Kidney Disease: Causes, Symptoms, and How Medications Affect Your Kidneys
When your kidney disease, a condition where the kidneys lose their ability to filter waste and excess fluid from the blood. Also known as chronic kidney disease, it often develops slowly and without clear warning signs until damage is advanced. Your kidneys work 24/7 to clean your blood, balance electrolytes, and help control blood pressure. When they start failing, toxins build up, fluid swells in your legs, and your body struggles to make red blood cells. Many people don’t realize they have it until a routine blood test shows high creatinine or low eGFR—numbers that tell doctors how well your kidneys are actually working.
What causes kidney disease? The top two culprits are high blood pressure, a condition that forces blood through vessels at too much pressure, damaging delicate kidney filters over time and diabetes, a metabolic disorder that floods the bloodstream with sugar, which slowly scars kidney tissue. But meds play a big role too. Common painkillers like ibuprofen or naproxen, certain antibiotics, and even some blood pressure drugs can harm your kidneys if used long-term or if you already have reduced function. Even over-the-counter supplements and herbal remedies aren’t always safe—some contain heavy metals or compounds that stress the kidneys. If you’re on multiple medications, especially with other health issues, your kidneys are working harder than you think.
Symptoms don’t always show up early. When they do, you might notice swelling in your ankles, fatigue, trouble sleeping, or changes in how often you urinate—too much, too little, or foamy urine. Some people feel nauseous or have persistent itching. These aren’t just "getting older" signs. They’re your body asking for help. The good news? Catching kidney disease early gives you time to slow it down. Diet changes, blood pressure control, avoiding certain drugs, and regular monitoring can keep you off dialysis for years—or even prevent it entirely.
The posts below cover real issues people face: how certain drugs like nitrofurantoin can be risky if you have kidney problems, what to do when swelling shows up from meds, how to safely dispose of kidney-related treatments, and how generic versions of essential drugs can help manage costs without cutting corners. You’ll find practical advice on communicating with doctors about your kidney health before surgery, understanding black box warnings on kidney-toxic meds, and what to ask when your prescription list keeps growing. This isn’t theoretical—it’s what people are dealing with right now, and what you need to know to protect your kidneys before it’s too late.
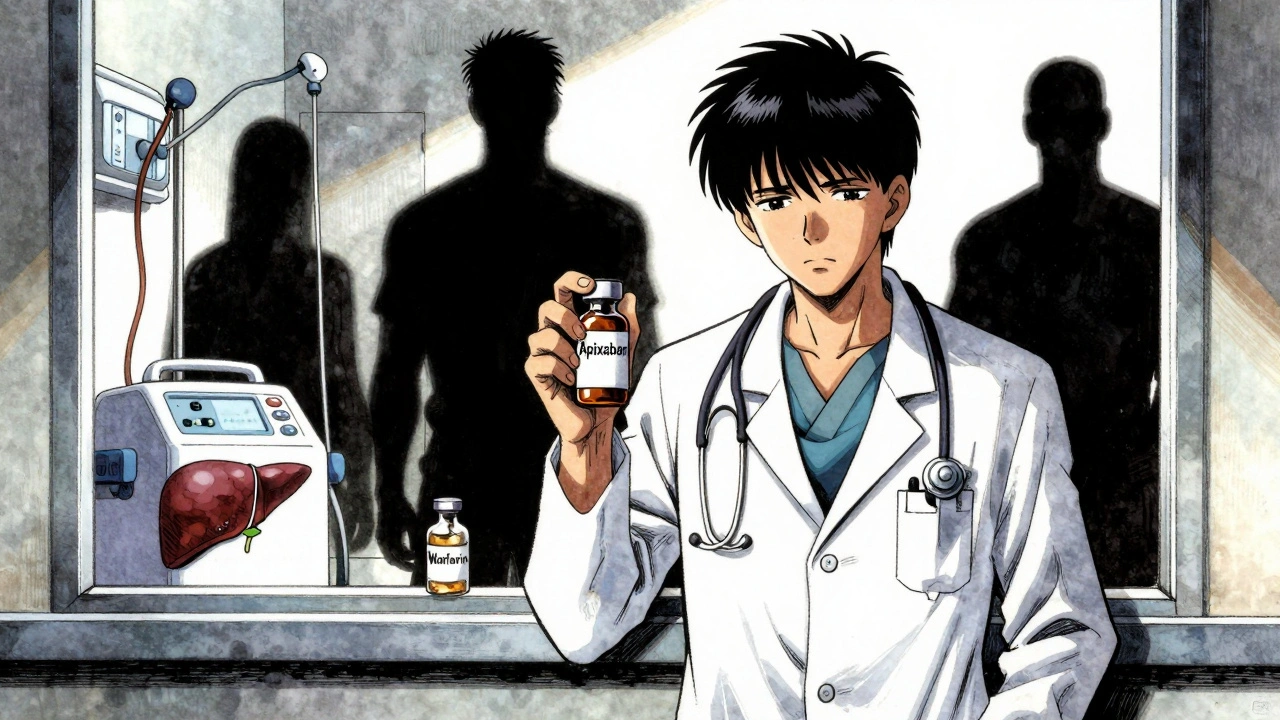
Anticoagulation in Kidney and Liver Disease: What Doctors Really Do
Managing blood thinners in kidney and liver disease is complex. Apixaban may be safest in advanced kidney disease, but DOACs are risky in cirrhosis. INR is unreliable. Real-world data shows gaps in guidelines. Here's what doctors actually do.