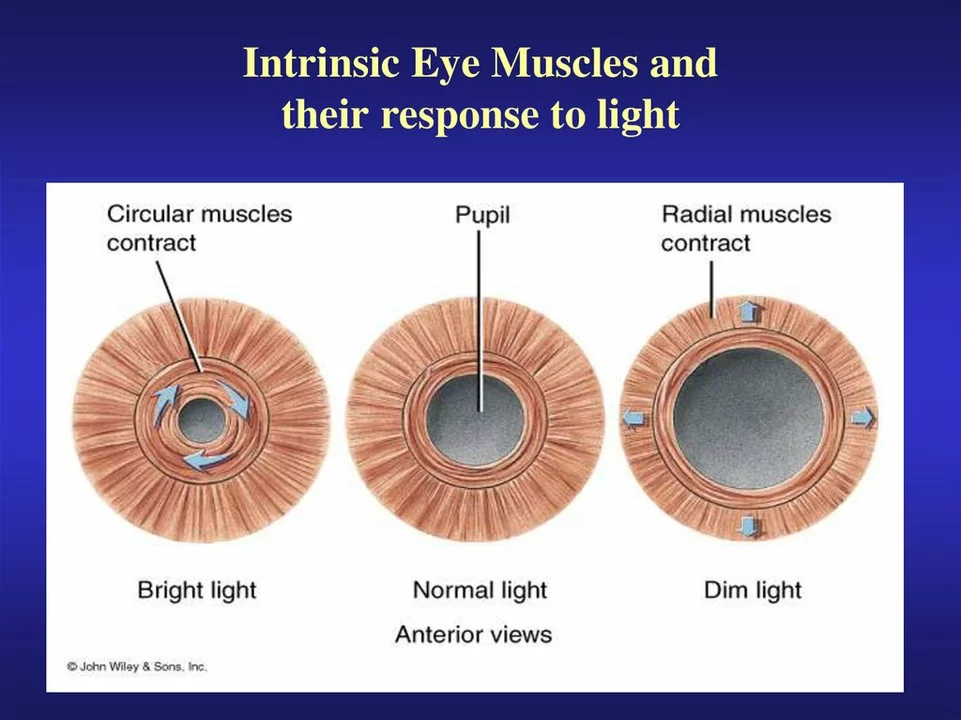
Before delving into the causes of myosis, let's first understand the basic function of the pupil and its importance. The pupil is the circular opening in the center of the iris, responsible for controlling the amount of light that enters the eye. Its primary function is to aid with vision by regulating the light that reaches the retina. When the surrounding environment is bright, the pupil constricts, reducing the amount of light entering the eye. Conversely, when the environment is dark, the pupil dilates, allowing more light to enter and improve vision.
Myosis: The Constriction of the Pupil
Myosis refers to the constriction or narrowing of the pupil, which can occur for various reasons. This natural process helps protect the retina from excessive light exposure and ensures clear vision. However, it's essential to understand the factors that can cause myosis, as some indicate underlying health issues that may require medical attention.
Light Exposure and Pupil Constriction
One of the most common causes of myosis is exposure to bright light. When the eye encounters a bright light source, the pupil constricts to reduce the amount of light entering the eye and prevent damage to the retina. This process, known as the pupillary light reflex, is an essential mechanism that helps protect our eyes and maintain clear vision.
Drugs and Medications Affecting Pupil Size
Certain drugs and medications can also cause myosis. Opioids, for example, are known to induce pupil constriction. This side effect is commonly observed in individuals who are taking prescription pain medications or using illicit substances such as heroin. Additionally, some eye drops used to treat conditions like glaucoma can also cause myosis as they work to reduce intraocular pressure.
Neurological Conditions and Pupil Constriction
Some neurological conditions can also lead to myosis. For instance, Horner's syndrome, a rare disorder affecting the sympathetic nervous system, can cause one pupil to be constricted while the other remains unaffected. This condition may result from an injury, tumor, or stroke affecting the sympathetic nerve pathway. If you notice an unexplained difference in pupil size, it's essential to seek medical attention for a proper diagnosis.
Head Injuries and Pupil Constriction
Head injuries can also cause myosis, as trauma to the brain can affect the nerves responsible for controlling pupil size. In some cases, a constricted pupil may indicate increased pressure within the skull, which can be life-threatening if not treated promptly. Therefore, it's crucial to seek immediate medical attention if you or someone you know experiences a head injury accompanied by changes in pupil size.
Aging and Pupil Size
As we age, it's common for our pupils to become smaller and less responsive to changes in light. This natural process, known as senile myosis, can make it more difficult for older individuals to adjust to different lighting conditions. While this change is considered a normal part of aging, it's essential to be aware of the impact it can have on vision and take necessary precautions, such as ensuring adequate lighting in the home.
Eye Conditions Affecting Pupil Constriction
Some eye conditions can also cause myosis. For example, uveitis, an inflammation of the middle layer of the eye, can lead to pupil constriction and light sensitivity. Additionally, conditions like iritis and anterior uveitis can cause the iris to stick to the lens, resulting in a constricted pupil. If you're experiencing unexplained myosis along with eye pain or vision changes, it's essential to consult an eye care professional for a proper evaluation.
Conclusion
Understanding the causes of myosis is essential for maintaining good eye health and identifying potential underlying health issues. From exposure to bright light and certain medications to neurological conditions and aging, many factors can contribute to pupil constriction. If you notice any unexplained changes in your pupil size, it's crucial to seek the advice of a healthcare professional to determine the cause and receive appropriate treatment if necessary.

Suzy Stewart
May 16, 2023 AT 13:35Great overview! 🎉 Your breakdown of the light reflex and drug effects is spot‑on. Keep it up! 😊
Traven West
May 19, 2023 AT 11:01Your article *reads* fine, but you *should* use “pupil” instead of “pupils” when talking about a single eye. Also, ditch the extra “the” – it drags the flow.
Jonny Arruda
May 22, 2023 AT 08:28I appreciate the clear way you listed the causes. It’s helpful for anyone who just noticed a weirdly small pupil.
Melissa Young
May 25, 2023 AT 05:55Honestly, this stuff is basic anatomy for anyone with a decent education. If you’re in the US, you’ve already covered this in high‑school biology, so stop over‑complicating it.
SHASHIKANT YADAV
May 28, 2023 AT 03:21Exactly, Suzy! 🤓 Adding to that, prolonged exposure to LED screens can also trigger mild myosis due to the blue‑light component, especially if you don’t use proper filters.
Ryan Pitt
May 31, 2023 AT 00:48Good catch, Traven. Also, it’s worth noting that the pupil’s response is mediated by the parasympathetic fibers of the oculomotor nerve – a quick reminder for readers.
Jami Johnson
June 2, 2023 AT 22:15The physiology of the pupil is a marvelous symphony orchestrated by the autonomic nervous system.
When photons flood the retina, photoreceptors send signals via the optic nerve to the pretectal nucleus, which then projects bilaterally to the Edinger‑Westphal nuclei.
From there, cholinergic fibers travel along the oculomotor nerve to innervate the sphincter pupillae, causing constriction.
This cascade is what we observe as the pupillary light reflex, a protective mechanism that has evolved over millennia.
However, the simplicity of the description belies the complexity of the underlying circuitry, which can be disrupted by a myriad of pathological states.
For instance, lesions in the sympathetic pathway result in Horner’s syndrome, manifesting not only as miosis but also as ptosis and anhidrosis.
Conversely, opiate intoxication produces a classic pinpoint pupil due to enhanced parasympathetic tone.
Glaucoma medications, particularly miotics like pilocarpine, pharmacologically mimic this effect by directly stimulating muscarinic receptors.
Age‑related changes introduce senile miosis, where the iris stroma loses elasticity, reducing dynamic range.
Moreover, chronic exposure to high‑intensity light can induce adaptive constriction, a protective adaptation against phototoxic damage.
It is crucial for clinicians to differentiate between physiological and pathological miosis, as the therapeutic approaches differ dramatically.
A thorough history encompassing drug use, recent head trauma, and systemic illnesses often provides the first clues.
Neuro‑imaging may be warranted when asymmetry persists, especially to rule out a compressive mass along the sympathetic chain.
Ophthalmic examination, including the use of apraclonidine drops, can help unmask subtle Horner’s syndrome.
In practice, the interdisciplinary collaboration between neurologists, ophthalmologists, and emergency physicians ensures timely diagnosis.
Ultimately, understanding the cascade empowers both patients and providers to respond appropriately to this deceptively simple yet clinically significant sign.
Kasey Krug
June 5, 2023 AT 19:41While your poetic description is entertaining, the average reader just wants the bottom line: pinpoint pupils = opioid use or CNS depression, not a deep dive into embryology.
jake cole
June 8, 2023 AT 17:08Spare us the condescension, Kasey. Anyone who reads your comment probably already knows the basics and is looking for nuanced info, which you clearly lack.
Natalie Goldswain
June 11, 2023 AT 14:35Interesting read, thanks for sharing.
khajohnsak Mankit
June 14, 2023 AT 12:01Indeed, the interplay of photons dancing across the retina is like a kaleidoscope of cosmic whispers, each photon a tiny messenger guiding our sight.
Jayant Paliwal
June 17, 2023 AT 09:28When considering myosis, one must first acknowledge the fundamental phototransduction cascade; this cascade, beginning with photon absorption, triggers a series of biochemical events, culminating in the contraction of the sphincter pupillae. Additionally, systemic factors such as autonomic tone, circadian rhythms, and even emotional states-fear, excitement-modulate pupil size, thereby introducing variability that challenges simplistic explanations. Pharmacologically, agents like pilocarpine, which act as muscarinic agonists, directly stimulate constriction, whereas opioids elevate parasympathetic output, producing a characteristic pinpoint appearance. Neurologically, lesions affecting the sympathetic pathway-be they due to carotid dissection, tumor infiltration, or spinal cord injury-manifest as Horner’s syndrome, a constellation that includes miosis, ptosis, and anhidrosis. Age‑related senile changes shrink the iris aperture, reducing responsiveness, a phenomenon observable in geriatric populations. Moreover, environmental illumination-particularly high‑intensity blue light from modern displays-can induce adaptive miosis, underscoring the importance of proper lighting ergonomics. Clinically, discerning physiological from pathological miosis necessitates a thorough history, precise slit‑lamp examination, and often pharmacologic testing with agents like apraclonidine. In sum, the multifactorial nature of pupil constriction demands a holistic approach, integrating anatomy, physiology, pharmacology, and environmental considerations.
Kamal ALGhafri
June 20, 2023 AT 06:55While your exhaustive enumeration is thorough, the crux remains that any persistent unilateral miosis warrants urgent neuro‑ophthalmic evaluation to exclude life‑threatening pathology.
Gulam Ahmed Khan
June 23, 2023 AT 04:21Nice job breaking it down! 👍 Keep the science coming!
John and Maria Cristina Varano
June 26, 2023 AT 01:48yeah great stuff but u should add more about the drug side effects its kinda missing
Melissa Trebouhansingh
June 28, 2023 AT 13:35In reflecting upon your observation, one must consider that the omission of pharmacological nuance may inadvertently diminish the educational value of the piece; however, the author’s primary intent appears to be an overview rather than an exhaustive pharmacopoeia, and thus the balance struck aligns with the constraints of a general‑audience blog format, which, while perhaps disappointing to a specialist reader such as yourself, still fulfills the broader goal of public outreach