Airway Inflammation: Causes, Symptoms, and Treatment Options
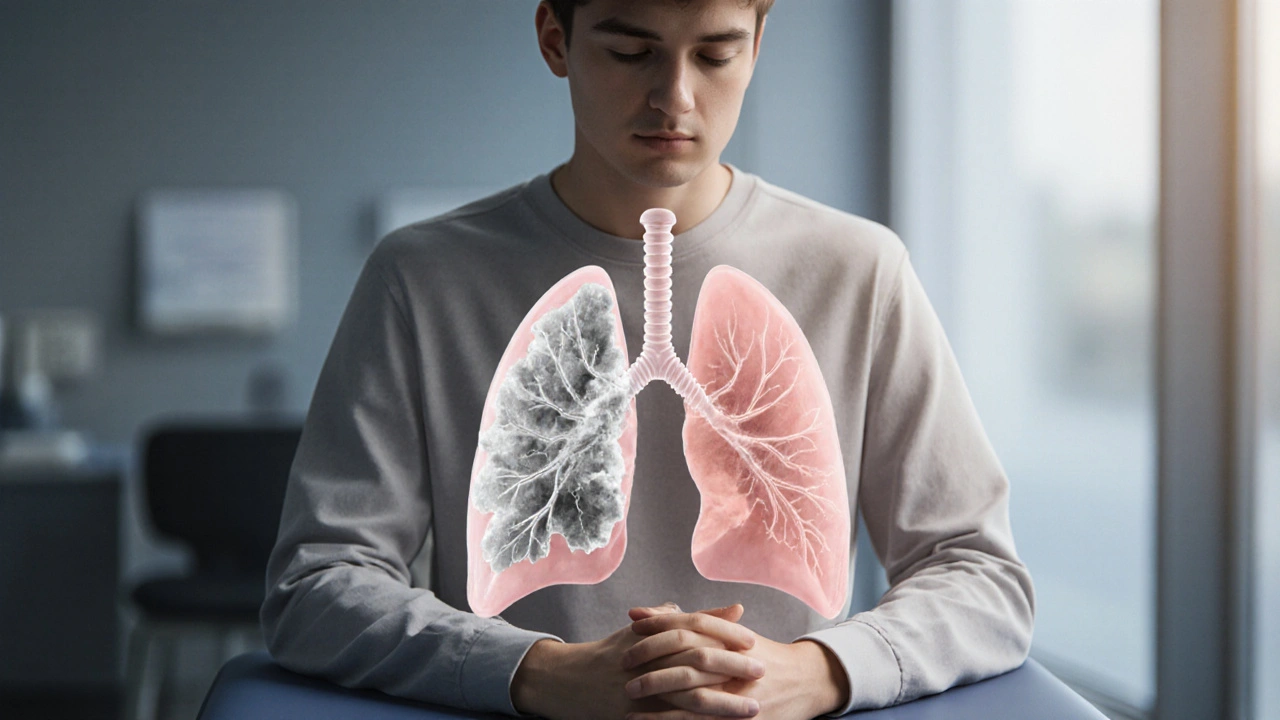
When dealing with airway inflammation, the swelling and irritation of the bronchial tubes that carry air to the lungs. Also known as respiratory tract inflammation, it is the core driver behind conditions such as asthma, a chronic disease marked by reversible airway narrowing and excess mucus and COPD, a progressive blockage of airflow usually caused by long‑term smoking or pollutant exposure. The presence of corticosteroids, powerful anti‑inflammatory drugs that reduce swelling and immune response in the airways often determines whether symptoms stay mild or flare into severe breathlessness. In short, airway inflammation requires an understanding of triggers, influences treatment choices, and connects directly to disease management strategies across respiratory health.
Key Factors Behind Airway Inflammation
First, triggers matter. Allergens like pollen, pet dander, or mold can activate mast cells, releasing histamine that inflames the bronchial lining. Viral infections, especially the common cold or flu, introduce cytokines that further irritate the airway wall. Environmental pollutants—smoke, ozone, particulate matter—act like a constant irritant, making the airway more reactive over time. Each of these factors can initiate or worsen inflammation, turning a simple cough into a chronic condition. Second, the body’s immune response plays a dual role. While it protects against pathogens, an overactive immune system can generate excess mucus and cause smooth‑muscle constriction, hallmark signs of asthma attacks or COPD exacerbations. Third, medication choice directly shapes outcomes. Inhaled corticosteroids (ICS) target the inflammatory cascade at its source, reducing the frequency of flare‑ups. For patients who can’t tolerate steroids, leukotriene modifiers or biologics such as anti‑IL‑5 agents provide alternative routes to calm the airway. Understanding how these elements interact helps clinicians pick the right therapy and empowers patients to avoid known triggers.
Finally, monitoring and lifestyle tweaks close the loop. Peak flow meters give real‑time feedback on airway calibre, letting users spot early signs of narrowing before breathlessness kicks in. Regular physical activity strengthens respiratory muscles, improving overall airflow and reducing inflammation‑related stiffness. Nutrition also matters; omega‑3 fatty acids, antioxidants from fruits and vegetables, and adequate hydration support a balanced immune response. When you combine trigger avoidance, targeted medication—whether corticosteroids, bronchodilators, or newer biologics—and consistent self‑monitoring, the cycle of inflammation can be broken or at least kept in check. Below you’ll find a curated list of articles that dives deeper into specific drugs, comparison guides, and practical tips related to airway inflammation and its many forms.
How Cystic Fibrosis and Asthma Are Linked
Explore why cystic fibrosis and asthma often appear together, how to tell them apart, and the best ways to treat both conditions safely.