When you’re on TRICARE, getting your prescription filled shouldn’t feel like a maze. For millions of military families, TRICARE coverage for generics is the backbone of affordable, reliable care. But knowing which generics are covered, how much you’ll pay, and where to get them can make all the difference. The good news? Most prescriptions you need are covered - and often at a fraction of what civilian insurance charges. The trick is knowing the rules.
How TRICARE Covers Generic Drugs
TRICARE doesn’t just cover generics - it pushes them. About 92% of all prescriptions filled through TRICARE are for generic medications. Why? Because they work just like brand-name drugs but cost 80-85% less. The FDA says they’re identical in active ingredients, dosage, safety, and effectiveness. TRICARE’s formulary includes over 5,500 approved drugs, and most of them are generics.Not every generic is automatically covered, though. TRICARE organizes drugs into four tiers:
- Tier 1: Generic formulary drugs - The cheapest and most preferred. These are your go-to options.
- Tier 2: Brand-name formulary drugs - Covered, but you pay more unless no generic exists.
- Tier 3: Non-formulary drugs - Not on the list. You need prior authorization to get them covered.
- Tier 4: Non-covered drugs - Not covered at all. No exceptions.
If your doctor prescribes a generic that’s not on the formulary, you might need to wait 48-72 hours for approval. About 78% of these requests get approved if you show medical need. But if you skip checking the formulary first, you could end up paying full price at the pharmacy.
Where to Fill Your Prescription and How Much It Costs
Your out-of-pocket cost depends entirely on where you fill your prescription. There are three main options:- Military pharmacies - Best deal on the planet. If you’re eligible and live near a base, fill your generic here. Copay? $0. That’s right - zero. Whether you’re active duty, a retiree, or a family member, you pay nothing for any covered generic. No deductible. No surprise fees.
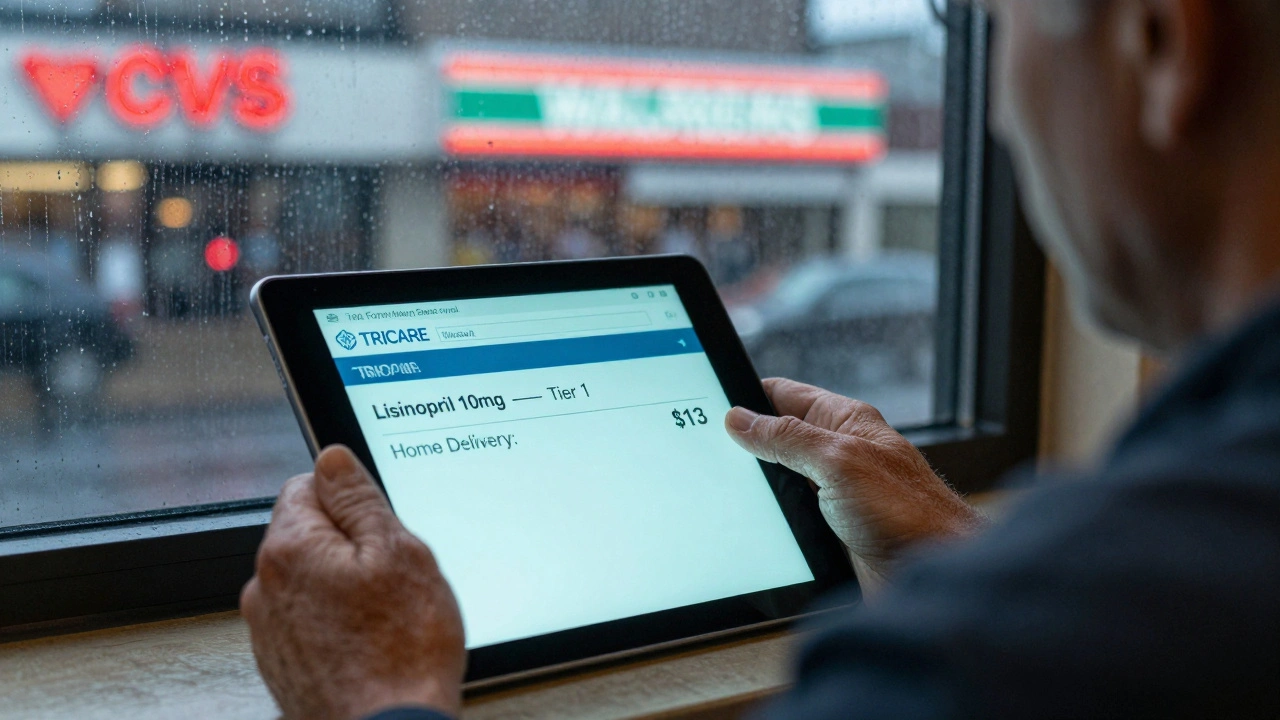
- TRICARE Home Delivery - Perfect for maintenance meds like blood pressure pills, diabetes drugs, or antidepressants. You get a 90-day supply shipped to your door. In 2025, the copay is $13. Starting January 1, 2026, it goes up to $14. Still cheaper than most civilian plans.
- Network retail pharmacies - CVS, Walgreens, Walmart, and others. For a 30-day supply of a generic, you pay $16 in 2025. This rate won’t change through 2026. If you need a med right away and can’t wait for home delivery, this is your backup.
Here’s the kicker: if you use a non-network pharmacy - like a local drugstore that doesn’t accept TRICARE - you’ll pay more. You’ll either owe 50% of the cost after your deductible (if you’re TRICARE Prime) or $48 or 20% of the total (whichever is higher) if you’re TRICARE Select. That’s why it’s critical to check if your pharmacy is in-network before you walk in.
How to Check If Your Generic Is Covered
You can’t assume a drug is covered just because it’s generic. Some generics are excluded - especially newer ones or those in controversial categories. The only way to know for sure? Use the TRICARE Formulary Search tool. It’s free, fast, and updated monthly.Enter the exact drug name and strength (like “Lisinopril 10 mg”). The tool tells you:
- Which tier it’s on
- Whether prior authorization is needed
- Your copay at each pharmacy type
- If it’s covered at all
Pro tip: Always check before your doctor writes the script. A 2025 beneficiary survey found that 28% of complaints came from people who didn’t check the formulary first. One Marine retiree said, “I got my generic cholesterol pill covered at home delivery for $14. My neighbor paid $30 at his pharmacy because he didn’t know TRICARE existed.”
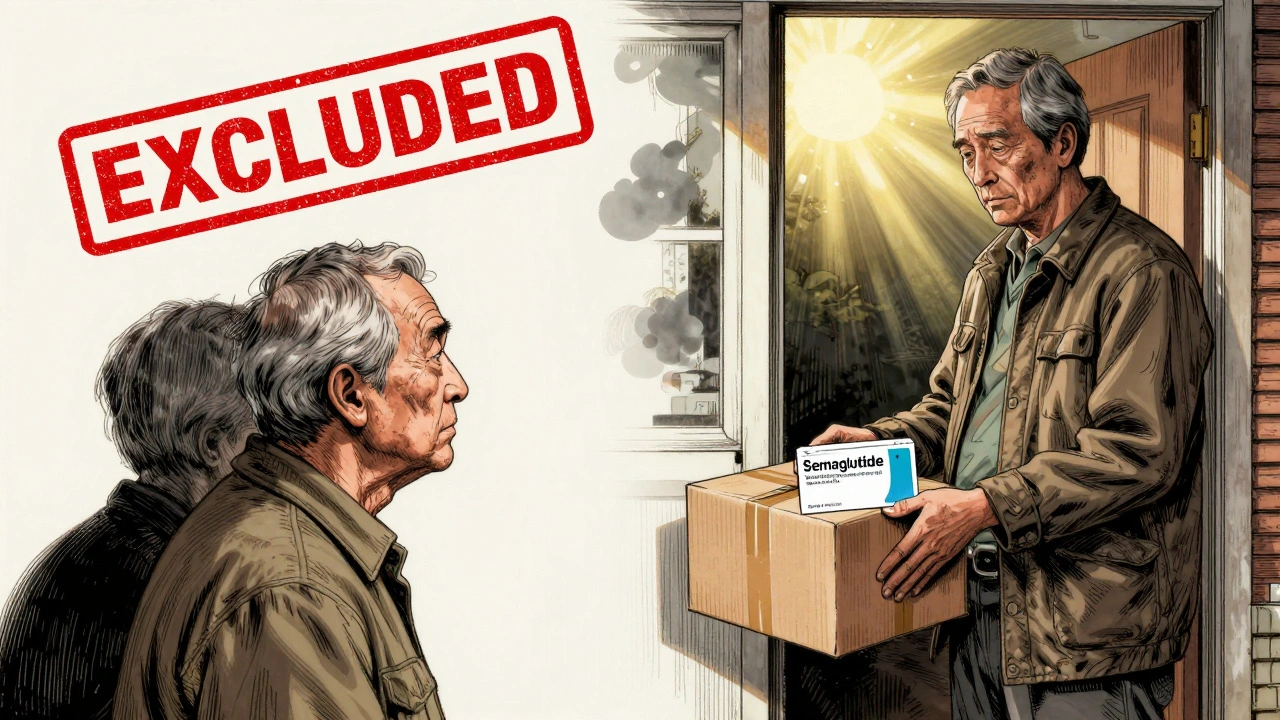
What’s Not Covered - And Why
TRICARE excludes some generics, even if they’re FDA-approved. The biggest change in 2025 was the August 31 cutoff for weight loss medications like semaglutide (Wegovy) and liraglutide (Saxenda). These are now excluded for TRICARE For Life beneficiaries - that’s retirees 65+ who also have Medicare. About 1.2 million people are affected. The Defense Health Agency says this was required by the 2024 National Defense Authorization Act. Critics call it a gap in care. The agency says they’re reviewing it.Another issue: generic biologics. These are complex drugs - like biosimilar versions of Humira or Enbrel. TRICARE requires higher prior authorization rates for them (22% more than regular generics) because of how they’re made. That means longer waits and more paperwork.
Also, TRICARE doesn’t cover over-the-counter drugs - even if your doctor recommends them. That includes things like generic ibuprofen or allergy pills. You’re on your own for those.
How TRICARE Compares to Other Plans
Let’s put TRICARE’s generic coverage in perspective:| Plan Type | 30-Day Generic Copay | 90-Day Generic Copay | Free Option? |
|---|---|---|---|
| TRICARE (Military Pharmacy) | $0 | $0 | Yes |
| TRICARE (Home Delivery) | N/A | $13 | No |
| TRICARE (Retail) | $16 | N/A | No |
| Medicare Part D | $7-$10 | $20-$30 | No |
| VA Pharmacy | $0 | $0 | Yes |
| Average Employer Plan | $15-$25 | $40-$60 | No |
TRICARE isn’t the cheapest overall - Medicare Part D has lower copays. But TRICARE is the only one that gives you a free option at military pharmacies. VA is free too, but only for veterans with service-connected conditions. TRICARE covers nearly all active duty, retirees, and families - no income limits, no means testing.
And while commercial plans might have wider formularies, TRICARE’s 94% access rate for chronic condition generics (like metformin or atorvastatin) beats the national average. Only 6% of users report trouble getting their maintenance meds.
What Beneficiaries Are Saying
Real people, real experiences:- “I get my blood pressure meds at the base pharmacy - zero copay. My civilian friend pays $45 a month. I don’t know how she does it.” - AirForceMom2023, Reddit
- “Waited three days for my generic diabetes drug to be approved. Frustrating, but it worked. Worth it.” - Army Veteran, Military OneSource
- “I had to pay $48 out of pocket because my local pharmacy wasn’t in-network. Never again. Now I use home delivery.” - Navy Spouse, TRICARE.mil review
The 2025 TRICARE Beneficiary Survey showed 86% satisfaction with generic access. But among retirees over 65, 39% are unhappy about the weight loss drug exclusion. That’s a real pain point.
What’s Changing in 2026
The big news: TRICARE Home Delivery’s generic copay jumps from $13 to $14 on January 1, 2026. That’s the first increase since 2023. Retail stays at $16. Military pharmacies remain free.Other changes coming:
- Real-time benefit tools - By Q3 2026, your doctor’s EHR will show you the exact cost and coverage of a drug before prescribing it.
- Step therapy expansion - You’ll be required to try cheaper generics first for 15 more drug classes (like asthma and depression meds).
- Pharmacogenomic testing - By 2028, TRICARE may test your genes before prescribing certain meds to avoid bad reactions.
These aren’t just tech upgrades - they’re designed to cut waste, prevent errors, and keep costs low. The goal? Keep TRICARE’s generic utilization rate above 94% by 2030.
What You Should Do Right Now
Don’t wait for a problem to find out you’re not covered. Here’s your action plan:- Go to esrx.com/tform and search for every generic you take.
- Write down which pharmacy type gives you the lowest copay for each drug.
- If you’re on maintenance meds, switch to home delivery. Save time and money.
- Know your military pharmacy’s hours. Use it whenever you can - it’s free.
- Call the TRICARE Pharmacy Helpline (1-877-363-1303) if you’re unsure. They handled 1.2 million calls in 2025 - they’ve heard it all.
TRICARE’s generic coverage is one of its strongest features. It’s not perfect - there are delays, exclusions, and paperwork. But for most people, it’s the most affordable, reliable prescription system available to military families. Use it right, and you’ll save hundreds - maybe thousands - every year.


Declan O Reilly
December 2, 2025 AT 10:01Man, I wish my civilian friends knew how lucky we are. Zero copay at the base pharmacy? That’s not healthcare, that’s a damn gift.
My brother-in-law pays $80 a month for the same generic blood pressure med. I just walk in, grab it, and leave. No receipts, no stress.
TRICARE’s not perfect, but this part? This part’s gold.
Conor Forde
December 3, 2025 AT 18:14Let’s be real - TRICARE’s ‘free’ pharmacy is just the military’s way of saying ‘you’re not allowed to be sick unless you’re convenient.’
They’ll give you lisinopril for free but deny you semaglutide because some bureaucrat in D.C. decided obesity isn’t a ‘combat-readiness issue.’
Meanwhile, my cousin in Canada gets Ozempic on the NHS. We’re the ones holding the bag while the Pentagon writes poetry about ‘cost efficiency.’
And don’t get me started on the 72-hour approval lag for generics that’ve been on the market since 2012.
It’s not healthcare. It’s a loyalty test.
patrick sui
December 4, 2025 AT 06:05Just wanted to add - if you’re on TRICARE Select and use a non-network pharmacy, you’re basically gambling with your wallet.
That $48 or 20% rule? It’s a trap. I learned the hard way when I grabbed my metformin at Rite Aid.
Pro tip: Use the formulary tool BEFORE you even see your doc. It’s like a cheat code for savings.
Also, home delivery is a game-changer for maintenance meds. No more rushing to the pharmacy at 8 PM because you ran out.
And yes, the $14 copay in 2026 is a bump, but still cheaper than most HMOs.
Stay informed, stay proactive 🙌
Sean McCarthy
December 5, 2025 AT 05:15Bee Floyd
December 5, 2025 AT 14:51My dad’s a retiree. He switched to home delivery after paying $48 out of pocket at CVS. Now he gets his meds every 90 days, no hassle.
He still complains about the weight loss drug exclusion - says he’s not trying to lose weight, he’s trying to stay alive.
But overall? He says it’s the best prescription plan he’s ever had.
Just don’t forget to check the formulary. I’ve seen too many people assume ‘generic = covered.’ It’s not that simple.
Small step, big savings.
Jeremy Butler
December 5, 2025 AT 23:03It is an incontrovertible fact that the structural efficiency of TRICARE’s pharmaceutical tiering system represents a paradigmatic departure from the profit-driven model endemic to commercial insurance.
By prioritizing cost-effectiveness without compromising therapeutic equivalence, the Department of Defense has, in effect, engineered a public good that operates outside the logic of market commodification.
One must acknowledge, however, that the administrative latency inherent in prior authorization protocols remains a non-trivial impediment to patient autonomy.
Nevertheless, the absence of a deductible for military pharmacy utilization constitutes a de facto subsidy of monumental magnitude.
It is not hyperbolic to assert that this framework constitutes one of the most equitable healthcare provisions in the modern American state.
Courtney Co
December 7, 2025 AT 02:20Okay but why do they make it so hard?? I had to wait 5 days for my husband’s generic antidepressant and he almost skipped a week because he was too stressed.
And then when we called, the lady on the phone said ‘Oh, that’s a tier 2 generic’ like that was normal.
My cousin’s insurance just gives it to her. No forms. No waiting. No ‘let me check the formulary.’
And now they’re raising the home delivery price? Like, seriously?
Who’s making these decisions? Are they even taking their own meds?
I just want to cry every time I have to fight for a pill.
Shashank Vira
December 7, 2025 AT 14:13Let us not be fooled by the veneer of affordability.
TRICARE’s ‘generics’ are merely the pharmaceutical industry’s low-hanging fruit - the same molecules, repackaged, with the same profit margins, just hidden behind bureaucratic curtains.
The real innovation? The system’s ability to make you feel grateful for a privilege that should be a right.
Meanwhile, in Germany, generics are automatically dispensed - no formulary checks, no tiered nonsense.
And here we are, celebrating $0 copays like it’s a miracle.
It’s not generosity. It’s control dressed as care.
Eric Vlach
December 8, 2025 AT 17:30Home delivery is the real MVP
Got my blood pressure med delivered last week - $13, no trip, no waiting
My buddy at work pays $22 at Walmart and still has to drive 20 mins
Just use the formulary tool - it’s free and works great
And yeah, the $14 in 2026 sucks but still better than most
Also military pharmacy is free like actually free
Don’t let anyone tell you otherwise
Jack Arscott
December 9, 2025 AT 03:50