Stopping steroids suddenly can be dangerous-really dangerous. If you’ve been on prednisone or another glucocorticoid for more than a few weeks, your body has stopped making its own cortisol. That’s normal. But when you cut the medicine too fast, your adrenal glands can’t snap back in time. The result? Crushing fatigue, dizziness, joint pain, or worse-an adrenal crisis that lands you in the ER. And even if you avoid that, your autoimmune disease might come roaring back harder than before. This isn’t theory. It’s what happens every day in clinics and emergency rooms.
Why Your Body Needs Time to Recover
When you take steroids like prednisone, they mimic cortisol, the hormone your adrenal glands naturally make. Your body notices the extra supply and says, "We don’t need to work anymore." So it shuts down production. That’s fine while you’re on the meds. But when you stop, your adrenals don’t just flip back on. They need time-weeks or months-to wake up again.Research from the Mayo Clinic shows that if you’ve been on steroids for more than three to four weeks, your HPA axis (that’s your hypothalamus-pituitary-adrenal system) is basically asleep. Abruptly stopping means no cortisol when your body needs it most-during stress, illness, or even just standing up too fast. That’s when you get low blood pressure, fainting, or nausea. In severe cases, it can be life-threatening.
And here’s the catch: even if you don’t feel sick, your immune system might be waiting to strike. If you’re tapering for rheumatoid arthritis, lupus, or inflammatory bowel disease, pulling the steroid too fast can trigger a flare. You might end up back on a higher dose than you started with. That’s why tapering isn’t just about avoiding side effects-it’s about keeping your disease under control.
How Tapering Actually Works (Step by Step)
There’s no one-size-fits-all plan. But most doctors follow a three-phase approach based on how long and how much you’ve been on steroids.Phase 1: Rapid Taper (High Dose)
If you’re on more than 20-40 mg of prednisone daily, you’ll usually drop by 5-10 mg every week. For example, going from 40 mg to 30 mg, then 20 mg. This phase is quick because your body still has some cortisol production left. It’s also the safest window to reduce fast-your adrenals aren’t completely shut down yet.
Phase 2: Gradual Taper (Mid Dose)
Once you hit 20 mg, the pace slows. You’ll drop by 5 mg every two weeks, then 2.5 mg weekly until you reach 10 mg. This is where many people start feeling off. Fatigue, muscle aches, joint pain, and trouble sleeping are common. These aren’t signs you’re getting sicker-they’re signs your body is trying to restart its own cortisol production. Pushing too hard here can backfire.
Phase 3: Slow Taper (Low Dose)
Below 10 mg, every milligram matters. Reducing by 2.5 mg every two weeks gets you to 5 mg. Then you drop to 2.5 mg over the next two to four weeks. At this point, you’re near the body’s natural production level (about 5-7 mg/day of prednisone). Some doctors recommend switching to hydrocortisone here because it’s shorter-acting and might help your adrenals wake up faster. But studies show most people taper fine without switching. The Australian Prescriber says there’s little proof hydrocortisone makes a real difference for most patients.
How long does this take? If you were on high-dose steroids for just a few weeks, you might be done in a month. But if you’ve been on them for six months or more, expect three to six months of slow, careful reductions. Rushing this phase is the number one reason people end up back in the hospital.
What Withdrawal Really Feels Like
You might hear people say, "I just felt tired," but withdrawal is more than fatigue. WebMD’s 2023 survey of 1,200 patients found that 68% experienced symptoms during tapering. Here’s what they reported:- 42% had extreme tiredness-even after a full night’s sleep
- 37% got joint or muscle pain that felt like their arthritis was flaring
- 29% had trouble sleeping or felt anxious for no reason
- 18% developed nausea, dizziness, or low blood pressure
One Reddit user described it as a "taper tantrum"-a sudden return of pain when going from 7.5 mg to 5 mg. They had to hold at 7.5 mg for two weeks before trying again. That’s not weakness. That’s biology. Your body isn’t broken. It’s just slow to recover.
What helps? Gentle movement. A 2022 review in Medical News Today found that patients who did 10-15 minutes of walking twice a day reduced stiffness by 57% compared to those who stayed in bed. Daily 10-minute meditation cut anxiety symptoms by 43%. Yoga, warm baths, and pool exercises also helped. These aren’t magic fixes-they’re support systems while your body heals.

What Your Doctor Should Tell You
Too many patients are given a vague script: "Cut back slowly." That’s not enough. The Mayo Clinic says 41% of withdrawal complications happen because patients didn’t understand their taper schedule. You need specifics:- A written plan with exact daily doses for each week
- Clear instructions on what to do if you get sick (more on that below)
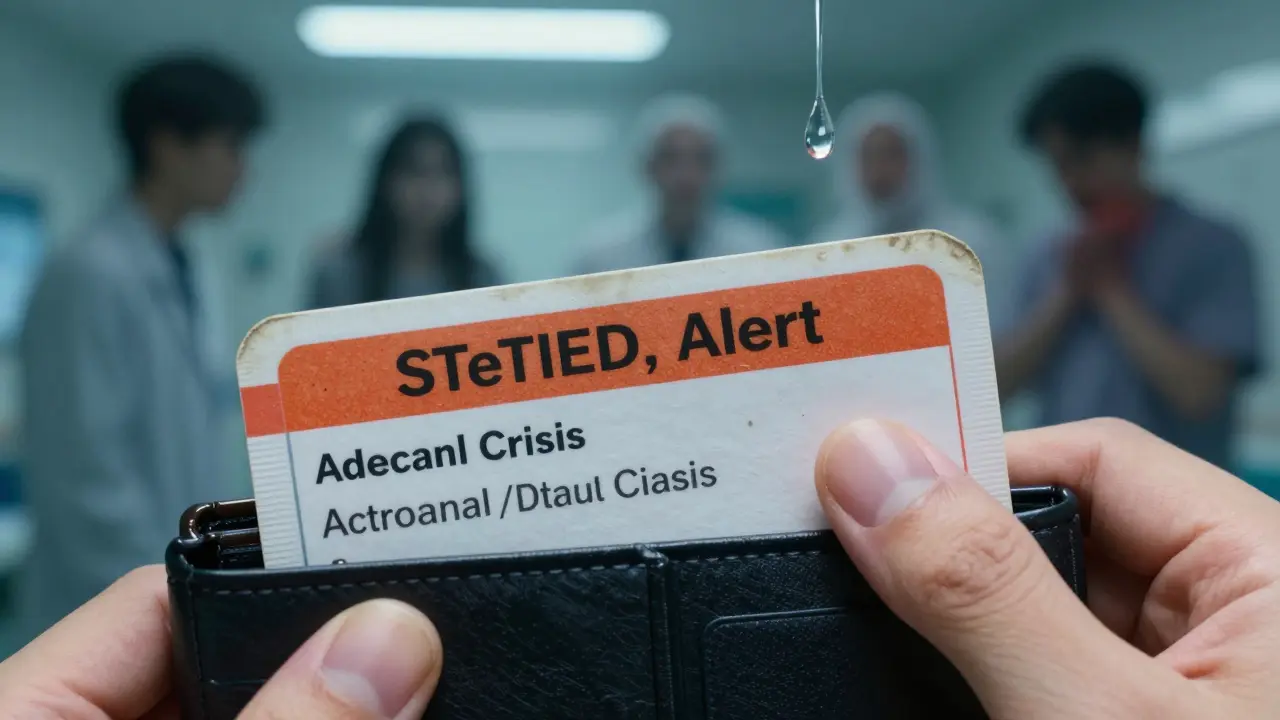
- A warning to carry a steroid alert card for at least 12 months
That card? It’s small. It says you’ve been on steroids and might need emergency hydrocortisone if you’re in an accident or get seriously ill. Even if you’ve been off for months, your adrenals might still be asleep. Endocrine society data says full recovery can take up to 18 months.
And here’s something most people don’t know: if you get a fever, infection, surgery, or even a bad flu, you need to temporarily increase your steroid dose. This is called "sick day rules." Skipping this step is why 18% of emergency visits for recently tapered patients happen. Your body needs extra cortisol to handle stress. No steroids = no defense.
New Ways of Thinking About Tapering
The old way was: "Take it down by 5 mg every two weeks, no matter what." Now, doctors are shifting. The American College of Rheumatology’s 2023 guidelines say: "Taper based on disease activity, not just time."For example, if you have rheumatoid arthritis, your doctor might check your DAS28 score-a measure of joint swelling and pain. If it’s low and stable, they might cut faster. If it’s creeping up? They’ll pause the taper. This personalized approach is becoming standard.
There’s also emerging tech. The Prednisone Taper Assistant app, launched in early 2023, lets you log symptoms daily. It uses AI to adjust your schedule. In pilot studies, it improved adherence by 82%. That means fewer mistakes, fewer flares.
And research is getting smarter. A 2023 study in the Journal of Clinical Endocrinology & Metabolism found that a simple CRH stimulation test could predict with 89% accuracy whether someone could stop steroids safely. It’s not widely available yet, but it’s coming.
What to Do If You’re Struggling
If you’re tapering and things feel worse, don’t panic. Don’t skip doses. Don’t double up. Call your doctor. Here’s what to do:- If fatigue or pain returns, hold your dose for 1-2 weeks. Don’t rush.
- Track your symptoms in a notebook or app. Patterns help your doctor adjust your plan.
- Don’t stop steroids on your own, even if you feel fine. That’s how adrenal crises start.
- If you’re sick-fever, infection, injury-double your dose immediately and call your doctor.
And remember: if your doctor doesn’t give you a clear plan, ask for one. You have the right to know exactly what to take, when, and why.
Final Thoughts: Patience Is the Medicine
Steroid tapering isn’t about getting off fast. It’s about getting off safely. It’s not a race. It’s a slow, careful recovery. Your body didn’t stop making cortisol overnight-it won’t start again overnight either.For people with autoimmune diseases, steroids are a lifeline. But they’re not a cure. Tapering is the bridge to life without them. Do it right, and you avoid hospital visits, flares, and long-term damage. Do it wrong, and you risk everything you’ve worked for.
The science is clear. The tools are here. The key? Listen to your body. Stick to the plan. And don’t be afraid to ask for help when things get hard.
Can I stop prednisone cold turkey if I’ve only been on it for two weeks?
If you’ve been on prednisone for less than three weeks, your adrenal glands likely haven’t fully shut down, so a sudden stop is usually safe. But even then, it’s not recommended. Doctors still advise a short, simple taper-like cutting by 5 mg every few days-to avoid any risk of temporary fatigue or low blood pressure. Always check with your doctor before stopping.
Why do I feel worse when I reduce my steroid dose?
You’re not getting sicker-you’re recovering. When you reduce steroids, your body starts trying to make its own cortisol again. That process takes time and can cause fatigue, joint pain, or mood swings. These are signs of withdrawal, not disease flare. Slowing the taper or adding gentle movement and stress-reduction techniques often helps. If symptoms are severe, hold your dose and talk to your doctor.
Should I switch from prednisone to hydrocortisone before finishing my taper?
Some doctors recommend switching to hydrocortisone at low doses because it has a shorter half-life and may help the adrenal glands wake up faster. But evidence is weak. Most studies show patients can successfully taper directly from prednisone without switching. The Australian Prescriber and the PMC primer both say this approach isn’t necessary for most people. Talk to your doctor about whether it’s right for you, but don’t assume it’s better.
How long does it take for my adrenals to recover after stopping steroids?
Recovery time varies. For short-term use (under 3 weeks), it can take a few days to weeks. For long-term use (6+ months), full recovery can take 6 to 18 months. During that time, your body still needs extra cortisol during stress. That’s why you should carry a steroid alert card for at least 12 months-and sometimes longer. Don’t assume you’re "cured" just because you stopped the pills.
What should I do if I get sick while tapering?
If you get sick-fever, infection, injury, or surgery-you must increase your steroid dose immediately. Your body needs extra cortisol to handle stress. The general rule is to double your current dose for 2-3 days, then return to your taper schedule once you’re better. If you’re unsure, call your doctor. Skipping this step is the leading cause of adrenal crisis in recently tapered patients.


Annie Joyce
February 12, 2026 AT 14:46Man, I thought I was going crazy when I hit phase 2 of my taper. Joint pain, zero energy, and my dog could tell I was off-I’d just stare at the wall. Turns out? My adrenals were napping. I started doing 10-minute walks after breakfast and honestly? It’s been a game-changer. Not magic, but it keeps me from crawling back into bed. Also, warm baths. Always the warm baths.
Rob Turner
February 13, 2026 AT 22:14Just wanna say-this post is a godsend. I’ve been tapering for 5 months now and I swear, if someone had told me ‘your body isn’t broken, it’s just slow’ six months ago, I’d’ve hugged them. I’m British, so I don’t do drama, but this? This is the kind of clarity you need when you’re stuck between ‘feeling fine’ and ‘feeling like death’. 🙏
steve sunio
February 14, 2026 AT 07:47lol so you’re telling me my body needs ‘time’ to wake up? like it’s on snooze? why not just give me a coffee and a slap? this whole thing feels like overmedicalized BS. i’ve seen people on prednisone for 2 years and they’re fine. just stop being weak.
athmaja biju
February 15, 2026 AT 16:40How can you even think about tapering when your country doesn’t even have universal healthcare? In India, we don’t get the luxury of ‘phases’. You either get the meds or you don’t. And if you’re lucky? You get a doctor who actually listens. This whole post reads like a rich person’s guide to suffering. Meanwhile, my cousin is still on 40mg because she can’t afford follow-ups.
Robert Petersen
February 15, 2026 AT 21:33Hey, I’ve been through this too-twice. First time I rushed it, ended up in the ER. Second time? I followed the plan, walked every day, meditated for 10 minutes, and tracked everything in a notebook. It sucked, but I didn’t crash. You’re not alone. And no, you’re not weak for needing time. Your body’s doing the hard work. Just keep showing up for it.
Craig Staszak
February 17, 2026 AT 13:21One thing no one talks about: the emotional rollercoaster. I went from ‘I’m fine’ to crying over spilled coffee because my cortisol was tanking. Not depression. Not anxiety. Just biology. I started saying ‘this is my body healing’ out loud every morning. Sounds dumb but it helped. Also, yoga. Always yoga.
alex clo
February 19, 2026 AT 02:42The data presented here is methodologically sound and aligns with current endocrine guidelines. The emphasis on HPA axis suppression and the phased tapering model is consistent with the 2023 American College of Rheumatology recommendations. However, the anecdotal references to Reddit users and WebMD surveys lack peer-reviewed validation and should be contextualized accordingly.
Joanne Tan
February 19, 2026 AT 10:04OMG I just hit 2.5mg and thought I was dying. My hands were shaking, I couldn’t sleep, and I felt like my bones were melting. Then I remembered the walking tip. Just 10 mins outside. Now I do it every morning. It’s not a cure but it’s my lifeline. Also-yoga pants. Always yoga pants. No shame.
Carla McKinney
February 20, 2026 AT 21:53Everyone’s acting like this is some groundbreaking revelation. I’ve been a nurse for 18 years. This is standard textbook material. If you didn’t know this already, you shouldn’t have been on steroids long-term without a specialist. Stop acting surprised. Education isn’t optional.
Sonja Stoces
February 21, 2026 AT 13:48So let me get this straight-you’re telling me I need to take a pill for 6 months, then slowly stop it over a year, and then carry a card forever? What if I forget? What if I get hit by a bus and no one knows? This is ridiculous. Why not just never take it in the first place? #Overmedicalized
Kristin Jarecki
February 23, 2026 AT 05:46While the clinical framework presented is accurate and evidence-based, I would respectfully suggest that the tone, though well-intentioned, inadvertently minimizes the psychological burden of prolonged glucocorticoid dependence. The emphasis on patience and biology, while scientifically valid, may inadvertently discourage patients who experience persistent HPA axis dysfunction beyond 18 months. Further research into biomarkers of adrenal recovery is urgently needed.
Jonathan Noe
February 24, 2026 AT 02:07Did you know the Prednisone Taper Assistant app has a feature that sends you a daily affirmation? Like, ‘Your adrenals are waking up, one milligram at a time.’ I thought it was cheesy until I cried the first time I got it. Now I look forward to it. It’s dumb. It’s real. And it helps.
Jim Johnson
February 25, 2026 AT 11:52My doc gave me a written plan. Exact doses. Every week. I printed it. Laminated it. Put it on my fridge. And when I got sick last month? I doubled my dose like it said. No panic. No guesswork. That’s what you need. Not vibes. Not memes. A plan. And if your doctor won’t give you one? Find a new one. Seriously.