Drug Interaction
When dealing with drug interaction, the way two or more medicines affect each other’s action in the body. Also known as medication interaction, it plays a key role in medication safety, preventing harmful outcomes when drugs are combined, can trigger an adverse drug reaction, unexpected side effects caused by drug mixtures, and hinges on pharmacokinetics, how the body absorbs, distributes, metabolizes, and excretes each drug. In short, drug interaction encompasses medication safety, requires knowledge of pharmacokinetics, and influences treatment outcomes.
Why It Matters for Everyday Health
Every time you add a new prescription, an over‑the‑counter pain reliever, or a vitamin supplement, you’re creating a potential interaction scenario. Clinical guidelines stress that clinicians must assess these combos before writing a new script, because a missed interaction can turn a simple therapy into a serious health risk. For example, combining certain blood thinners with NSAIDs can amplify bleeding risk, while mixing some antibiotics with statins may raise muscle toxicity. Knowing the interaction landscape lets both doctors and patients avoid preventable complications.
Common interaction culprits include food‑drug combos, like grapefruit juice slowing the breakdown of many cholesterol‑lowering agents, or caffeine boosting stimulant effects. These examples show how pharmacodynamics – the way drugs act on targets – intertwines with pharmacokinetics. When a drug’s metabolism is blocked, its concentration rises, intensifying both intended and unwanted effects. Understanding both sides helps you predict which pairings are safe and which need dose adjustments.
Technology now offers quick checks: many pharmacy apps and electronic health record systems flag risky combos in real time. These tools draw from massive databases that classify interactions by severity, guiding clinicians to pause, switch, or monitor therapy. For patients, a simple online checker can confirm whether a new OTC product is safe with their current regimen, adding another layer of medication safety.
Chronic disease management illustrates the stakes. A diabetic on metformin who starts a course of steroids may see blood sugar spikes, while a heart patient on nitrates must avoid phosphodiesterase‑5 inhibitors to prevent dangerous blood pressure drops. Each condition brings its own interaction profile, and ignoring these can derail long‑term treatment goals. That’s why up‑to‑date interaction knowledge is a cornerstone of effective care.
Staying current is easier than it sounds. Professional societies release annual updates to interaction guidelines, and major drug authorities publish safety alerts when new risks emerge. Subscribing to these resources or using reputable interaction checkers keeps you ahead of changes that could affect your therapy plan.
Below you’ll find a curated collection of articles that dive deeper into specific drug interaction topics—from detailed medication comparisons to practical tips for managing interactions in everyday life. Whether you’re a patient looking to understand a new prescription or a healthcare professional needing a quick refresher, the posts here aim to make drug interaction knowledge clear, actionable, and ready to use.
PDE5 Inhibitors and Nitrates: What You Need to Know About the Life-Threatening Blood Pressure Risk
Mixing PDE5 inhibitors like Viagra or Cialis with nitrates can cause life-threatening drops in blood pressure. Learn why this interaction is dangerous, how long to wait between doses, and what alternatives exist.
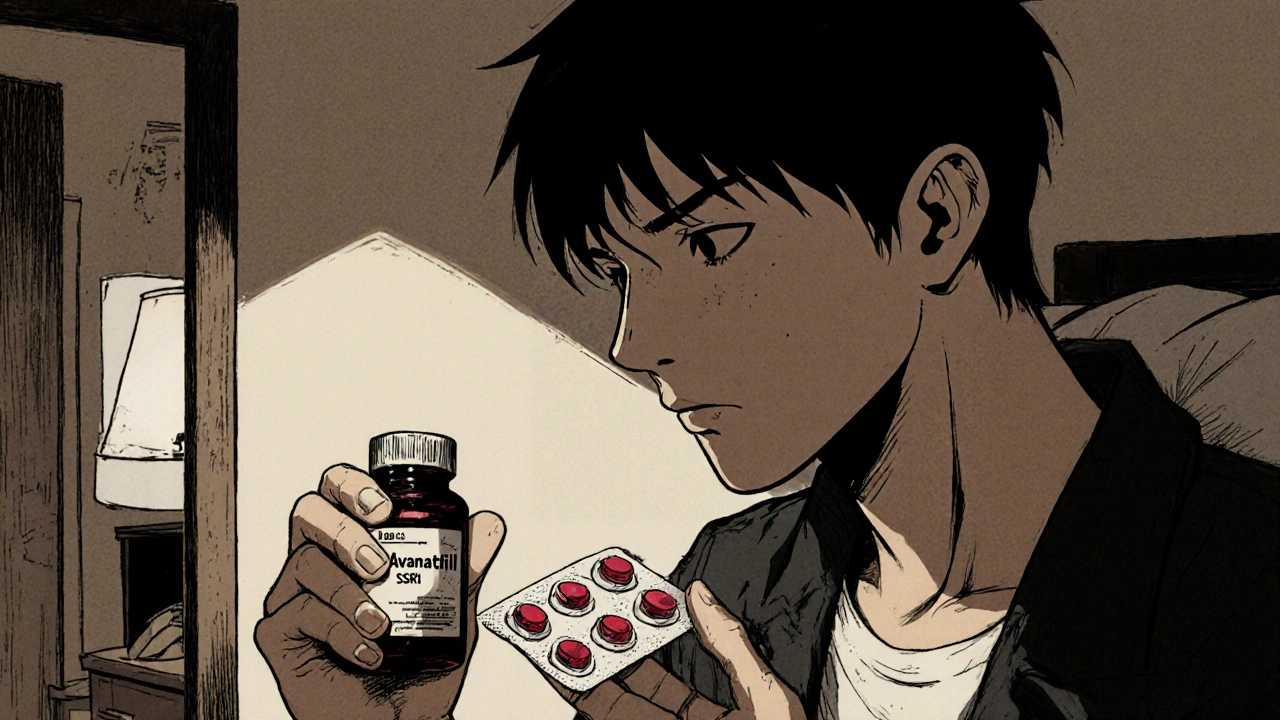
Avanafil and Antidepressants: Safe Combination Explained
Explore whether avanafil can be safely taken with antidepressants, covering interaction risks, side‑effects, dosage tips, and when to seek medical advice.