Every time you pick up a prescription or grab a bottle of painkillers from the shelf, you’re holding a document that could save your life-or hurt you if you don’t know how to read it. Drug labels aren’t just stickers with names and numbers. They’re packed with critical information designed to keep you safe. But here’s the problem: most people don’t understand them.
A 2022 survey of over 1,200 patients found that nearly 7 out of 10 struggled to make sense of their prescription labels. One in four admitted they’d taken medicine the wrong way because they didn’t get what the label said. That’s not just inconvenient-it’s dangerous. Medication errors contribute to around 7,000 deaths in the U.S. every year. And it’s not because people are careless. It’s because the labels themselves are confusing, cluttered, and written for doctors, not patients.
What’s Actually on a Prescription Label?
If you’ve ever stared at a pharmacy label like it’s a cryptic code, you’re not alone. Prescription labels follow a strict format set by the FDA, but that doesn’t make them easy to read. Here’s what you’ll typically find:
- Patient name - Always double-check this. Mixing up names is one of the most common errors.
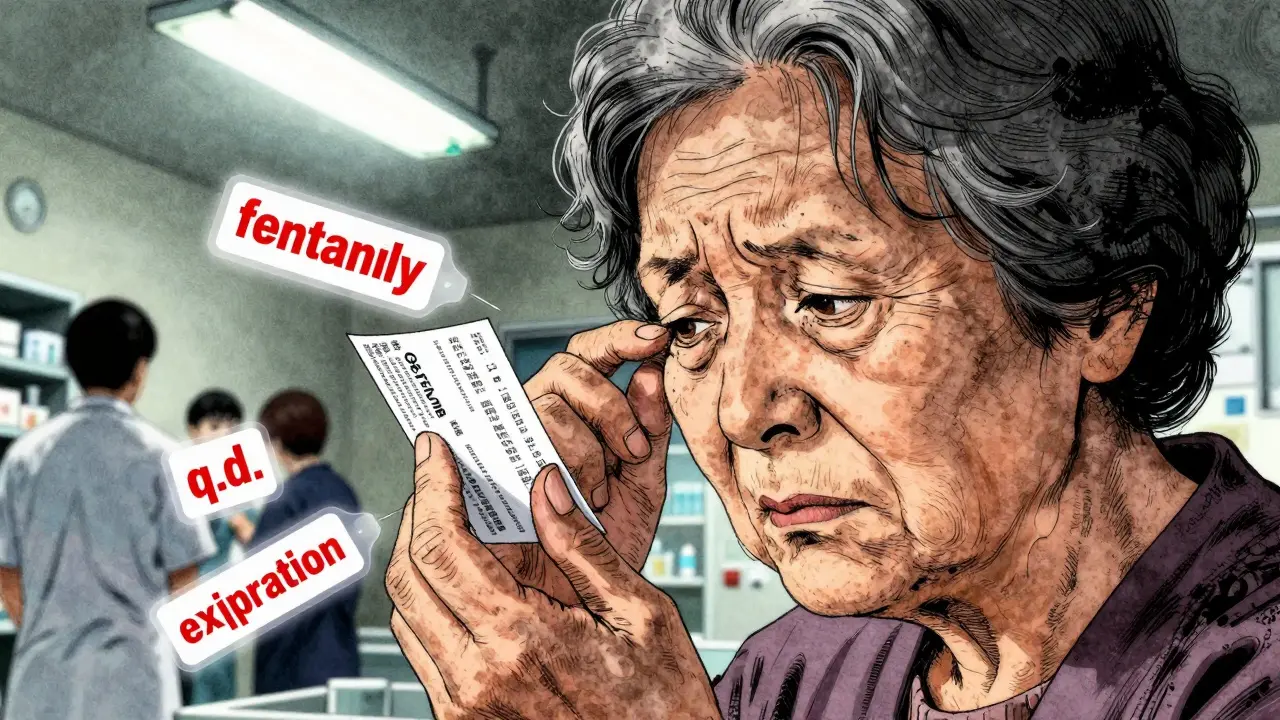
- Medication name - This includes both the brand name (like Abstral) and the generic name (like fentanyl). The generic name is the active ingredient-the part that actually does the work.
- Strength and dosage form - You’ll see something like “100 micrograms per tablet” or “500 mg capsule.” Don’t confuse strength with dose. Strength is how much medicine is in each pill. Dose is how many you take.
- Directions - These tell you how often and how to take it. Watch out for abbreviations like “q.d.” (once daily) or “b.i.d.” (twice daily). Many people misread these. Always ask if you’re unsure.
- Dispensing date and pharmacy info - This helps track your medication history and gives you a way to call if something’s wrong.
- Expiration date - Medications lose effectiveness over time. Taking expired pills can be risky, especially for antibiotics or heart meds.
- Refill info - How many times you can get it refilled without a new prescription.
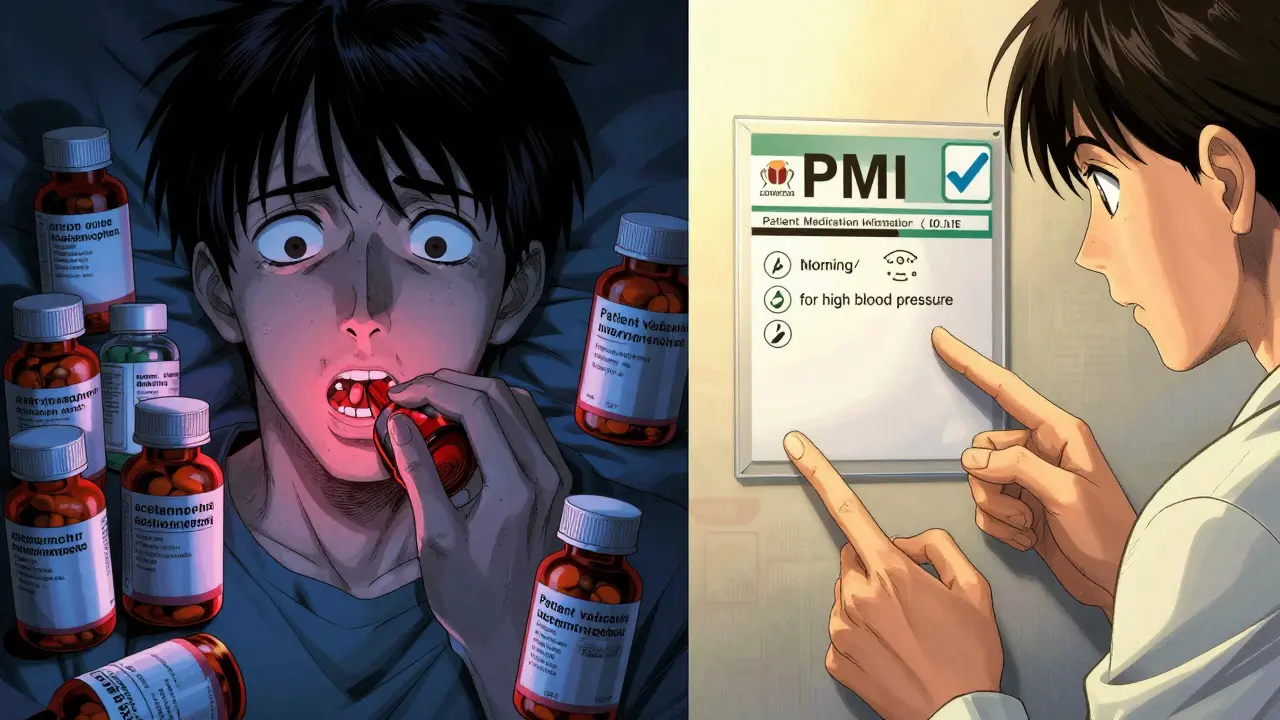
But here’s what’s missing: why you’re taking it. Most labels don’t say whether the pill is for high blood pressure, anxiety, or infection. That’s a huge gap. A University of Florida study found that when labels included the reason for use-like “for high blood pressure”-medication errors dropped by 42%.
Over-the-Counter Labels: Simpler, But Still Tricky
OTC meds like Tylenol, Advil, or cough syrup follow a different format called the “Drug Facts” label. It’s designed for you, not a doctor. Here’s how it breaks down:
- Active ingredient - This is the medicine itself. For example, acetaminophen in Tylenol. Always check this to avoid taking too much of the same drug from different products.
- Purpose - What the ingredient does. “Pain reliever,” “fever reducer,” “antihistamine.”
- Uses - Symptoms it treats: headache, runny nose, sore throat.
- Warnings - When NOT to take it. This includes allergies, other meds you’re on, pregnancy, and conditions like liver disease.
- Directions - How much and how often. Pay attention to “do not exceed” limits.
- Inactive ingredients - Fillers, dyes, flavors. Important if you have allergies or sensitivities.
- Other information - Storage tips, like “keep refrigerated” or “protect from light.”
Even with this clearer format, mistakes happen. People take multiple cold medicines thinking they’re different, not realizing they all contain acetaminophen. That’s how liver damage happens. Always check the active ingredient list.
Why Labels Are So Hard to Understand
The FDA’s labeling rules were built for doctors, not patients. The full prescribing information for a drug can be 50 pages long, filled with medical jargon, clinical trial data, and statistical terms. It’s meant to inform healthcare providers, not help someone with low health literacy understand why they’re taking a pill.
Patients aren’t the only ones confused. Nurses and pharmacists say they struggle too. One nurse with 12 years of experience posted on Reddit: “I still have trouble quickly finding the dose on some labels.” That’s alarming. If trained professionals can’t read them easily, what chance does an elderly person with poor eyesight have?
Older adults are especially at risk. A 2022 Medicare report found that 54% of beneficiaries over 65 had trouble reading small print on labels. That’s linked to a 22% higher chance of medication errors. And it’s not just about size. Abbreviations like “q.i.d.” (four times a day) or “p.r.n.” (as needed) are still common. The Institute for Safe Medication Practices says these kinds of abbreviations cause about 15% of labeling-related errors.
Even drug names can trip you up. Hydroxyzine and hydralazine sound alike but do completely different things. One’s for anxiety, the other for high blood pressure. That’s why some pharmacies use “tall man lettering”-writing similar names with uppercase letters to highlight differences, like predniSONE vs. predniSOLONE.
What You Can Do to Stay Safe
You don’t have to be a pharmacist to understand your meds. Here’s how to take control:
- Ask for the reason - When your doctor gives you a prescription, ask: “Why am I taking this?” Write it down. If the label doesn’t say it, ask your pharmacist to add it.
- Read the label every time - Don’t assume it’s the same as last time. Strengths, dosages, and instructions can change.
- Use a pill organizer - Especially if you take multiple meds. Label each compartment with the day and time.
- Ask your pharmacist to explain - Pharmacists are trained to translate label jargon into plain language. A 2021 study showed that when pharmacists explained labels to patients with low health literacy, medication errors dropped by 29%.
- Check for interactions - Tell your pharmacist everything you’re taking-even vitamins, herbs, or OTC drugs. Some combinations can be dangerous.
- Use a magnifying glass or phone zoom - If the print is too small, don’t guess. Use technology to help.

The Future of Drug Labels: Better, Clearer, Patient-Focused
Change is coming. The FDA is working on something called Patient Medication Information (PMI)-a one-page, standardized summary that replaces the current dense prescribing info with plain-language instructions. Think of it like a nutrition label for medicine: simple, visual, and easy to scan.
By 2026, the first PMI templates will roll out for high-risk medications like blood thinners, insulin, and chemotherapy drugs. These will include:
- Why you’re taking it
- How to take it (with icons for times of day)
- What to avoid
- When to call your doctor
- Storage and disposal instructions
Some pharmacies are already ahead of the curve. A 2022 survey found that 63% of independent pharmacies have added patient-centered features like larger fonts, color coding, or written reasons for use. Chain pharmacies lag behind, with only 41% making similar changes.
And it’s not just labels. The FDA also requires Instructions for Use (IFU) for complex medications-like inhalers or injectables. These come with step-by-step pictures showing how to use the device. No more guessing how to prime a pen or spray into your nose.
Don’t Guess. Ask.
Medication labels are meant to protect you. But they only work if you understand them. If something on your label doesn’t make sense-say it out loud. Call your pharmacist. Ask your doctor. Write it down. Don’t assume you’ll remember later. And don’t be embarrassed. Even experts get tripped up.
The goal isn’t to turn everyone into a pharmacologist. It’s to make sure you can take your medicine safely, without fear, confusion, or risk. The system is changing. But until it’s fully updated, your best tool is still your voice. Speak up. Ask questions. Read the label. Your health depends on it.
What’s the difference between brand name and generic name on a drug label?
The brand name is what the company calls the drug, like Abstral. The generic name is the actual medicine, like fentanyl. All versions of a drug-brand or generic-contain the same active ingredient. Generic versions are cheaper and just as effective. Always check the generic name to avoid accidentally taking two of the same drug.
Why don’t prescription labels say why I’m taking the medicine?
Current FDA rules don’t require it. Labels are designed for doctors, not patients. But research shows adding the reason-like “for high blood pressure”-reduces errors by 42%. Many pharmacies now add it manually, and the FDA is working on making it standard by 2026 through the new Patient Medication Information format.
Can I take medicine after the expiration date?
It’s not recommended. Some medications, like antibiotics or insulin, can lose effectiveness or even become harmful after expiration. For most OTC pain relievers, they may just be less potent. But with serious conditions, you can’t risk it. If in doubt, dispose of it properly and get a new prescription.
What should I do if my label looks wrong?
Don’t take it. Call the pharmacy immediately. Check your name, the drug name, dosage, and instructions. If something doesn’t match what your doctor told you, it could be a mistake. Pharmacies make errors too-about 1 in 100 prescriptions has an issue. Catching it early can prevent serious harm.
Are there tools to help me understand my labels better?
Yes. Many pharmacies offer free counseling. Apps like Medisafe or MyTherapy let you scan barcodes to get plain-language explanations. The FDA also provides free Medication Guides for high-risk drugs-ask your pharmacist for one. And don’t forget: your pharmacist is there to help. Use them.

Bobbi Van Riet
January 31, 2026 AT 09:13I used to ignore labels until my grandma almost overdosed on ibuprofen because she thought 'take as needed' meant every hour. Now I read every single line, even if my eyes glaze over. I keep a little notebook next to my pill organizer with the reason for each med, written in big marker. My pharmacist even started doing it for me now-she says she wishes more people asked. It’s not just about safety, it’s about dignity. You shouldn’t have to be a detective just to take your own medicine.
And yeah, the font size? Criminal. My mom’s 78 and squints like she’s decoding a spy message. I zoom in on my phone just to read the 'take with food' part. Why can’t they print like normal humans do?
I’m not saying the FDA’s lazy-but they’re clearly not living in the real world. If I had to read a label like that after a 12-hour shift or while half-asleep, I’d mess it up too. This isn’t rocket science. It’s basic human design.
Also, if your label says 'q.i.d.' and you don’t know what that means? Just ask. No shame. I’ve asked a hundred times. Every time, the pharmacist smiles and says, 'Good for you.' That’s the culture we need to build.
And please, for the love of all things holy, don’t mix cold meds. I once took three different NyQuil variants because I thought 'Nighttime Cold & Flu' and 'Nighttime Severe Cold' were different. Turns out they were both loaded with acetaminophen. I spent a night in the ER with liver enzymes higher than my anxiety levels. Don’t be me.
TL;DR: Ask. Write it down. Use your phone. Your body will thank you.
Holly Robin
February 1, 2026 AT 15:48OMG I KNEW IT. THIS IS ALL A PHARMA CONSPIRACY. THEY WANT YOU TO BE CONFUSED SO YOU’LL KEEP BUYING NEW MEDS AND NEVER QUESTION IT. THE FDA IS IN THEIR POCKET. THEY USE ‘Q.D.’ AND ‘P.R.N.’ ON PURPOSE BECAUSE THEY KNOW OLD PEOPLE CAN’T READ IT AND WILL JUST TAKE MORE ‘JUST IN CASE.’ I SAW A DOC ON YOUTUBE WHO SAID THE SAME THING-THEY EVEN USE SIMILAR-SOUNDING DRUG NAMES TO TRICK YOU INTO MISTAKES. IT’S NOT AN ACCIDENT. IT’S A BUSINESS MODEL.
AND WHY DO THEY PUT THE EXPIRATION DATE SO SMALL? SO YOU’LL THINK IT’S STILL GOOD AND KEEP TAKING IT. I THREW OUT ALL MY ANTIBIOTICS LAST YEAR BECAUSE I DIDN’T TRUST THE LABEL. NOW I JUST USE OREGANO OIL AND VIBRATIONAL HEALING. IT WORKS BETTER ANYWAY.
AND DON’T EVEN GET ME STARTED ON ‘GENERIC’ DRUGS. THEY’RE JUST PLACEBOS WITH DIFFERENT COLORS. THE REAL STUFF IS ONLY IN THE BRAND NAME. THEY’RE LYING TO YOU.
IF YOU’RE NOT TAKING A MIRACLE CURE FROM A GUY ON INSTAGRAM, YOU’RE BEING MANIPULATED. STAY WAKE.
Amy Insalaco
February 2, 2026 AT 23:33It’s not that the labels are confusing-it’s that the patient population has been systematically de-skilled through decades of consumerist healthcare. The FDA’s format is functionally adequate; it’s the cultural incompetence of the populace that renders it opaque. The fact that 70% of patients can’t parse ‘b.i.d.’ speaks less to poor design and more to the erosion of basic literacy and scientific reasoning in public education.
Moreover, the notion that ‘why you’re taking it’ should be printed on the label is a dangerous precedent. That’s clinical context, not regulatory obligation. If patients need to know the indication, they should consult their prescriber-not have their label turned into a medical chart. The label’s purpose is to convey dosage, administration, and safety parameters-not therapeutic rationale.
And while we’re at it, ‘tall man lettering’ is a band-aid solution to a systemic problem: the proliferation of look-alike, sound-alike drug names due to pharmaceutical marketing incentives. The real fix is reducing drug proliferation, not redesigning labels to accommodate corporate naming chaos.
Let’s not confuse accessibility with dumbing down. We don’t need a ‘nutrition label’ for medicine-we need a population that understands pharmacology at a foundational level. Otherwise, we’re just building bigger crutches for cognitive laziness.
Beth Beltway
February 4, 2026 AT 22:11You people are naive. You think this is about ‘safety’? It’s about liability. The labels are written in legalese because if you mess up, they don’t get sued. If you read ‘q.d.’ and take it four times, that’s your fault. They’ve covered their asses since the 80s. The FDA doesn’t care if you die-they care if a lawyer can prove they gave you the info.
And don’t get me started on ‘generic’ drugs. You think they’re the same? Try taking a generic Adderall after being on the brand for years. The fillers are different. The absorption profile is different. You think that’s an accident? It’s not. It’s a profit play. The generics are cheaper because they’re not held to the same bioequivalence standards.
And yes, I’ve seen pharmacists make mistakes. I’ve seen them give me the wrong strength because they misread a handwritten script. That’s not the label’s fault. That’s incompetence. Stop blaming the system. Blame the people running it.
Also, ‘ask your pharmacist’? They’re paid by the pharmacy chain. They want you to refill ASAP. They don’t care if you understand it-they care if you leave with a receipt.
Bottom line: You’re on your own. Read the label. Double-check. Don’t trust anyone. Ever.
Marc Bains
February 4, 2026 AT 22:21I’ve worked in community health for over a decade, and let me tell you-this isn’t just about labels. It’s about trust. People don’t ask questions because they’re afraid of looking stupid, or because their doctor rushes them, or because they can’t afford to go back for clarification.
One time, I had an elderly Haitian woman who took her blood pressure med every morning… but she thought it was for her ‘bad stomach’ because the label didn’t say anything else. She’d skip it on days she didn’t feel nauseous. That’s not ignorance-that’s systemic failure.
We started using pictograms: a heart for BP meds, a moon for sleep aids, a sun for morning doses. We printed the reason in Creole and English. Within six months, her adherence went from 30% to 90%.
It’s not about dumbing down. It’s about designing for humans. We don’t need PhDs to take medicine. We need clarity. And if you’re a pharmacist or doctor who thinks ‘just ask’ is enough-you’re part of the problem.
Also, if you’re reading this and you’re young? Don’t wait until your grandma’s in the ER to care. Talk to your elders. Help them read their labels. It’s the most powerful thing you can do.
Healthcare isn’t a privilege. It’s a right. And understanding your meds? That’s the first step.
kate jones
February 4, 2026 AT 23:15While I appreciate the sentiment behind patient-centered labeling, it’s critical to acknowledge that the current FDA-prescribed format adheres to the USP Standard for Prescription Labeling (USP 1782), which mandates specific elements for regulatory compliance and interprofessional communication. The omission of indication is not an oversight-it’s a deliberate limitation to avoid off-label promotion risks under the FDCA.
That said, the emergence of PMI represents a significant evolution in risk communication strategy, aligning with the principles of health literacy and cognitive load theory. The use of iconography for dosing schedules, for instance, reduces reliance on textual comprehension, which is particularly beneficial for non-native English speakers and those with cognitive impairments.
Pharmacies implementing color-coded systems (e.g., red for anticoagulants, blue for CNS agents) are demonstrating operational innovation within existing regulatory frameworks. However, standardization across chain pharmacies remains inconsistent due to variable IT infrastructure and vendor contracts.
It’s also worth noting that the 42% reduction in errors with indication inclusion was observed in controlled, single-center studies. Real-world generalizability requires multivariate analysis controlling for socioeconomic status, health literacy, and polypharmacy burden-factors often underreported in advocacy literature.
Bottom line: The system is imperfect, but incremental, evidence-based reform-not emotional appeals-is the path to sustainable safety.
Sidhanth SY
February 5, 2026 AT 05:06Man, I read this while waiting for my chai at the pharmacy in Delhi. Same thing here-people take two kinds of cough syrup because they both say 'for fever' and don’t realize they both have paracetamol. My aunt once took her diabetes pill with grapefruit juice because the label didn’t say ‘avoid citrus.’ She ended up in the hospital.
But here’s the thing-we don’t have fancy labels or apps. We have the pharmacist standing there, yelling over the noise, explaining in Hindi and English. That’s the real safety net.
Maybe the US needs more people like my uncle who works at the local pharmacy-he draws little pictures on the bottles. A sun for morning, a moon for night, a heart for blood pressure. Simple. Works.
It’s not about tech. It’s about someone caring enough to explain. And honestly? That’s what’s missing everywhere.
Adarsh Uttral
February 5, 2026 AT 06:12lol i just use google lens to scan the label and it tells me what it is. no cap. saved me like 3 times already. also i always screenshot the pic of the pill so i know what it looks like. dumb but works. also dont trust the pharmacy name on the bottle-sometimes they switch generics and you get a different color. check the imprint code. google it. easy.