ICD-10 vs Patient Language: Bridging Medical Codes and Real-World Understanding
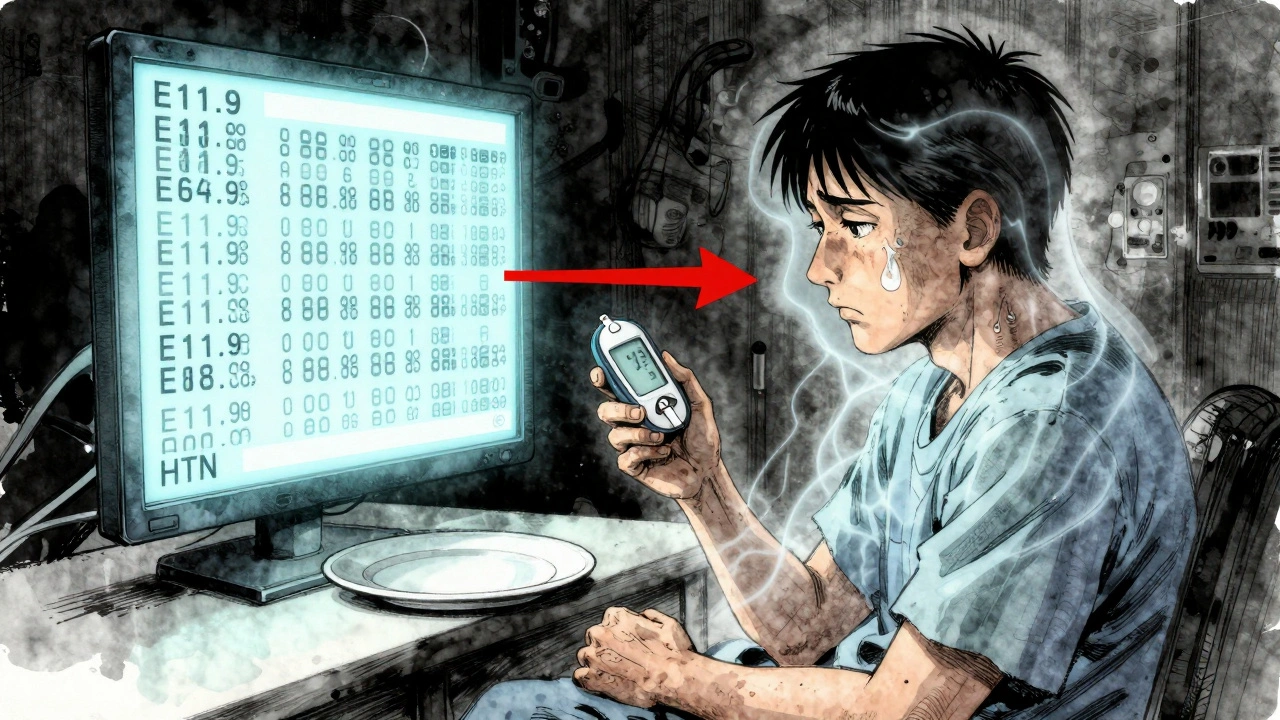
When your doctor says you have ICD-10, a standardized system of diagnostic codes used by healthcare providers for billing and tracking diseases. Also known as International Classification of Diseases, 10th Revision, it helps hospitals, insurers, and government agencies organize health data. But if you walk out of the office hearing only "E11.9" or "J44.1," you’re left with a string of numbers—not an answer. ICD-10 was never meant to explain your condition to you. It was built for paperwork, not understanding.
That’s where patient language, the plain, everyday words people use to describe their symptoms and health experiences comes in. You don’t say "hypertension"—you say "my blood pressure’s been high." You don’t say "G47.33"—you say "I can’t sleep through the night." The gap between these two systems isn’t just technical—it’s personal. When doctors skip translating ICD-10 into patient language, people get confused, anxious, or worse, stop trusting their care. Studies show patients who understand their diagnosis in plain terms are more likely to follow treatment plans, take meds correctly, and notice warning signs early. That’s why the best doctors don’t just code your illness—they explain it.
This gap shows up everywhere in real care. A patient with chronic obstructive pulmonary disease, a lung condition often coded as J44.9 might hear "COPD" and think it’s just smoking-related. But if the doctor says, "Your lungs are stiff and can’t push air out well," suddenly it clicks. Same with kidney disease, coded as N18.9, but often described by patients as "my kidneys aren’t filtering right". The code tells the system what to bill. The explanation tells the patient what to do. And when you’re managing meds like blood thinners, inhalers, or antihistamines—like in our posts on DOACs, EpiPens, or Clarinex—you need to know why you’re taking them, not just what the code says.
Some doctors still treat ICD-10 like a secret code. But the best ones use it as a starting point—not the ending. They pair the code with a story: "This is what’s happening in your body, here’s how it feels, and here’s what we do next." That’s the kind of clarity that turns confusion into control. In the posts below, you’ll find real examples of how patients and providers navigate this divide—from explaining black box warnings to helping military families understand TRICARE coverage, or teaching people how to talk about drug reactions before surgery. These aren’t just medical guides. They’re translations.
Patient Information vs Healthcare Provider Information: How Label Differences Affect Care
Patient and provider labels often don’t match-leading to confusion, errors, and missed care. Learn how medical jargon creates gaps in understanding and what’s being done to fix it.