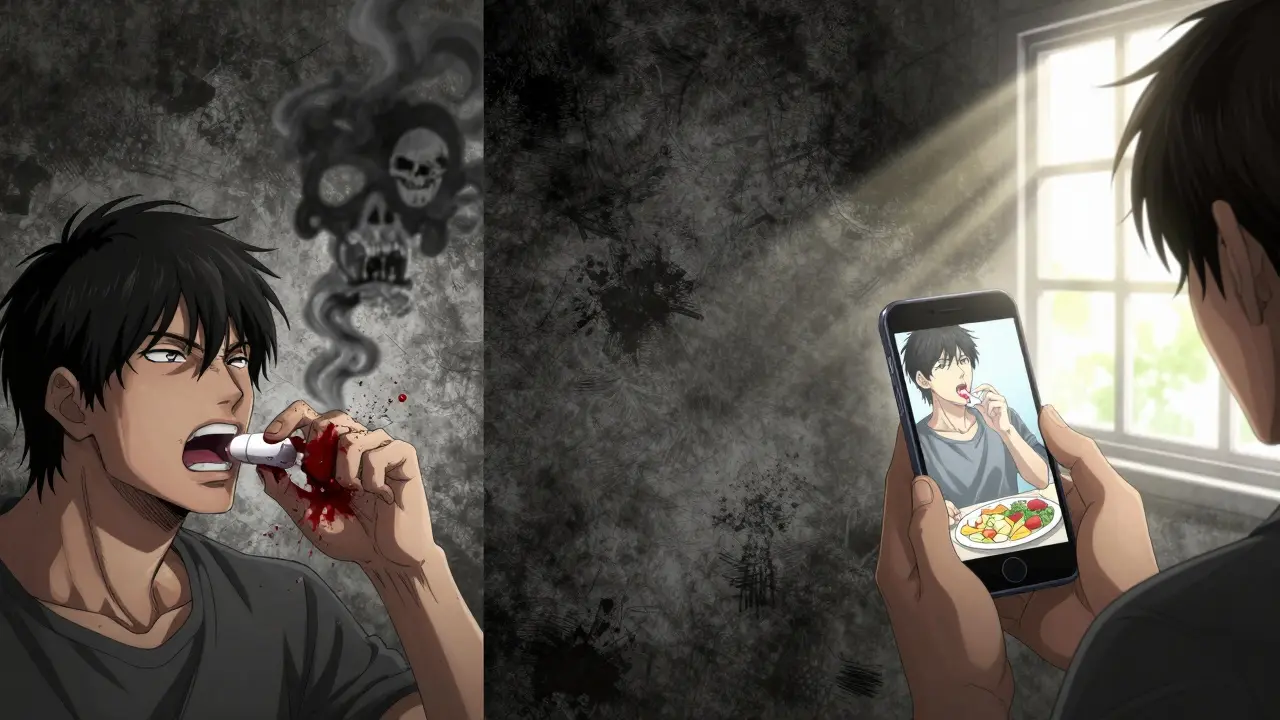
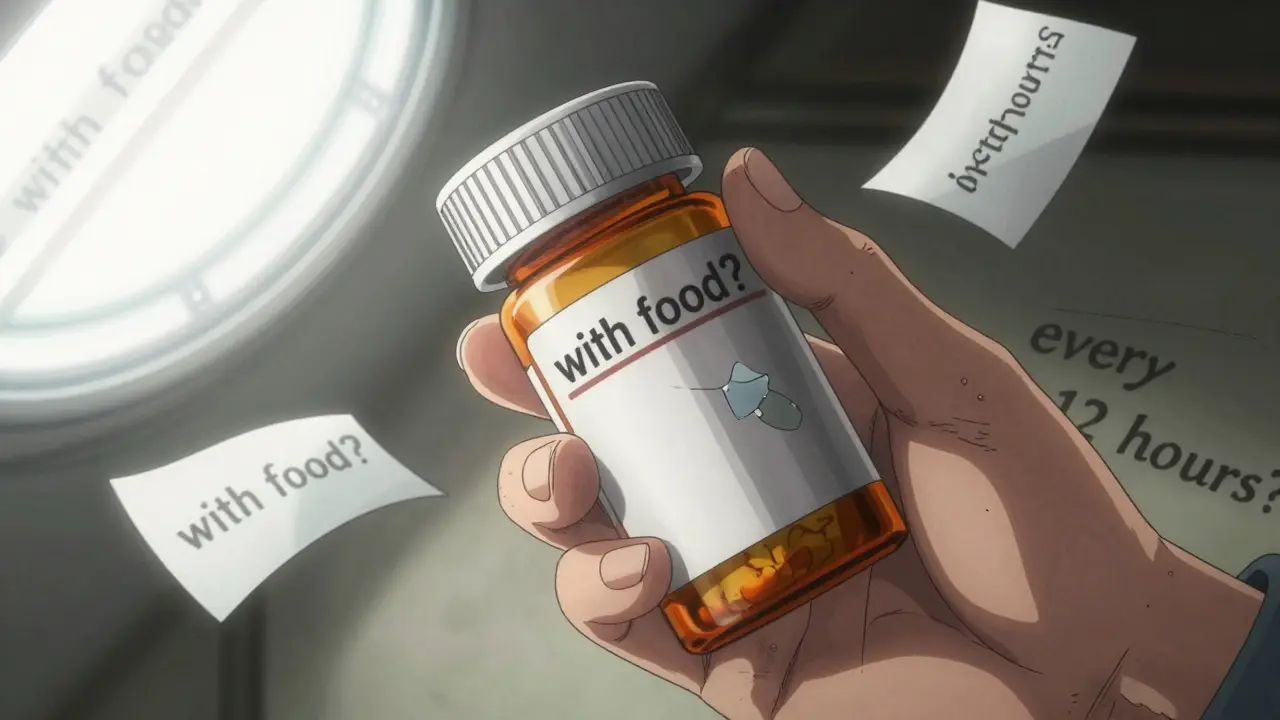
Have you ever looked at your prescription bottle and wondered what "take with food" really means? Or maybe you’ve skipped a dose because you weren’t sure if "every 12 hours" meant 8 a.m. and 8 p.m. - or 12 a.m. and 12 p.m.? You’re not alone. Nearly half of all patients misinterpret the special instructions on their prescription labels. And those small misunderstandings can lead to big problems: hospital visits, dangerous side effects, or meds that just don’t work.
What Are Special Instructions, Anyway?
Special instructions on prescription labels aren’t just extra text. They’re life-saving details that tell you how to take your medicine - not just when or how much. While basic dosage says "take one tablet daily," special instructions say things like:- Take on an empty stomach
- Shake well before use
- Refrigerate
- Avoid sunlight
- Do not crush
- Take with a full meal
- Discard after 14 days
Where Do These Instructions Hide?
You might think all the info is right on the bottle. But it’s not that simple. According to the Cleveland Clinic, special instructions show up in three places:- On the main label (32% of cases)
- On a small sticker stuck to the bottle (47% of cases)
- In a separate paper insert (21% of cases)
Why Do People Keep Getting It Wrong?
It’s not just about reading. It’s about understanding. Take "take with food." Sounds simple, right? But a Harvard Health study found people interpret it three different ways:- 41% think it means "with the first bite of food"
- 33% believe it means "during the meal"
- 26% understand it as "within 30 minutes of eating"
What’s Being Done to Fix This?
The FDA knows this is a problem. In 2014, they updated labeling rules to require:- Minimum 10-point font size
- At least 70% contrast between text and background
- Clear, plain language - no medical jargon
What You Can Do Right Now
You don’t have to wait for better labels. Here’s how to protect yourself:- Check all three places - the bottle, the sticker, and the paper insert. Don’t assume everything’s on the front.
- Ask your pharmacist - not just "What’s this for?" but "What does ‘take with food’ mean here?" Ask them to explain timing, food rules, and storage.
- Write it down - copy the instructions in your own words. If it says "take on empty stomach," write: "No food or drink (except water) for 1 hour before and 2 hours after."
- Use tools - pill organizers with time slots cut timing errors by 47%. Medication reminder apps help 62% of users stick to their schedule.
- Request large print - 94% of U.S. pharmacies offer it for free. If the text is too small, ask for it.
When to Call Your Doctor or Pharmacist
Don’t guess. If any of these sound familiar, call right away:- You’re not sure if "with food" means a snack or a full meal
- You missed a dose and aren’t sure if you should take it late
- The instructions say "avoid sunlight" but you’re not sure what that means - do you stay indoors? Wear sunscreen?
- You see a symbol you don’t understand (like a sun with a line through it)
- The label says "discard after 14 days" but you still have pills left
The Bigger Picture
Misunderstanding medication instructions isn’t just a personal problem. It’s a national crisis. The U.S. spends $42 billion a year on preventable medication errors. A 2023 Medicare report found 43% of patient complaints about prescriptions were about confusing instructions - costing $1.2 billion in avoidable hospital stays. But there’s hope. Studies show clear special instructions reduce errors by 38%. Standardized language could cut emergency visits for seniors by 19%. And if we get this right - really right - experts estimate we could save $18.7 billion a year by 2030. It’s not about perfect labels. It’s about clear communication. And that starts with you asking questions, checking all the details, and never assuming you know what a phrase means.What does 'take with food' really mean on a prescription label?
It doesn’t mean just eating something. For most medications, it means taking the drug with a full meal - not a snack, not a glass of milk, and not right after brushing your teeth. A full meal usually means at least 300 calories and includes protein, fat, and carbs. If you’re unsure, ask your pharmacist what counts as a "full meal" for your specific drug.
Why do some pills say 'do not crush'?
Crushing can destroy how the medicine works. Some pills are designed to release slowly over time. Crush them, and you get the full dose all at once - which can be dangerous or even deadly. Others have coatings that protect your stomach or prevent bad tastes. Crushing ruins those features. Always swallow whole unless your doctor or pharmacist says it’s safe to crush.
What if my prescription says 'take on an empty stomach' but I feel sick?
If you feel nauseous or dizzy when taking a drug on an empty stomach, don’t just stop. Call your pharmacist. Some medications can be taken with a small amount of bland food - like dry toast or plain crackers - without affecting absorption. Others absolutely cannot. Never assume. Always ask for clarification before changing how you take it.
Are special instructions different for generics vs. brand-name drugs?
The active ingredient is the same, so the core instructions should be too. But sometimes the inactive ingredients (fillers, coatings, time-release materials) differ. That can change whether you need to take it with food, avoid sunlight, or store it in the fridge. Always read the label that came with your specific bottle - even if you’ve taken the drug before under a different brand.
Can I rely on my phone’s medication app to remind me of special instructions?
Apps are great for timing reminders, but they don’t replace reading the label. Many apps don’t include special instructions like "avoid sunlight" or "shake well." They also don’t know if your pharmacy added a sticker with new info. Use apps as a tool - not your only source. Always double-check the physical label and ask your pharmacist if anything seems unclear.
Why do some labels have icons like a sun or a fridge?
Those icons are visual cues meant to help people who struggle with reading. A sun means "avoid sunlight" or "take in daylight." A fridge means "store in refrigerator." But the U.S. uses them on only 15% of labels - compared to 68% in Europe. Don’t assume the icon means what you think. Always read the text next to it. If you’re unsure, ask your pharmacist to explain what the symbol means for your specific drug.

Vu L
December 29, 2025 AT 04:50Bro, 'take with food' means eat a whole damn burger, not a single almond. I once took my antibiotic with a grape and spent the next 12 hours feeling like a zombie. Pharmacists don't care. Labels are written by lawyers who've never eaten a meal.
James Hilton
December 29, 2025 AT 15:02Let me guess - next they’ll tell us ‘avoid sunlight’ means don’t go outside. 😂 I’m just glad we’re not being told to ‘breathe in oxygen’ with a 10-point font and a sticker. At this point, my meds should come with a TikTok tutorial. #MedicationSurvivalGuide
Ryan Touhill
December 30, 2025 AT 20:02One cannot help but observe the alarming epistemological dissonance inherent in contemporary pharmaceutical labeling practices. The conflation of semiotic clarity with bureaucratic minimalism has resulted in a systemic failure of patient agency. One might argue that the FDA’s 10-point font mandate is less a regulatory intervention and more a performative gesture - a symbolic appeasement to the illiterate masses while the structural causes - namely, the commodification of healthcare - remain unaddressed. The real issue isn’t the label; it’s the commodification of human vulnerability.
Teresa Marzo Lostalé
December 31, 2025 AT 13:27Honestly? I just stare at the bottle until it feels like it’s talking back. 🤔 I once took my blood pressure med with a glass of wine because 'with food' sounded like 'with vibes.' Turned out I was fine. Maybe the real instruction is 'listen to your body.' Or maybe I’m just lucky. 🍷
ANA MARIE VALENZUELA
January 1, 2026 AT 15:16People are dumb. If you can’t read a label, don’t take the medicine. Simple. You think a pharmacy is your therapist? Go to school. Learn. Or better yet - don’t be a walking liability. I’ve seen people take insulin with soda. That’s not a mistake. That’s a public health hazard. And no, ‘take with food’ doesn’t mean ‘take with a Pop-Tart.’
Gran Badshah
January 1, 2026 AT 19:10I’m from India, we don’t have these labels here. We just ask the pharmacist - ‘Bhaiya, yeh tablet kis ke saath lena hai?’ He says ‘with roti.’ That’s it. No stickers, no inserts. Maybe the American system is overcomplicating it. We survive on trust, not 70% contrast.
Ellen-Cathryn Nash
January 3, 2026 AT 18:49It’s not just about instructions - it’s about dignity. When you’re elderly, sick, or scared, you shouldn’t have to decode hieroglyphics just to stay alive. The fact that we’ve normalized this level of neglect in healthcare says more about our society than it does about patient literacy. I cried reading about that woman who bled for months because of a sticker. That’s not negligence. That’s betrayal.
Samantha Hobbs
January 3, 2026 AT 21:01Wait so if I take my pill with a smoothie - is that food? I made one with kale, banana, and protein powder. Is that a full meal? I’m confused now. 😅 Also, why do they always put the important stuff on the back sticker? Like, is it a game? Find the hidden instructions!
Nicole Beasley
January 4, 2026 AT 18:37My app reminds me to take my meds, but it never tells me if I should eat a steak or just a cracker 🤷♀️ I asked my pharmacist and she said ‘it depends on the drug’… so now I have a sticky note on my fridge that says ‘ASK BEFORE YOU SWALLOW’ 😂