Blood Thinners: Practical Guide to Staying Safe
A small cut can feel different when you’re on blood thinners. These medicines lower your risk of dangerous clots, but they also raise the chance of bleeding. If you or a loved one takes one, knowing how they work and what to watch for makes everyday life safer and less stressful.
Types and how they work
There are two big groups: anticoagulants and antiplatelets. Anticoagulants block the proteins that make clots. Common ones include warfarin and newer direct oral anticoagulants (DOACs) like apixaban, rivaroxaban, dabigatran, and edoxaban. Antiplatelets, like aspirin and clopidogrel, stop platelets from sticking together and are often used after stents or for heart disease.
Warfarin needs regular blood tests (INR) to stay in a safe range—usually 2.0–3.0 for many conditions. DOACs don’t require routine INR checks, but your kidney function should be checked regularly because some DOACs are cleared by the kidneys.
Everyday safety and what to watch for
Simple rules cut risk. Always tell any healthcare provider, dentist, or pharmacist you take a blood thinner. Wear an ID card or bracelet. Before starting any new medicine—even OTC pain relievers like ibuprofen—ask your doctor because NSAIDs increase bleeding risk. Avoid skipping doses; if you miss one, take it as soon as you remember unless it’s almost time for the next dose—then skip and don’t double up.
Diet matters with warfarin: foods high in vitamin K (leafy greens, broccoli) can lower its effect. Keep your vitamin K intake steady rather than avoiding those foods entirely. Alcohol can also change how these drugs work—talk to your clinician about limits.
Herbs and supplements can interact. St. John’s wort, high-dose fish oil, garlic supplements, and ginkgo may affect bleeding or drug levels. Always check with your provider before adding supplements.
Genetics can affect clot risk and treatment. For example, Factor V Leiden or prothrombin gene changes raise clotting risk and may change how long someone needs a blood thinner. If you have a family history of clots, ask about genetic testing and personalized treatment plans.
If you need surgery or a dental extraction, your doctor will give specific instructions about stopping or bridging therapy. Do not stop a blood thinner on your own.
Watch for warning signs: heavy or uncontrollable bleeding, blood in urine or stool, unusual bruising, severe headache, dizziness, or fainting. If these happen, get medical help right away. Know reversal options: vitamin K reverses warfarin; specific antidotes exist for some DOACs—discuss availability with your clinic.
Managing life on blood thinners is about small daily choices: keep communication open with providers, track tests and doses, and learn the red flags. That simple attention keeps you safer and more confident while on these important medicines.
Nosebleeds Linked to Medications: Common Causes and How to Prevent Them
Nosebleeds can be a side effect of common medications like aspirin, ibuprofen, and blood thinners. Learn why they happen, which drugs are most likely to cause them, and how to prevent them without stopping essential treatments.
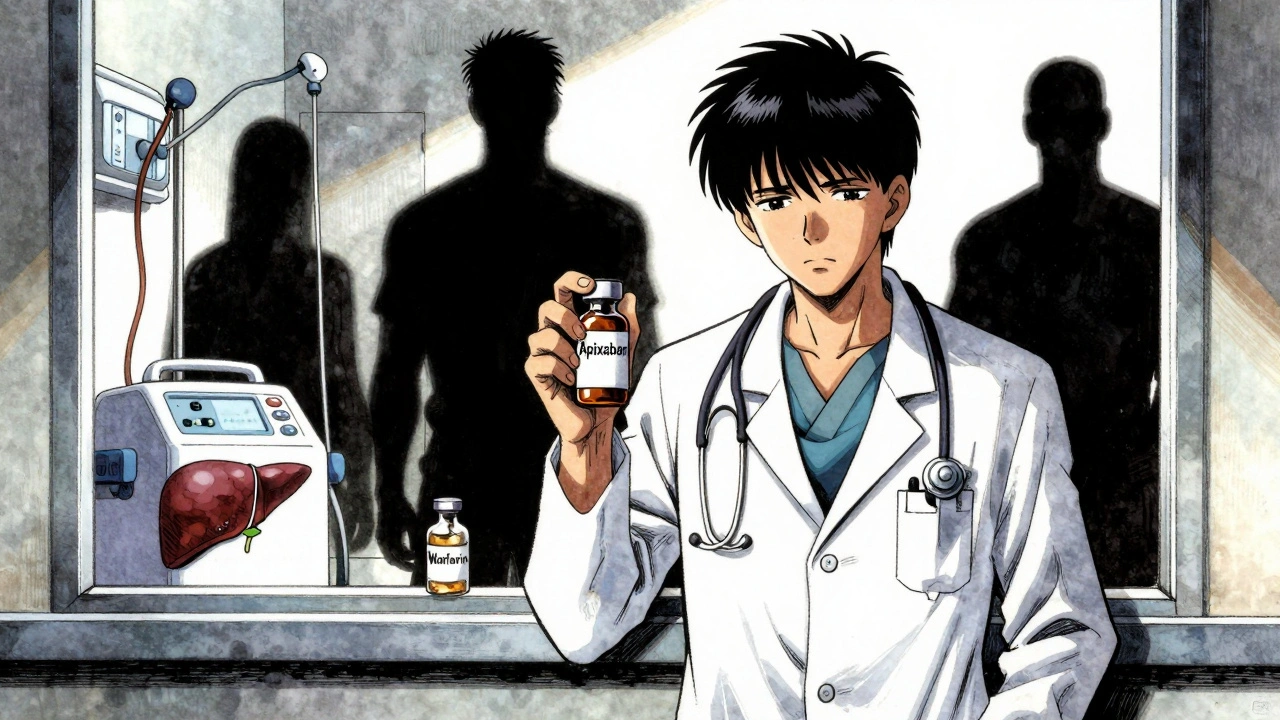
Anticoagulation in Kidney and Liver Disease: What Doctors Really Do
Managing blood thinners in kidney and liver disease is complex. Apixaban may be safest in advanced kidney disease, but DOACs are risky in cirrhosis. INR is unreliable. Real-world data shows gaps in guidelines. Here's what doctors actually do.
Blood Thinners: How They Work and When They're Needed
In my latest post, I delve into the topic of blood thinners, their function, and when they're necessary. Blood thinners work by reducing the formation of blood clots, which is crucial in preventing heart attacks and strokes. They're often prescribed for individuals with certain conditions like atrial fibrillation or deep vein thrombosis. It's important to note that while these medications can be life-saving, they must be used under close medical supervision due to potential side effects. So, if you or a loved one are prescribed blood thinners, understanding how they work is key to ensuring they're used safely and effectively.