Generic Drug History: How Cheaper Medicines Changed Healthcare
When you pick up a prescription and see generic drug history, the story of how identical, lower-cost versions of brand-name medicines became mainstream. Also known as generic medications, they’re not just cheaper—they’re the reason millions can afford life-saving treatments today. Before the 1980s, if you needed a drug like ibuprofen or amoxicillin, you paid whatever the brand made you pay. No alternatives. No competition. Then came the Hatch-Waxman Act of 1984, a quiet law that changed everything. It let companies make exact copies of expired brand-name drugs without repeating expensive clinical trials. The FDA didn’t need to prove they worked again—just that they matched the original in strength, safety, and how the body absorbed them.
This wasn’t magic. It was logic. The brand-name drugs, medications developed and marketed by pharmaceutical companies under patent protection. Also known as originator drugs, it took years and hundreds of millions to bring a new drug to market. Clinical trials, marketing, patents—all added cost. Once the patent expired, generics stepped in. The FDA approval, the process that ensures generic drugs meet the same strict standards as brand-name versions. Also known as ANDA approval, it became the gatekeeper. No shortcuts. No exceptions. A generic pill had to dissolve the same way, release the same amount of active ingredient, and perform the same in your body. That’s why your doctor can confidently switch you from Lipitor to atorvastatin, or from Claritin to loratadine.
And it worked. By 2023, over 90% of prescriptions filled in the U.S. were generics. That’s not just a number—it’s a family keeping their insulin, their blood pressure meds, their antidepressants. It’s an elderly person choosing between groceries and a pill. The drug affordability, the ability to access necessary medications without financial hardship. Also known as medication cost savings, it didn’t happen by accident. It happened because the system was designed to let competition drive prices down. You don’t need to be a scientist to understand this: if two pills are chemically identical, why pay three times more for the one with the fancy logo?
Some people still worry. They think generics are "weaker" or "made in a different factory"—which is true, but irrelevant. The same factories often make both brand and generic versions. The same quality controls apply. The same inspectors show up unannounced. What’s changed isn’t the pill. It’s the perception. Advertising still pushes brand names. Doctors still get free samples. But the data doesn’t lie: patients on generics have the same outcomes, same side effects, same success rates. The generic drug history isn’t about cutting corners. It’s about cutting waste. It’s about making medicine work for everyone, not just those who can afford the markup.
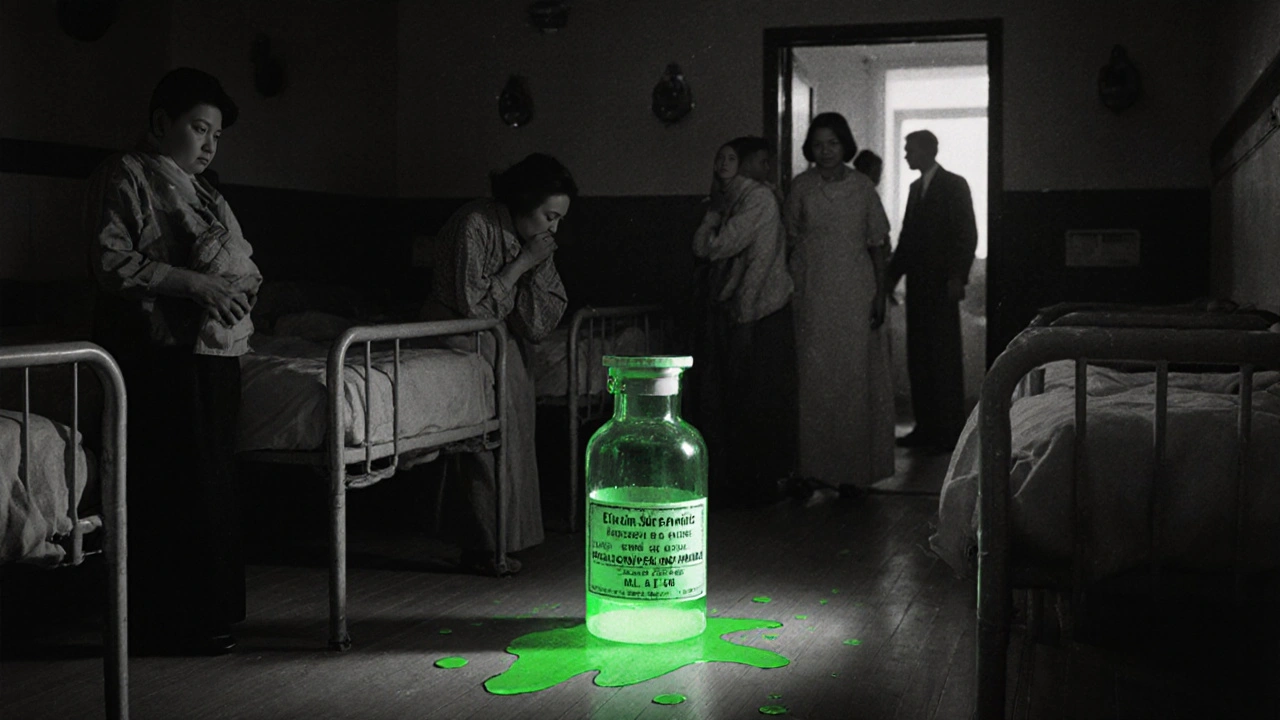
Below, you’ll find real stories and facts about how generics save money, how they’re made, why some combinations still lag behind, and how marketing tricks still fool people into paying more. These aren’t theory pieces. They’re grounded in what’s happening now—in pharmacies, in clinics, in people’s wallets. You’re not just reading about history. You’re seeing how it still shapes your health today.
History of Generic Drugs in the United States: How Cheaper Medicines Took Over
Generic drugs now make up over 90% of U.S. prescriptions, saving trillions. Learn how the Hatch-Waxman Act, FDA regulations, and global supply chains shaped today’s affordable medicine system.