Anticoagulation: What It Is, Why It Matters, and What You Need to Know
When your blood starts clotting where it shouldn’t—like in your legs, heart, or brain—that’s when anticoagulation, the medical process of preventing harmful blood clots using drugs that thin the blood. Also known as blood thinning, it’s not about making your blood watery—it’s about stopping clots before they cause strokes, heart attacks, or pulmonary embolisms. Millions of people rely on anticoagulation every day, whether they’ve had a clot before, have atrial fibrillation, or just had hip surgery. But this isn’t just popping a pill and forgetting it. Getting it right means knowing which drug you’re on, how it interacts with food and other meds, and when to call your doctor if something feels off.
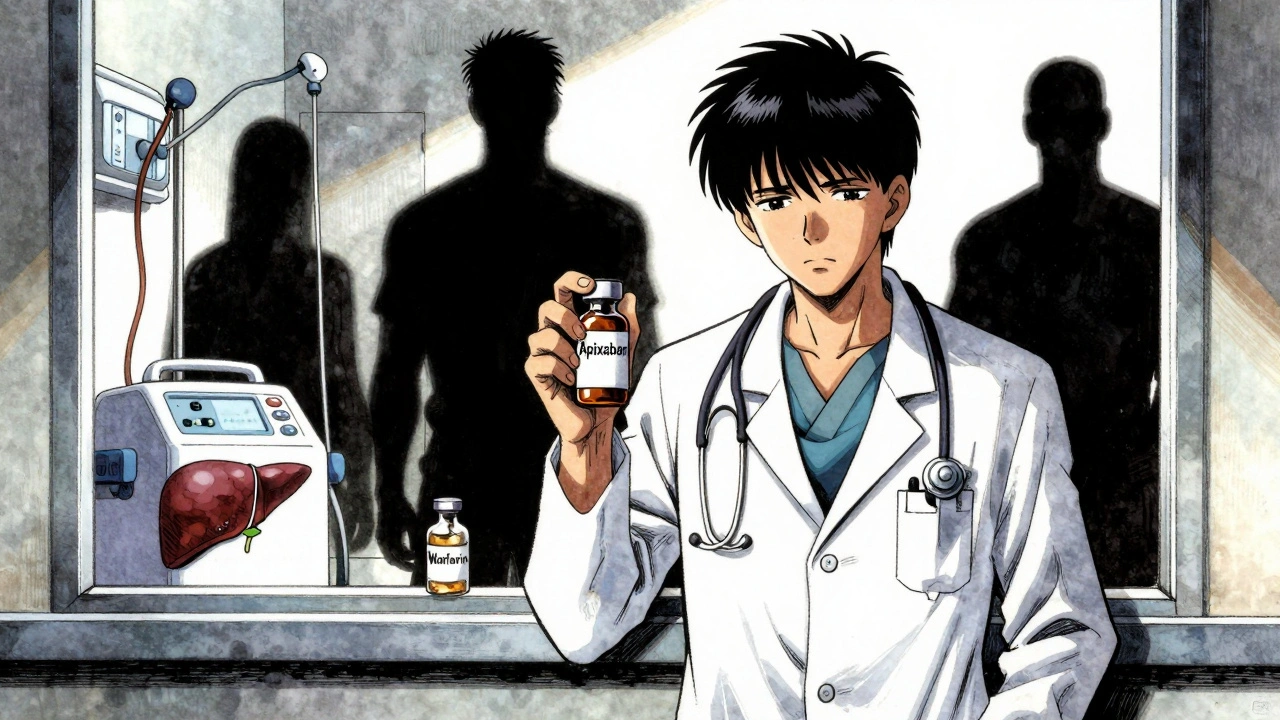
Anticoagulant drugs, medications designed to slow down the blood’s clotting process. Also known as blood thinners, it includes older options like warfarin and newer ones like apixaban or rivaroxaban. Each works differently. Warfarin needs regular blood tests and strict diet control—vitamin K in greens can mess with it. Newer drugs don’t need those tests, but they’re pricier and harder to reverse if you bleed. Then there’s clot prevention, the broader goal behind anticoagulation, whether through medication, compression devices, or movement. It’s not just about pills. Sitting still after surgery? That’s a risk. Skipping walks after a long flight? That’s a risk too. Anticoagulation doesn’t exist in a vacuum—it’s part of a bigger safety plan.
People often think if they’re on a blood thinner, they’re safe. But side effects happen. A nosebleed that won’t stop. Bruising out of nowhere. Black, tarry stools. These aren’t normal. And mixing anticoagulants with NSAIDs like ibuprofen? That’s a recipe for trouble. Even some herbal supplements—ginger, garlic, ginkgo—can make bleeding more likely. That’s why knowing your exact medication, dose, and why you’re taking it matters more than you think. The posts below cover real situations: how to talk to your doctor about switching drugs, what to do if you miss a dose, why some people can’t take certain anticoagulants, and how to handle emergencies when things go wrong. You’ll also find info on how these drugs interact with other treatments, how to store them safely, and what to do when your prescription runs out. This isn’t theory. It’s what people actually deal with every day.
Anticoagulation in Kidney and Liver Disease: What Doctors Really Do
Managing blood thinners in kidney and liver disease is complex. Apixaban may be safest in advanced kidney disease, but DOACs are risky in cirrhosis. INR is unreliable. Real-world data shows gaps in guidelines. Here's what doctors actually do.