DOACs: What They Are, How They Work, and Why They Matter
When you hear DOACs, Direct Oral Anticoagulants are a class of prescription blood thinners designed to prevent dangerous clots without the need for frequent blood tests. Also known as novel oral anticoagulants, they’ve changed how millions manage conditions like atrial fibrillation and deep vein thrombosis. Unlike warfarin, which requires regular INR checks and strict diet limits, DOACs work with a fixed dose, fewer food interactions, and predictable results. That’s why doctors now prescribe them for over 70% of new anticoagulant patients.
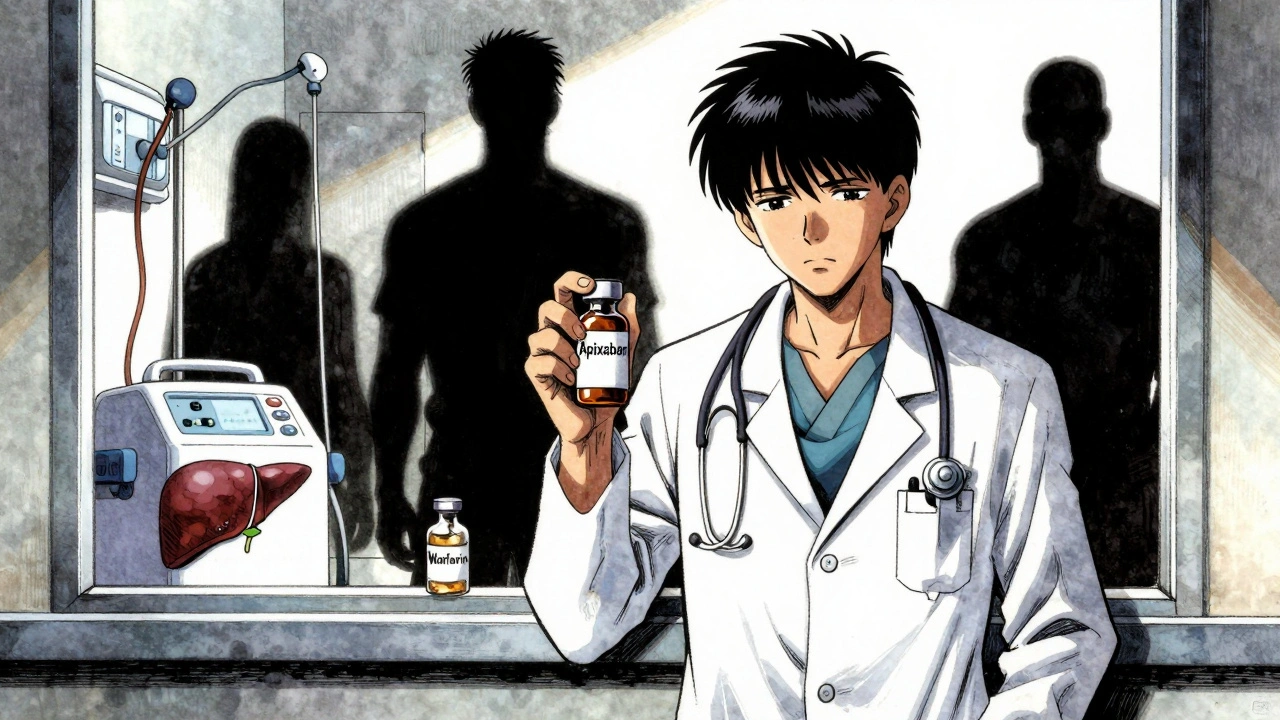
DOACs include drugs like apixaban, a common choice for stroke prevention in atrial fibrillation, known for its low bleeding risk., rivaroxaban, often used for treating blood clots in the legs or lungs., and dabigatran, one of the first in this class, effective for both prevention and treatment of clots. These drugs block specific proteins in the blood—factor Xa or thrombin—that trigger clotting. By targeting just one step, they avoid the broad effects of older drugs, reducing side effects and making them safer for long-term use.
But DOACs aren’t right for everyone. People with severe kidney disease, mechanical heart valves, or certain types of cancer may still need warfarin. And while they don’t need routine blood tests, you still need to tell every doctor you see you’re on one—especially before surgery or dental work. Stopping them suddenly can cause clots to form fast, sometimes with deadly results. That’s why understanding your exact medication, dose, and timing matters more than you might think.
What you’ll find in the posts below isn’t just a list of drug facts. It’s real-world guidance on how DOACs fit into daily life: how they interact with other meds, what to do if you miss a dose, how to handle emergencies, and why some patients still struggle to get them covered. You’ll also see how patent rules and pharmacy policies affect access, how patients communicate risks before surgery, and why even a simple pill can have complex consequences. This isn’t theory. It’s what people actually deal with when they’re on these drugs.
Anticoagulation in Kidney and Liver Disease: What Doctors Really Do
Managing blood thinners in kidney and liver disease is complex. Apixaban may be safest in advanced kidney disease, but DOACs are risky in cirrhosis. INR is unreliable. Real-world data shows gaps in guidelines. Here's what doctors actually do.