EHR Patient Notes: What Doctors Really See and How It Affects Your Care
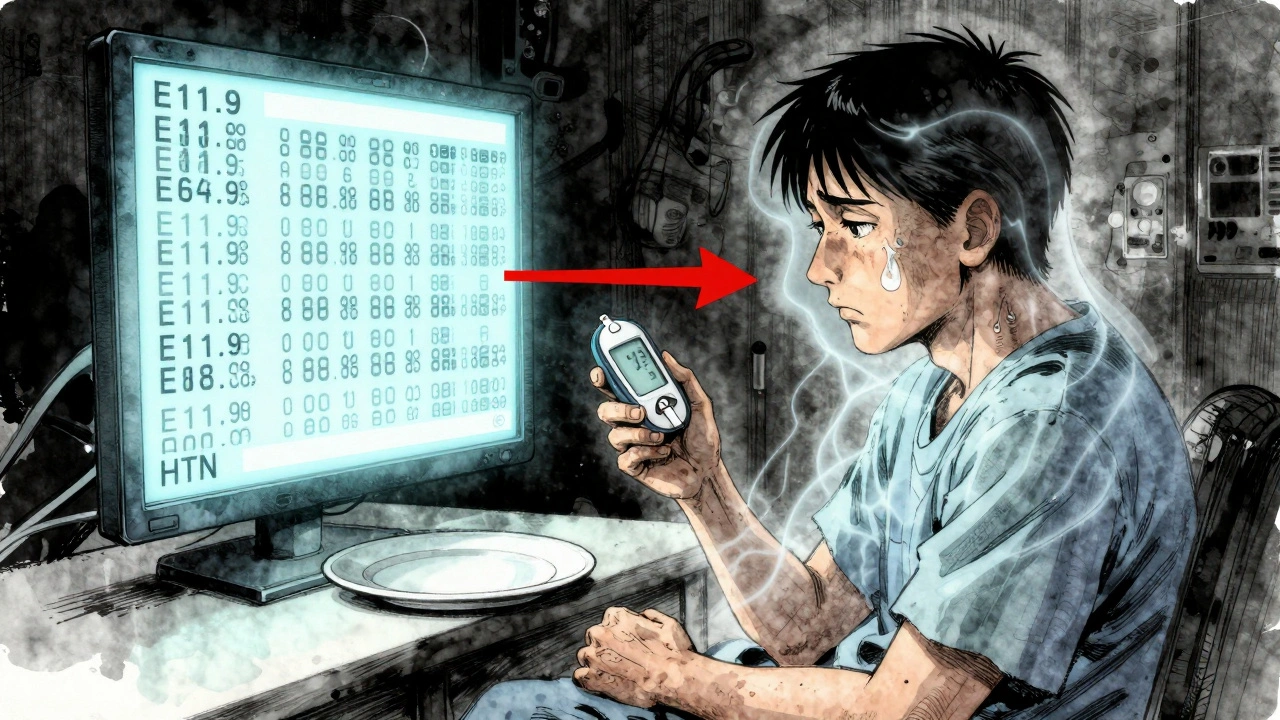
When you visit a doctor, the most important part of your visit isn’t what you say—it’s what ends up in your EHR patient notes, digital records that capture your medical history, symptoms, medications, and test results for clinical use. Also known as electronic health records, these notes are the blueprint doctors use to make decisions about your treatment, from prescribing antibiotics to ordering emergency scans. If the note is unclear, incomplete, or mislabeled, your care can be delayed, misdirected, or even dangerous.
EHR patient notes don’t just store data—they influence how medications are chosen, how allergies are flagged, and whether a drug interaction gets caught. For example, if your note says "allergic to penicillin" without specifying the reaction, a doctor might avoid all beta-lactams unnecessarily. Or if a recent lab result is buried under old notes, a kidney issue might go unnoticed until it’s critical. These aren’t hypothetical risks. Real-world studies show that over 40% of medication errors in hospitals trace back to poor documentation in EHRs. And it’s not just about missing details—it’s about how those details are organized. A note that says "patient reports fatigue" means something very different than "fatigue x 3 weeks, worsened with exertion, no chest pain, Hgb 9.2". The difference isn’t just word count—it’s whether a doctor sees anemia, heart failure, or just stress.
Doctors don’t write these notes for patients—they write them for other doctors, pharmacists, and billing systems. That’s why they’re often dense, abbreviated, and full of jargon. But that doesn’t mean you can’t understand them. You have a right to see your own EHR patient notes. In fact, reviewing them can help you catch errors before they become problems. Did your doctor note that you’re taking warfarin but forget to mention your new fish oil supplement? That could raise your bleeding risk. Did they list your allergy as "rash" when it was actually anaphylaxis? That’s a life-or-death mismatch.
And it’s not just about what’s in the note—it’s about what’s left out. Many EHR systems force doctors into templates that don’t fit real cases. A patient with complex chronic pain might end up with a note that says "follow-up for pain"—with no detail on what meds were tried, what side effects occurred, or how the pain affects sleep or work. That’s why some doctors still use handwritten addendums or voice notes to fill the gaps. These workarounds are signs of a system struggling to keep up with real patient needs.
What you’ll find in the posts below are real examples of how EHR patient notes impact care—from how generic drug switches get flagged in systems, to why black box warnings get missed in cluttered records, to how military families using TRICARE rely on clean documentation to get their prescriptions approved. You’ll see how expired medication disposal guidelines get recorded (or ignored), how drug reactions are documented before surgery, and why complex generics sometimes get stuck because the EHR doesn’t recognize the combination. These aren’t abstract tech issues—they’re the quiet, daily moments where your health hangs in the balance of a few typed lines.
Patient Information vs Healthcare Provider Information: How Label Differences Affect Care
Patient and provider labels often don’t match-leading to confusion, errors, and missed care. Learn how medical jargon creates gaps in understanding and what’s being done to fix it.