Understanding Neuroblastoma and its Complexities
Before unraveling the role of personalized medicine in neuroblastoma treatment, it is essential to understand what neuroblastoma is. Neuroblastoma is a type of cancer that develops from immature nerve cells found in several areas of the body. It primarily affects children, particularly those below the age of 5. The complexities of neuroblastoma lie in its varied behavior; it can be aggressive and spread quickly, or it may resolve on its own without treatment. The prognosis for neuroblastoma varies greatly, with some children recovering fully while others do not respond to treatment.
The Emergence of Personalized Medicine
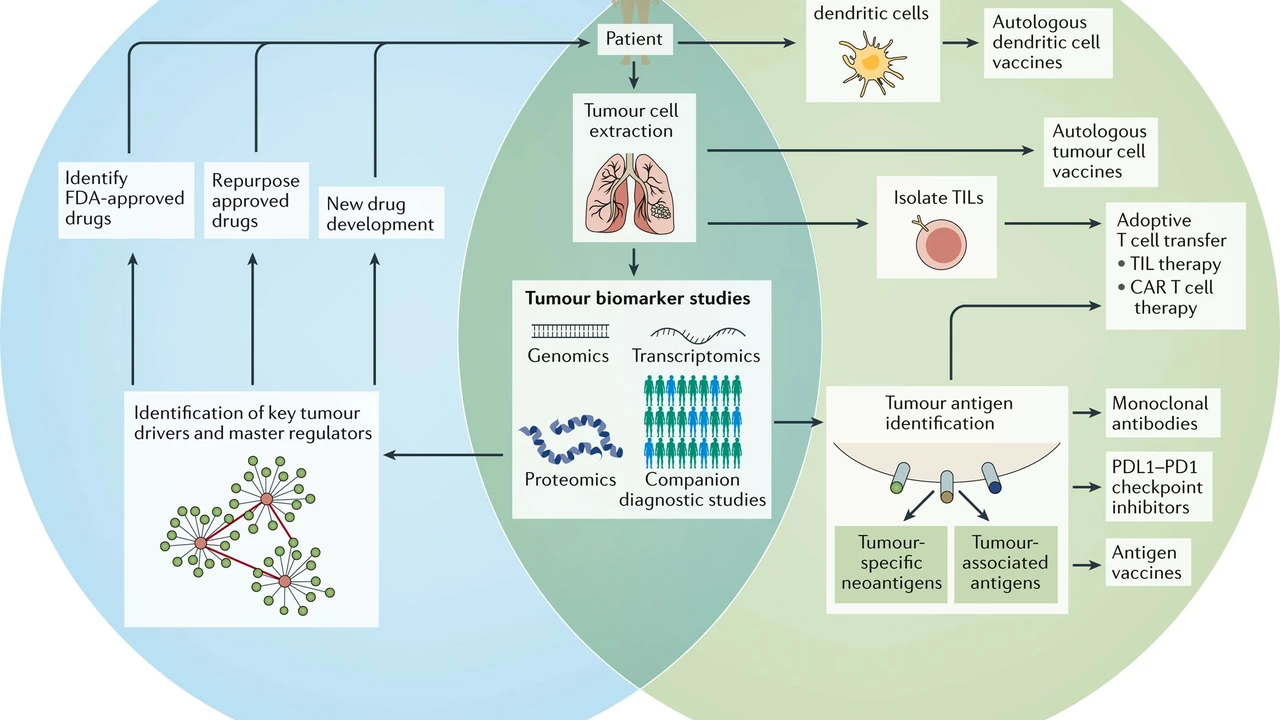
Enter personalized medicine, a new frontier in the healthcare landscape. Personalized medicine is a medical model that separates patients into different groups - with medical decisions, practices, interventions, and/or products being tailored to the individual patient based on their predicted response or risk of disease. The concept relies heavily on genetic information about a patient's disease. By understanding the genetic makeup of a patient's cancer, doctors can devise a treatment strategy that is specifically designed to target the cancer cells.
Genomic Sequencing in Neuroblastoma
Genomic sequencing plays a central role in personalized medicine. In the context of neuroblastoma, genomic sequencing helps identify specific genetic mutations responsible for the disease. Once these mutations are identified, they can be targeted with specific drugs. For instance, researchers have discovered that a mutation in the ALK gene is responsible for about 10% of neuroblastoma cases. Drugs that specifically target this mutation are now being used in clinical trials. This approach is radically different from traditional chemotherapy, which targets all rapidly dividing cells, leading to a host of side effects.
Efficacy of Personalized Medicine in Neuroblastoma Treatment
Personalized medicine holds great promise in the treatment of neuroblastoma. Early studies have shown that this approach can lead to better outcomes and fewer side effects compared to conventional treatments. However, it is critical to remember that personalized medicine is still a relatively new field, and there is much we don't know. Ongoing research is needed to fully understand the potential benefits and limitations of this approach. As more genetic mutations linked to neuroblastoma are discovered and more targeted drugs become available, the role of personalized medicine in neuroblastoma treatment is expected to grow.
The Future of Neuroblastoma Treatment
Given the promising results of personalized medicine in early studies, it is not unreasonable to envision a future where every child diagnosed with neuroblastoma will have their tumor genetically sequenced. This information could then be used to devise a personalized treatment plan that targets the specific mutations driving their disease. This could potentially lead to more effective treatments with fewer side effects, vastly improving the prognosis for children with neuroblastoma.
Concluding Thoughts
Personalized medicine represents a significant shift in how we approach neuroblastoma treatment. By tailoring treatment to the individual patient, we have the potential to dramatically improve outcomes and quality of life for children with this disease. While there are still many unknowns and challenges to overcome, the promise of personalized medicine is undeniable. It is our hope that as research advances, more children will benefit from this revolutionary approach to cancer treatment.

Carl Watts
July 26, 2023 AT 21:44Reading about neuroblastoma through the lens of personalized medicine feels like watching a kaleidoscope where each turn reveals a new pattern of hope. The disease's unpredictable nature reminds us that biology is a conversation, not a monologue. When we let the genome speak, we are finally listening to the patient rather than imposing a one‑size‑fits‑all regimen. This shift from generic chemotherapy to mutation‑targeted therapy is akin to moving from a blunt axe to a precision scalpel. Yet, we must remember that every genetic insight carries ethical weight, demanding both humility and rigor from the scientific community.
Brandon Leach
August 20, 2023 AT 04:53Personalized meds? Sure, if you like paying extra for fancy tests.
Alison Poteracke
September 18, 2023 AT 03:20It’s really encouraging to see how far we’ve come in trying to match treatments to each child’s unique cancer profile. The idea is simple: find the exact mutation driving the tumor and then hit that target with a drug that’s designed for it. This means fewer side effects because we’re not blasting all the fast‑growing cells at once. Kids who go through traditional chemo often end up with hair loss, nausea, and a lot of fatigue, which can be especially hard on young families. By using genomic sequencing, doctors can avoid many of those harsh experiences and focus on what actually matters – shutting down the cancer. Early studies have shown that children with ALK‑mutated neuroblastoma respond well to ALK inhibitors, which is a big win. It also opens doors for future research, because each successful case adds to a growing database of what works and what doesn’t. Parents can feel more empowered when they have detailed information about their child’s tumor, rather than being told to accept a generic protocol. The technology is getting cheaper and faster, making it realistic to sequence every tumor at diagnosis. This could become a standard part of the care pathway, just like blood tests are today. With more data, we’ll be able to spot patterns that we didn’t even know existed, leading to new drug targets. The hope is that, over time, the survival rates will rise and the quality of life for survivors will improve dramatically. It also means that the emotional burden on families might lessen, since they can see a clear, science‑driven plan rather than hoping for a miracle. While there are still challenges – such as access to testing in low‑resource settings and the need for more targeted drugs – the trajectory is positive. The community should keep supporting research, sharing data, and advocating for insurance coverage of these essential tests. Together, we can turn the promise of personalized medicine into a reliable reality for every child battling neuroblastoma.
Marianne Wilson
October 17, 2023 AT 01:46While the optimism is admirable, we must not overlook the glaring disparities in who actually receives these cutting‑edge treatments. Many families lack the resources or insurance coverage to afford genomic sequencing, leaving their children stuck with outdated protocols. Moreover, the data on long‑term outcomes for targeted therapies is still thin, so proclaiming them as panacea is premature. It’s also worth noting that focusing solely on genetics can obscure the role of environmental and socioeconomic factors in disease progression. A balanced approach, integrating personalized medicine with broader public health measures, would be far more responsible.
Patricia Bokern
November 9, 2023 AT 04:20Honestly, it feels like the pharma giants are just cashing in on every new mutation they discover. Every time a gene is linked to neuroblastoma, a new “miracle” drug appears, priced at absurd levels. I’m skeptical of all the hype – who’s really watching the long‑term side effects? It’s a classic case of profit over patients, and the whole system needs a reality check.