More than 500 million adults worldwide live with type 2 diabetes. In the UK alone, over 4.3 million people have been diagnosed, and an estimated 1 million more don’t know they have it. This isn’t just a condition that affects older people anymore. Teens, young adults, and even children are being diagnosed at rising rates. The good news? You can take control of it - if you know what to look for and what to do next.
What Are the Real Signs You Might Have Type 2 Diabetes?
Many people think type 2 diabetes comes with sudden, dramatic symptoms. It doesn’t. Most of the time, it creeps in slowly. You might feel tired all the time, drink more water than usual, or notice you’re peeing more often - especially at night. These signs are easy to brush off as stress, aging, or just getting older.
But here’s what’s happening inside your body: your cells aren’t responding to insulin the way they should. That’s called insulin resistance. Your pancreas tries to keep up by pumping out more insulin. But over time, it gets worn out. Blood sugar starts to climb. And that’s when symptoms become harder to ignore.
The most common signs include:
- Constant thirst - even after drinking
- Frequent urination - especially at night
- Feeling hungry all the time, even after eating
- Unexplained weight loss - despite eating normally
- Extreme fatigue - not just from lack of sleep
- Blurred vision - that comes and goes
- Slow-healing cuts or sores
- Recurrent infections - like yeast infections or urinary tract infections
- Tingling or numbness in hands or feet
Some people notice dark, velvety patches on their neck, armpits, or groin. That’s called acanthosis nigricans. It’s a visible sign of insulin resistance. And while it’s not dangerous on its own, it’s a red flag your body is struggling to manage blood sugar.
Here’s the hard truth: 1 in 4 people with type 2 diabetes have no symptoms at all. That’s why routine blood tests matter. If you’re over 40, overweight, or have a family history, ask your doctor for a simple fasting glucose or HbA1c test. It takes five minutes. It could save your life.
Why Did This Happen to Me? The Real Causes Behind Type 2 Diabetes
It’s not your fault. But it’s not just genetics either. Type 2 diabetes is the result of a mix of things you can change - and things you can’t.
Genetics play a big role. If one of your parents has type 2 diabetes, your risk goes up by 40%. If both have it, your risk jumps even higher. Certain ethnic groups - including Black, South Asian, and Hispanic populations - are more likely to develop it, even at lower body weights.
But the biggest driver? Weight. Specifically, excess fat around the abdomen. Fat in the wrong place releases chemicals that block insulin from working. People with a BMI over 30 are 80 times more likely to develop type 2 diabetes than those with a BMI under 22. That’s not a small risk. That’s a massive one.
And it’s not just about being overweight. Being inactive is just as dangerous. The World Health Organization says physical inactivity contributes to nearly 1 in 4 cases of type 2 diabetes. Sitting for long hours - whether at a desk, in a car, or on the couch - slows down how your body uses sugar.
Age matters too. After 45, your risk increases. But now, kids as young as 10 are being diagnosed. Why? Because processed foods, sugary drinks, and sedentary lifestyles have become normal. The CDC reports over 287,000 Americans under 20 have type 2 diabetes. That number is rising fast.
Stress and sleep also play roles. Chronic stress raises cortisol, which raises blood sugar. Poor sleep messes with hunger hormones and insulin sensitivity. It’s not just diet and exercise. It’s your whole life.
What Happens If You Ignore It?
High blood sugar doesn’t just make you tired. It quietly damages your body over years.
Your heart and blood vessels are the first to suffer. People with type 2 diabetes are 2 to 4 times more likely to have a heart attack or stroke. That’s why heart disease causes 65-80% of deaths in people with diabetes.
Your nerves start to die. This is called neuropathy. It starts with tingling in your feet. Then numbness. Then pain. And if you can’t feel a cut or blister? It can turn into an ulcer. One in five people with neuropathy will develop a foot ulcer. And one in five of those will need an amputation.
Your kidneys get damaged. Diabetes is the leading cause of kidney failure. One in three people with type 2 diabetes will develop kidney disease. That means dialysis or a transplant down the line.
Your eyes are at risk too. Diabetic retinopathy affects nearly 30% of people with diabetes. It can lead to blindness. In the US alone, it causes 17,000 new cases of vision loss every year.
And your brain? Studies show people with type 2 diabetes have a 2 to 3 times higher risk of Alzheimer’s. Some scientists now call it “type 3 diabetes.”
Then there’s mental health. Depression is twice as common in people with diabetes. And it makes managing the condition harder - creating a cycle that’s tough to break.
This isn’t fearmongering. It’s facts. But here’s the flip side: you can stop most of this.

How to Actually Manage Type 2 Diabetes - Not Just Treat It
Managing type 2 diabetes isn’t about taking a pill and calling it done. It’s about changing how you live.
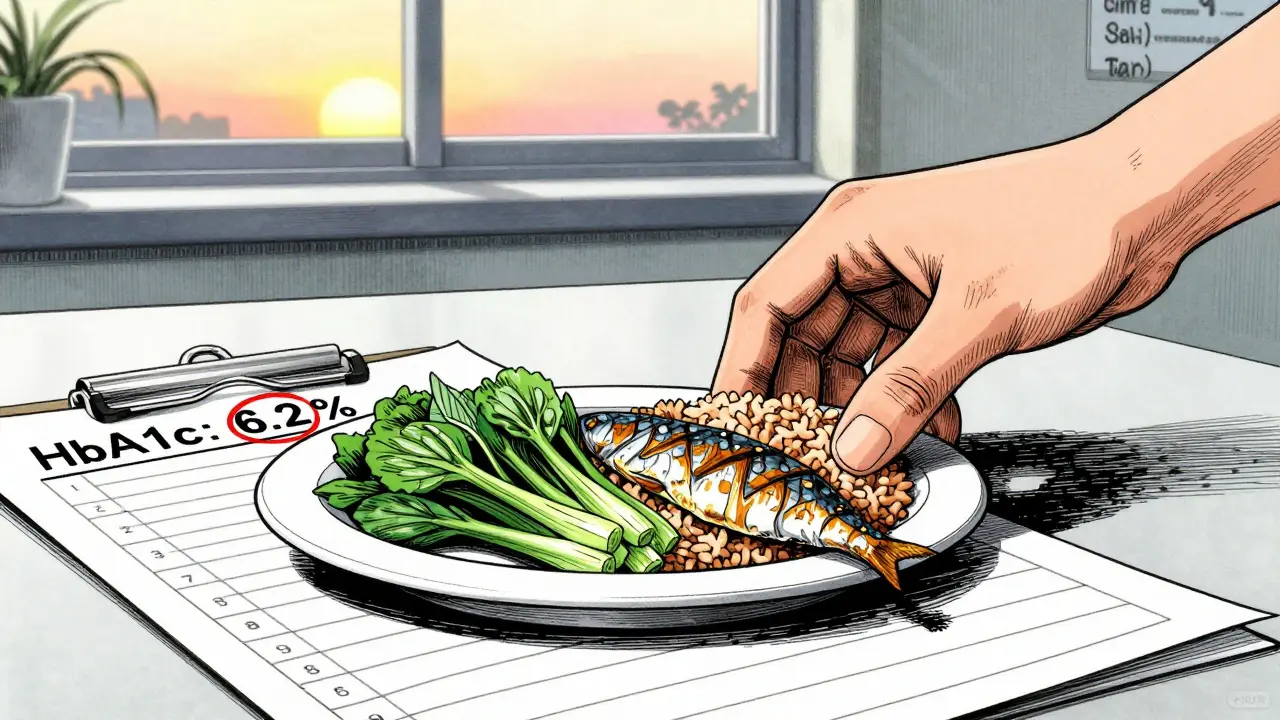
The first step? Know your numbers. HbA1c is your 3-month average blood sugar. Most doctors aim for under 7%. But for some, 6.5% is safe. For others - especially older adults - 8% might be better. Talk to your doctor. Don’t just accept a number. Understand why it’s right for you.
Medication is often part of the plan. Metformin is the first-line drug. It’s cheap, safe, and reduces HbA1c by 1-2%. It doesn’t cause weight gain or low blood sugar. Many people stay on it for life.
But newer drugs are changing the game. GLP-1 agonists like semaglutide (Ozempic, Wegovy) and SGLT2 inhibitors like empagliflozin (Jardiance) don’t just lower blood sugar. They protect your heart and kidneys. They also help you lose weight - 3 to 15 pounds on average. These aren’t just pills. They’re tools for long-term health.
But the most powerful treatment? Lifestyle. Not “eating better.” Not “exercising more.” Real, structured change.
The CDC’s National Diabetes Prevention Program proved something simple: lose 7% of your body weight, move 150 minutes a week, and you cut your risk of diabetes by 58%. That’s not a miracle. That’s math.
One of the most surprising breakthroughs? Remission. The DIALECT trial showed that nearly half of people with type 2 diabetes for less than 6 years went into remission after a strict 800-calorie diet for 3-5 months, followed by gradual food reintroduction. No surgery. No drugs. Just food. And it worked.
You don’t need to be perfect. You just need to be consistent. A 10-minute walk after dinner. Swapping soda for sparkling water. Taking the stairs. These small things add up.
Technology Is Changing Everything - And You Can Use It
Remember when checking blood sugar meant pricking your finger five times a day? Now, continuous glucose monitors (CGMs) track your sugar 24/7. They show you how food, sleep, stress, and movement affect your levels in real time.
Since 2017, Medicare coverage for CGMs in type 2 diabetes has jumped from 1.2% to 12.7% of users. That’s not just tech. That’s access. And it’s working. People using CGMs spend more time in the healthy blood sugar range - 71% vs. 51% without them.
Hybrid closed-loop systems - sometimes called “artificial pancreases” - now work for type 2 diabetes too. The MiniMed 780G, approved in 2022, automatically adjusts insulin based on your glucose levels. It’s not a cure. But it takes the guesswork out of management.
Apps help too. MyFitnessPal, Glucose Buddy, and even Apple Health can track patterns. You don’t need fancy gear. Just a phone, a log, and a willingness to see what’s really happening.
What’s Next? Hope Is Real
Type 2 diabetes is not a death sentence. It’s a signal. A sign your body needs help - and you have the power to give it.
Early action changes everything. The UKPDS study showed that tight control in the first few years gives you protection that lasts decades. That’s called the “legacy effect.” It means the choices you make now echo for years.
And the science is moving fast. New drugs, better monitoring, smarter diets - we’re not stuck. We’re evolving.
Don’t wait for symptoms to get worse. Don’t wait for a crisis. If you’re at risk - overweight, inactive, over 40, or have a family history - get tested. Talk to your doctor. Start small. Walk more. Drink less sugar. Sleep better. These aren’t just tips. They’re medicine.
And if you already have it? You’re not broken. You’re learning. And every choice you make today - what you eat, how you move, how you sleep - is a step toward a longer, healthier life.
Can type 2 diabetes be reversed?
Yes - in some cases. Research shows that people with type 2 diabetes who lose significant weight - often through a very low-calorie diet - can return blood sugar to normal without medication. This is called remission. It’s most likely if you’ve had diabetes for less than 6 years and act early. It’s not a cure, but it means you no longer need drugs to manage it. Lifestyle changes must continue to keep it from coming back.
Do I need to take insulin for type 2 diabetes?
Not always. Most people start with metformin and lifestyle changes. Over time, as the pancreas loses its ability to make insulin, some people do need insulin - especially after 10-15 years. But many never do. Newer medications like GLP-1 agonists and SGLT2 inhibitors help lower blood sugar without insulin. The goal is to delay or avoid insulin if possible, but if it’s needed, it’s not a failure. It’s just the next step in care.
Can I still eat carbs with type 2 diabetes?
Yes - but not all carbs are equal. Avoid sugary drinks, white bread, pastries, and processed snacks. These spike blood sugar fast. Instead, choose whole grains, beans, lentils, vegetables, and fruit. Portion matters. A small serving of brown rice or quinoa is fine. Pair it with protein or fat to slow digestion. Monitoring your blood sugar after meals helps you learn what works for you.
How often should I check my blood sugar?
It depends. If you’re on insulin or have trouble controlling your levels, your doctor may ask you to check daily. If you’re managing with diet and metformin, checking a few times a week - or even just once a week - may be enough. HbA1c tests every 3 to 6 months give you the big picture. Continuous glucose monitors (CGMs) are becoming more common and reduce the need for finger pricks. Talk to your healthcare team to find the right plan for you.
Is type 2 diabetes hereditary?
Yes, genetics play a role. If a parent or sibling has type 2 diabetes, your risk is about 40% higher. But genes aren’t destiny. Even with a strong family history, you can delay or prevent it by staying active, eating well, and keeping a healthy weight. Many people with a genetic risk never develop diabetes because they manage their lifestyle.
Can stress make type 2 diabetes worse?
Absolutely. Stress triggers hormones like cortisol and adrenaline, which raise blood sugar. Chronic stress also leads to poor sleep, emotional eating, and skipping exercise - all of which make diabetes harder to control. Managing stress through walking, meditation, therapy, or hobbies isn’t optional. It’s part of treatment.
What’s the best diet for type 2 diabetes?
There’s no single “best” diet. But the most effective ones focus on whole foods: vegetables, lean proteins, healthy fats, and complex carbs. Mediterranean, DASH, and low-carb diets all show good results. The key is reducing sugar, refined grains, and ultra-processed foods. Portion control and timing matter too. Eating regularly helps avoid blood sugar spikes and crashes. Find a pattern you can stick to - not a short-term fix.
Can I drink alcohol with type 2 diabetes?
Yes - in moderation. Alcohol can lower blood sugar, especially if you’re on insulin or certain pills. Drink with food. Limit to one drink per day for women, two for men. Avoid sugary mixers like soda or juice. Choose dry wine, light beer, or spirits with soda water. Always check your blood sugar before bed if you drink, as low sugar can happen hours later.
What Should You Do Today?
Here’s your simple plan:
- If you haven’t been tested and you’re over 40, overweight, or have a family history - ask your doctor for an HbA1c test.
- If you’ve been diagnosed, don’t panic. Start with one change: walk 15 minutes after dinner every day.
- Swap one sugary drink a day for water, tea, or sparkling water.
- Get your feet checked at your next doctor visit.
- Write down your blood sugar readings if you’re testing - even if it’s just once a week.
You don’t need to fix everything at once. You just need to start. And you’re not alone. Millions are doing the same thing - one step, one meal, one day at a time.


Jenci Spradlin
January 10, 2026 AT 12:12man i got diagnosed last year and honestly i didnt even know what was going on. just kept being tired, peeing every hour, and eating like a horse but still losing weight. my doc was like 'bro you're diabetic' and i was like 'wait, i dont even drink soda that much?' lol. turned out it was the bagels and donuts for breakfast every day. changed to eggs and spinach and my energy's way better now.
Elisha Muwanga
January 10, 2026 AT 15:03It is utterly irresponsible to suggest that type 2 diabetes can be 'managed' without strict adherence to medical protocol. The normalization of lifestyle 'hacks' undermines decades of clinical research. This article reads like a wellness blog masquerading as public health guidance.
Catherine Scutt
January 12, 2026 AT 08:23so many people think it's just 'eat less sugar' and boom you're fixed. no. it's not that simple. i had acanthosis nigricans for years before anyone told me what it was. my doctor just said 'you're overweight' like it was a personality flaw. it's not. it's biology. and yeah, it sucks.
Darren McGuff
January 13, 2026 AT 09:47I've been living with this for 12 years now. Started on metformin, then added a GLP-1 agonist. Lost 47 pounds. My HbA1c dropped from 9.1 to 5.8. But here's the thing-no one talks about the emotional toll. The guilt. The shame when you slip up and eat pizza. It’s not just a disease. It’s a full-time job. And you’re not alone in feeling tired of it.
Alicia Hasö
January 14, 2026 AT 08:56You are not broken. You are not lazy. You are not failing. You are learning how your body works-and that’s a superpower. Every walk after dinner, every swap of soda for sparkling water, every time you choose to check your numbers-that’s courage. You’re doing better than you think. Keep going. One meal. One step. One day at a time. You’ve got this.
Aron Veldhuizen
January 15, 2026 AT 00:14Let’s be honest: the entire narrative around type 2 diabetes is a capitalist construct. If it were truly about health, we wouldn’t be selling $1,000 CGMs and $1,200 monthly GLP-1 drugs. The real solution? Stop eating processed food. But corporations profit from your ignorance. So they market 'management' instead of prevention. The system doesn’t want you cured. It wants you subscribed.
Micheal Murdoch
January 15, 2026 AT 06:02It’s funny how we treat diabetes like it’s a moral failure. Like if you just had more willpower, you wouldn’t have it. But the body doesn’t care about willpower. It cares about insulin resistance, fat distribution, chronic stress, sleep deprivation. We’ve turned a biological condition into a personal failing. That’s not just wrong-it’s cruel. Healing starts when we stop blaming and start understanding.
Ian Long
January 16, 2026 AT 12:32I used to think the keto diet was the only way. Then I tried Mediterranean. Then I tried low-carb, then plant-based. Turns out none of them ‘worked’ for me-until I stopped chasing diets and started listening to my body. My numbers improved when I stopped obsessing over macros and started eating slowly, sleeping better, and walking with my dog. Sometimes the answer isn’t more discipline. It’s less pressure.
Johanna Baxter
January 17, 2026 AT 21:41i hate how everyone acts like this is some inspirational journey. it’s not. it’s exhausting. i have to check my sugar before i kiss my kid. before i go to bed. before i drive. before i eat a damn apple. i’m tired of being the person who can’t have dessert. i’m tired of feeling guilty. i’m tired of being told i ‘could’ve prevented it’ like i just didn’t try hard enough.
Jerian Lewis
January 18, 2026 AT 13:08People who say it’s reversible are lying to themselves. Once your pancreas is worn out, it’s done. No 800-calorie diet is gonna bring it back. You might get numbers down, but the damage is permanent. Don’t give false hope. Be honest. This is a chronic condition. Deal with it.
Kiruthiga Udayakumar
January 20, 2026 AT 11:35in india we have so many people with type 2 diabetes now because of all the packaged snacks and sugary tea. my aunt had it and she just ate rice with ghee every day and said 'it's tradition'. now she's on insulin. we need to change the culture, not just the diet.
Patty Walters
January 21, 2026 AT 06:26just started using a cgm last month and it changed everything. i had no idea my blood sugar spiked after eating oatmeal. or that a 10-minute walk after dinner brought it back down. i thought i was eating healthy. turns out i was just eating the *wrong* healthy stuff. this tech is a game changer. no more guessing.
Phil Kemling
January 23, 2026 AT 06:06If we accept that type 2 diabetes is a consequence of modern life-sedentary work, processed food, chronic stress, sleep debt-then calling it a 'personal failure' is like blaming a fish for drowning in polluted water. The system is broken. The individual is just swimming in it. Maybe the real question isn't 'how do I fix myself?' but 'how do we fix the environment that made this inevitable?'