Syphilis and Fertility Risk Calculator
This tool helps evaluate potential risk factors for syphilis-related infertility. Answer the following questions honestly to get an assessment of your risk level.
Your risk assessment will appear here after answering the questions and clicking "Assess My Risk"
Check off symptoms that apply to you:
Selected Symptoms:
Imagine planning a family and then learning a hidden infection could be blocking the road. Syphilis is a bacterial sexually transmitted infection caused by Treponema pallidum that can silently damage the reproductive system if it goes untreated. While many think of syphilis as a historical scourge, it’s still a modern health issue and, surprisingly, a contributor to infertility in both men and women. This guide walks you through how the bug interferes with fertility, how doctors spot it, and what treatment options can restore the chance of conceiving.
Key Takeaways
- Syphilis can cause infertility by damaging the uterus, fallopian tubes, prostate, or sperm production.
- Early-stage infection often shows no symptoms, so routine STI testing is crucial for anyone trying to conceive.
- Standard treatment is a single dose of Penicillin; alternative antibiotics are used only when penicillin isn’t an option.
- Most people regain normal fertility within 6‑12 months after successful therapy, provided no irreversible damage occurred.
- Prevention, partner notification, and follow‑up testing are the best ways to keep syphilis from affecting future pregnancies.
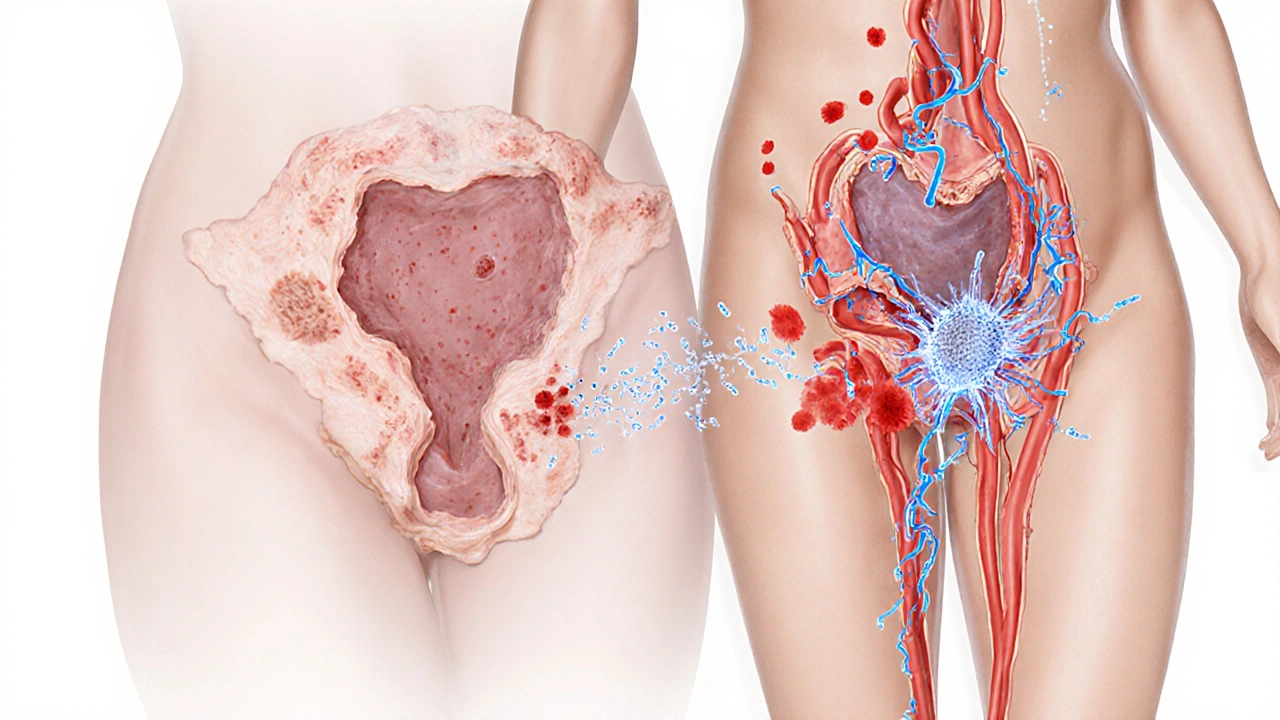
How Syphilis Threatens Fertility
Syphilis progresses through three main stages-primary, secondary, and tertiary-each with its own set of risks.
In the primary stage, a painless ulcer (chancre) appears at the infection site. Most people never notice it, and the bacteria begin migrating through the bloodstream.
During secondary syphilis, a rash, fever, and sore throat may emerge. The bacterium can now reach the reproductive organs. In women, it can inflame the uterus and fallopian tubes, leading to scarring that blocks egg transport. In men, it may cause prostatitis or epididymitis, reducing sperm count and motility.
If the infection reaches tertiary syphilis-a rare outcome in countries with good healthcare-the damage becomes permanent. Granulomas (gummas) can form in the pelvic region, causing severe obstruction. Even before reaching this stage, chronic inflammation can lower fertility odds significantly.
Another hidden danger is co‑infection with other STIs, especially HIV. Immune suppression can worsen syphilis‑related organ damage, further compromising reproductive health.
When to Suspect Syphilis‑Related Infertility
Infertility is defined as the inability to conceive after 12 months of regular, unprotected intercourse. If you’ve hit that wall, ask yourself these questions:
- Have you or your partner ever had an untreated sore or rash on the genitals, mouth, or anus?
- Do you experience unexplained pelvic pain, painful urination, or swelling in the groin?
- Has a recent STI test come back positive for syphilis, or have you missed routine screenings?
Even without symptoms, a hidden syphilis infection can be the culprit. That’s why many fertility clinics include a comprehensive STI panel-blood tests for syphilis, chlamydia, gonorrhea, and HIV-before starting assisted reproductive treatments.
Diagnosing Syphilis in the Context of Infertility
Doctors rely on two types of tests: non‑treponemal and treponemal.
| Test | Type | What it Detects | Typical Use |
|---|---|---|---|
| VDRL | Non‑treponemal | Antibodies that appear during active infection | Screening & monitoring treatment response |
| RPR | Non‑treponemal | Similar to VDRL, easier to read | Initial screen, especially in labs |
| FTA‑ABS | Treponemal | Specific antibodies against Treponema pallidum | Confirmatory test after a positive screen |
| TP‑PA | Treponemal | Detects long‑lasting antibodies | Confirming past infection or treatment success |
If you’re being evaluated for infertility, a positive VDRL or RPR followed by a confirmatory treponemal test (FTA‑ABS or TP‑PA) will prompt immediate treatment.
Treatment Options: What Really Works
The cornerstone of syphilis therapy is penicillin. The World Health Organization and the Australian STI Guidelines both recommend a single intramuscular dose of benzathine penicillin G for early syphilis. For late or tertiary disease, three weekly doses are standard.
Why penicillin? It kills Treponema pallidum quickly, clears the bloodstream, and has decades of safety data. Alternatives like doxycycline (100mg twice daily for 14days) or azithromycin (1g single dose) are reserved for patients with a confirmed penicillin allergy, but they’re slightly less effective and may require stricter follow‑up.
Below is a quick side‑by‑side look at the most common regimens.
| Regimen | Dose | Duration | Success rate (early) | Notes |
|---|---|---|---|---|
| Benzathine Penicillin G | 2.4millionIU IM | Single dose (early) / 3 doses weekly (late) | ≈98% | First‑line, safe in pregnancy |
| Doxycycline | 100mg PO | 14days | ≈93% | Avoid in pregnancy, photosensitivity |
| Azithromycin | 1g PO | Single dose | ≈85% | Resistance reported in some regions |
After the injection, doctors repeat the VDRL/RPR at 6months and 12months to confirm that antibody titers have dropped four‑fold, indicating cure.

Can Fertility Bounce Back After Treatment?
Good news: most reproductive damage caused by early‑stage syphilis is reversible. Studies from Australian fertility clinics show that 80‑90% of women who received timely penicillin regained normal tubal patency within a year, as verified by hysterosalpingography. In men, sperm concentration and motility typically improve within 3‑6months after treatment, provided the infection didn’t lead to permanent epididymal scarring.
However, if the infection progressed to tertiary syphilis with gummatous lesions, surgical repair may be required, and success rates drop to 40‑60%.
Key factors that boost recovery:
- Early detection-before organ damage sets in.
- Complete adherence to the prescribed antibiotic course.
- Partner treatment to prevent reinfection.
- Follow‑up testing to confirm cure before attempting conception.
If you’re already in an assisted reproductive technology (ART) program, doctors may advise a waiting period of 6months after the final dose of penicillin to ensure the infection is fully cleared.
Prevention: Keeping Syphilis From Stealing Your Family Plans
Prevention is simple but powerful:
- Use condoms consistently, especially with new or multiple partners.
- Get a full STI panel at least once a year, or sooner if you notice any sores.
- If diagnosed, inform all recent sexual partners so they can get tested and treated.
- Pregnant women should be screened at the first prenatal visit; untreated syphilis can cause miscarriage, stillbirth, or congenital infection.
- Vaccination doesn’t exist for syphilis, so regular testing is your best shield.
Australian health services offer free or low‑cost syphilis testing through community clinics, sexual health centers, and some general practices. Knowing your status early saves heartache later.
Frequently Asked Questions
Can a single dose of penicillin cure all stages of syphilis?
For early (primary or secondary) syphilis, a single intramuscular dose of benzathine penicillin G is enough. Late or tertiary syphilis requires three weekly doses to fully eradicate the bacteria.
How long after treatment can I try to get pregnant?
Most clinicians recommend waiting at least six months and confirming a negative VDRL/RPR test before trying to conceive. This window ensures the infection is cleared and reduces the risk of reinfection.
Is there any risk to the baby if the mother had syphilis during pregnancy?
Untreated maternal syphilis can lead to miscarriage, stillbirth, or congenital syphilis, which may cause severe birth defects. Prompt treatment with penicillin in pregnancy virtually eliminates these risks.
What if I’m allergic to penicillin?
Allergy to penicillin complicates treatment. Doctors may use doxycycline or azithromycin, but they require careful monitoring and a longer follow‑up schedule. In pregnancy, desensitization to penicillin is the preferred route.
Can syphilis cause permanent infertility?
If the infection reaches tertiary syphilis and creates scar tissue in the uterus, fallopian tubes, prostate, or epididymis, the damage can be permanent. Early detection and treatment dramatically lower this risk.


Sriram Musk
October 5, 2025 AT 14:00It's good to see a concise overview of how syphilis can affect reproductive health. The piece manages to strike a balance between medical detail and readability, which is helpful for folks without a clinical background. I appreciate the inclusion of both non‑treponemal and treponemal testing algorithms, as many patients get confused by the terminology. The treatment section correctly emphasizes penicillin as first‑line therapy while noting alternatives for allergic patients. Overall, this article serves as a solid starting point for anyone concerned about fertility and STI risk.
allison hill
October 7, 2025 AT 21:40While the guide appears thorough, it conveniently overlooks the fact that many modern studies suggest hidden reservoirs of infection in underserved populations. The assertion that a single penicillin dose resolves early syphilis fails to account for documented treatment failures in regions with rampant drug resistance. A more skeptical tone would better serve readers seeking a full picture.
Tushar Agarwal
October 10, 2025 AT 05:20Great effort on the layout! 👍 The risk calculator looks user‑friendly and the symptom checker is a neat interactive touch. Keep it up, the info is super useful for couples planning families.
Richard Leonhardt
October 11, 2025 AT 09:13Thanks for the kind words! Just a heads‑up, the "single dose" line could use a tiny tweak – it’s technically true but best practice is to re‑check serology after a few months. Also, don’t forget to mention that doxycycline can be a fallback, altho it’s not ideal for pregnant folks. I’ll add a note about follow‑up testing to make the guide even stronger.
Shaun Brown
October 12, 2025 AT 13:06The article does a respectable job of outlining the classical stages of syphilis. However, it completely glosses over the socioeconomic factors that drive infection rates in marginalized communities. By ignoring how poverty, limited access to healthcare, and education intersect with disease transmission, the piece falls into a textbook echo chamber. Moreover, the reliance on outdated treatment algorithms betrays a lack of engagement with the latest WHO guidelines. The claim that a single dose of penicillin cures all early cases is technically correct but misleading, because adherence and follow‑up testing are essential. The author also fails to mention the rising rates of macrolide resistance in certain regions, a fact that could impact the efficacy of azithromycin alternatives. While the fertility section is thorough, it sidesteps a critical point: the emotional toll of infertility on couples, which often leads to mental health crises. The discussion of partner notification is presented as a simple administrative step, ignoring the cultural stigma that can prevent disclosure. In addition, the article does not address the role of telemedicine in expanding STI testing access, which has become particularly relevant after the pandemic. The statistical data cited are drawn from studies that are over a decade old, raising questions about their current applicability. A more nuanced approach would integrate recent epidemiological trends from both high‑income and low‑income settings. The absence of any patient narratives makes the piece feel detached and clinical. The graphical risk calculator is a nice UI feature but offers no explanation of the underlying algorithm, leaving users in the dark about its validity. Finally, the recommendation to wait six months before conception is overly conservative for patients who have shown rapid serological response. In summary, the article is a solid starter guide but would benefit from a deeper, more critical analysis of systemic barriers and emerging research.
Damon Dewey
October 12, 2025 AT 13:53Your alarmist tone is completely unnecessary.
Dan Barreto da Silva
October 13, 2025 AT 17:50Honestly, the whole "just get tested" vibe feels a bit dismissive when people are dealing with real fear and stigma. You can't just brush off the anxiety that comes with a potential diagnosis. Some empathy would go a long way here.
Ariel Munoz
October 14, 2025 AT 21:43Look, if you’re not proud of your country’s health system, you’re just making excuses. The facts clearly show that penicillin works worldwide, regardless of politics.
Ryan Hlavaty
October 16, 2025 AT 01:36It's morally imperative that we prioritize universal STI screening before anyone thinks about starting a family. Ignoring this responsibility is tantamount to endangering future generations. We must hold ourselves accountable and demand accessible testing for all.
Chris Faber
October 17, 2025 AT 05:30Hey man, I get where you're coming from but let's keep it chill. Everyone's trying to do right by their partners and kids
aura green
October 18, 2025 AT 09:23Wow, this guide really pulls out all the stops, doesn’t it? 😏 It’s like a textbook got a makeover and decided to host a party. The risk calculator is slick, yet I’m still left wondering if the algorithm is more myth than science. Still, I have to give props for the thorough treatment rundown – who knew penicillin could be so dramatic? The fertility section reads like a romance novel gone wrong, but hey, at least it warns us before heartbreak. All in all, great job, and thanks for the smiley faces! 😊
Edward Morrow
October 19, 2025 AT 13:16Nice try hiding behind a glossy UI while the real data stays in the shadows. The so‑called "risk" is just a buzzword sprinkled over half‑baked stats. If you want credibility, stop dressing up vague math as science. And maybe, just maybe, stop pretending this is a free pass for reckless behavior.
Shayne Tremblay
October 20, 2025 AT 17:10Great work! This article gives hopeful couples a clear roadmap and the confidence to seek help. Remember, early testing and treatment can really turn the tide toward a healthy pregnancy.
Stephen Richter
October 21, 2025 AT 21:03While the encouragement is admirable, the content would benefit from a more rigorous citation of recent studies. Consider adding a section on psychosocial support for affected partners.
Musa Bwanali
October 23, 2025 AT 00:56You've done a solid job outlining the steps, but don't forget to push readers to act decisively. The sooner they get tested, the quicker they can protect their future families.
Allison Sprague
October 24, 2025 AT 04:50The guide is commendable, but it's riddled with vague phrasing that could mislead lay readers. Precise terminology-especially regarding serology thresholds-must be crystal clear. Moreover, omitting recent resistance patterns is a glaring oversight. Tighten the language, cite up‑to‑date sources, and the piece will truly shine.