CF and Asthma Link: Understanding Overlap and Differences
When talking about the CF and asthma link, the relationship between cystic fibrosis (CF) and asthma that often confuses patients and clinicians alike. Also known as CF‑asthma overlap, it involves shared airway inflammation, similar symptoms, and sometimes mixed treatment strategies.
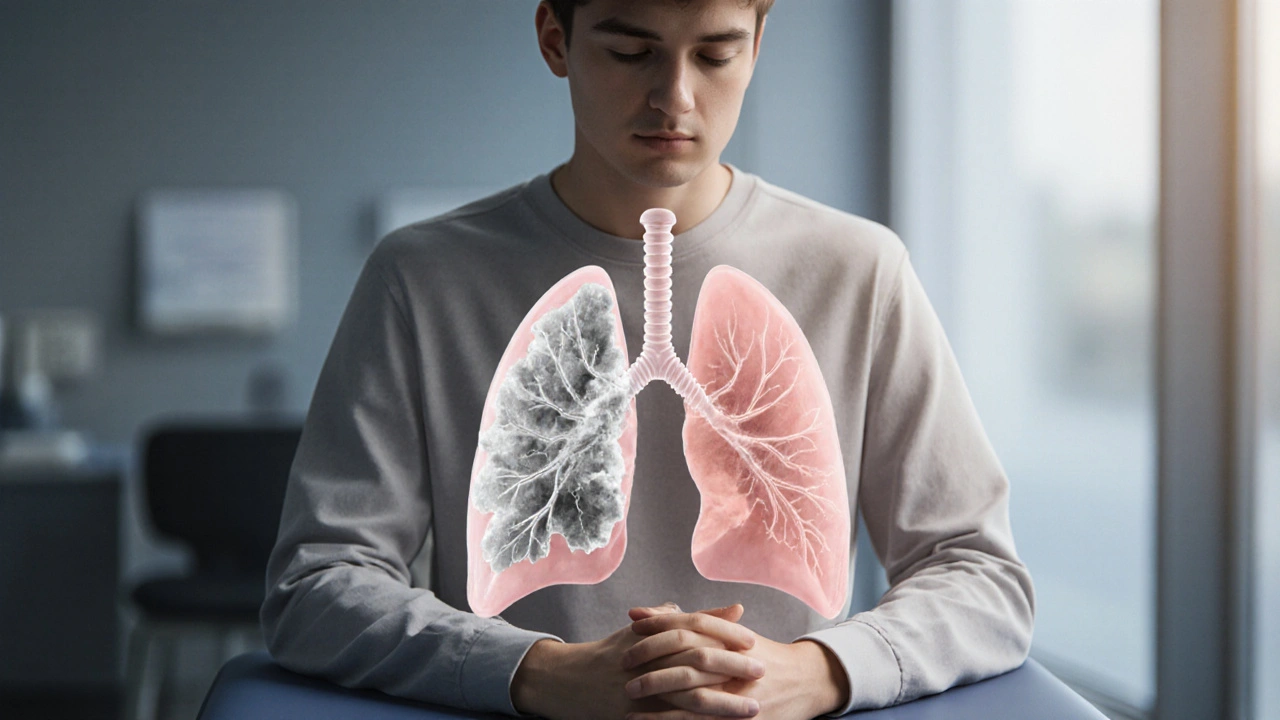
The Cystic Fibrosis, a genetic disorder caused by mutations in the CFTR gene that leads to thick mucus and chronic lung infections and Asthma, a chronic inflammatory disease characterized by reversible airway narrowing and hyper‑responsiveness each have distinct roots, but they converge on several key pathways. Both conditions trigger airway inflammation (CF and asthma link encompasses inflammation of the bronchial tree), increase mucus production, and can cause wheezing, coughing, and shortness of breath. Recognizing these commonalities helps clinicians decide when a patient might need both CF‑targeted therapy and asthma‑style bronchodilators.
Why the Overlap Matters for Patients
Understanding the CF and asthma link is not just academic; it reshapes daily care. First, symptom overlap can delay accurate diagnosis. A teenager with CF who suddenly develops episodic wheeze may be mislabelled as having worsening CF alone, missing an asthma component that would respond to inhaled corticosteroids. Second, treatment decisions hinge on this relationship. While CF therapy focuses on mucolytics, antibiotics, and CFTR modulators, asthma management adds inhaled steroids, long‑acting bronchodilators, and allergy control.
Three semantic connections illustrate the web of influence: (1) The CF and asthma link requires knowledge of genetic mutation (CFTR) and immune response (eosinophilic inflammation). (2) Airway hyper‑responsiveness influences symptom severity in both diseases. (3) Effective management depends on tailored lung function monitoring, because spirometry can reveal patterns unique to each condition.
From a practical standpoint, patients and families should track two sets of indicators. For CF, keep an eye on sweat chloride levels, pancreatic status, and chronic infection history. For asthma, monitor peak flow variability, allergen exposure, and response to rescue inhalers. When both sets show red flags, a combined approach—such as adding a low‑dose inhaled steroid to a CF regimen—can improve quality of life.
Research shows that about 10‑15% of people with CF also meet asthma diagnostic criteria, and they tend to experience more frequent exacerbations and lower lung function scores. This statistic underscores why the CF and asthma link deserves a dedicated section in any lung‑health guide. Clinicians often use a trial of bronchodilators to see if symptoms improve, a simple test that can differentiate pure CF airway obstruction from an asthma component.
Another critical piece of the puzzle is environmental triggers. Common asthma allergens—dust mites, pet dander, and pollen—can aggravate CF airways just as they do in asthma. Likewise, tobacco smoke and air pollution worsen both conditions. Patients who adopt a clean indoor environment, use HEPA filters, and avoid second‑hand smoke often see reduced wheeze episodes, illustrating the direct link between external factors and the CF‑asthma overlap.
In terms of medication interactions, the CF and asthma link can create challenges. For example, some CF patients take high‑dose ibuprofen for anti‑inflammatory effects, while asthma patients rely on leukotriene modifiers. When both are prescribed, monitoring for gastrointestinal side effects becomes essential. Likewise, newer CFTR modulators may affect the metabolism of certain inhaled corticosteroids, so pharmacy oversight is a must.
Finally, consider the psychosocial angle. Living with two chronic lung diseases can heighten anxiety and depression, especially in adolescents. Integrated care models that bring together pulmonologists, allergists, and mental‑health professionals address the full spectrum of the CF and asthma link, ensuring that treatment plans are both medically sound and emotionally supportive.
Below you’ll find a curated collection of articles that dive deeper into each aspect of this overlap—ranging from drug interaction guides to lifestyle tips and the latest research on genetic pathways. Whether you’re a patient, caregiver, or healthcare provider, the posts ahead offer concrete insights to help you navigate the complexities of the CF and asthma link.
How Cystic Fibrosis and Asthma Are Linked
Explore why cystic fibrosis and asthma often appear together, how to tell them apart, and the best ways to treat both conditions safely.