Geriatric Prescribing: Safe Medication Use for Older Adults
When we talk about geriatric prescribing, the practice of selecting and adjusting medications for older adults based on their changing physiology and health needs. Also known as prescribing for the elderly, it's not just about giving pills—it's about understanding how aging changes the way the body handles drugs. As we get older, our kidneys and liver don't filter medications the same way. Blood flow slows down, body fat increases, and muscle mass drops. That means a dose that was safe at 50 might be too strong at 75. Many seniors take five or more meds at once—a situation called polypharmacy, the use of multiple medications by a patient, often leading to increased risk of side effects and interactions. This isn’t just a numbers game. It’s about balance. A pill that helps with arthritis might make dementia worse. A blood pressure med that lowers pressure too much can cause falls. And many common drugs, like antihistamines or muscle relaxants, are actually risky for seniors but still get prescribed because doctors aren’t always trained to spot the danger.
That’s where drug interactions in aging, the way medications behave differently when taken together by older adults, often leading to unexpected side effects. becomes critical. Take a senior on warfarin for blood thinning who also starts taking an antibiotic. That combo can spike bleeding risk. Or someone on a statin for cholesterol who adds a muscle relaxant—suddenly, they’re at risk for rhabdomyolysis, a dangerous muscle breakdown. Even over-the-counter stuff like ibuprofen or sleep aids can cause trouble. Seniors often don’t realize these aren’t harmless. And sometimes, doctors don’t either. The real problem isn’t the drugs themselves—it’s the lack of personalized review. Many prescriptions just keep getting refilled year after year, even when the original reason is gone.
What you’ll find in this collection isn’t theory. It’s real-world examples of how medications behave differently in older bodies. You’ll see how drugs like nitrofurantoin can harm the liver in seniors, why certain statins cause more muscle pain in the elderly, and how stopping a seizure med like carbamazepine without tapering can trigger dangerous withdrawal. You’ll learn why expired pills might still work—but not for everyone—and how to spot when a drug is doing more harm than good. There’s no one-size-fits-all fix in geriatric prescribing. It’s about asking the right questions: Is this still needed? Could this be replaced? What’s the real risk here? These posts give you the facts to make those calls—whether you’re a patient, a caregiver, or a clinician trying to do better.
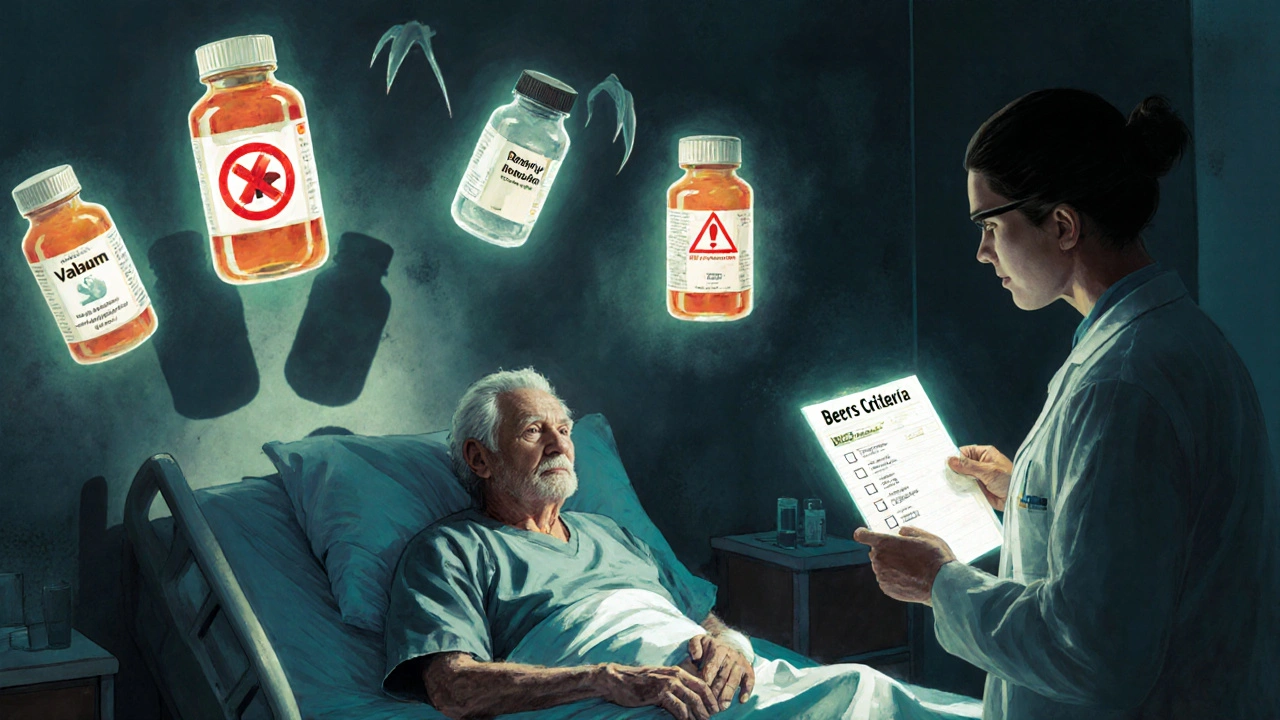
Beers Criteria: Potentially Inappropriate Drugs in Older Adults Explained
The Beers Criteria identify potentially dangerous drugs for adults over 65. Learn which medications to avoid, why they're risky, and how to talk to your doctor about safer options.