Healthcare Provider Labels: What They Mean and Why They Matter
When you pick up a prescription, the small sticker on the bottle isn’t just paperwork—it’s your healthcare provider labels, official instructions from your doctor or pharmacist that tell you how, when, and why to take your medicine. Also known as prescription labels, these are the last line of defense against medication errors, and they carry legally required details that can save your life. These labels aren’t just about dosage—they include warnings, storage rules, refill info, and sometimes even why the drug was prescribed. If you ignore them, you’re guessing. And guessing with meds is dangerous.
Behind every label is a system built on FDA labeling requirements, federal rules that force drugmakers and pharmacies to include critical safety info. For example, black box warnings—like those on blood thinners or seizure meds—must appear in bold, upfront text. But not all labels are created equal. Some are cluttered. Others skip key details. And when pharmacies switch generic brands, the label might change even though the drug doesn’t. That’s why you need to read every line, not just the name and dose. A label for a medication safety, the practice of preventing harm from drugs through clear communication and proper use system also includes things like "Take with food" or "Avoid alcohol," which aren’t suggestions—they’re science-backed rules. Skip them, and you risk liver damage, dangerous interactions, or even death.
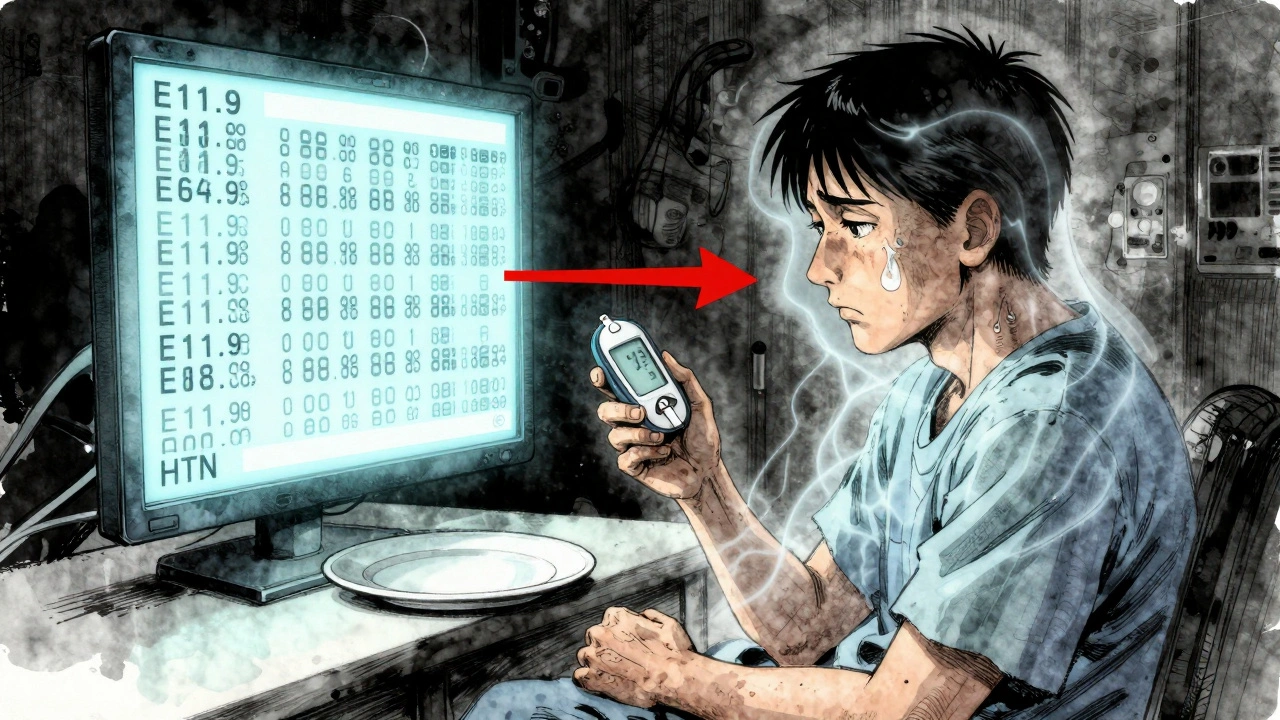
Here’s the thing: most people don’t realize how much is hidden in those tiny fonts. A label for an inhaler might say "use as needed," but if you’re using it 5 times a day, you’re likely mismanaging your asthma. A label for a generic version of a drug might look different from the brand, even though it’s identical—yet many patients assume the change means it’s weaker. That’s not true, but it’s a myth fueled by poor labeling clarity. And when you’re on multiple meds—like a blood thinner, a kidney drug, and a painkiller—the risk of conflicting instructions skyrockets. That’s why drug labeling, the standardized way information is presented on prescriptions and packaging needs to be clear, consistent, and patient-centered. Too often, it’s not.
What you’ll find in the articles below is real-world insight into how these labels work—or fail to work—in practice. You’ll see how patent delays affect generic labels, why some drugs have confusing warnings, how military families navigate TRICARE’s labeling rules, and why expired EpiPens still have active ingredients years past their printed date. You’ll learn how to spot when a label is hiding a risk, how to ask your pharmacist for clarification, and what to do when the label contradicts your doctor’s advice. This isn’t theory. It’s what happens when people actually use their meds—and what goes wrong when the system lets them down.
Patient Information vs Healthcare Provider Information: How Label Differences Affect Care
Patient and provider labels often don’t match-leading to confusion, errors, and missed care. Learn how medical jargon creates gaps in understanding and what’s being done to fix it.