Myosis causes: why your pupils are tiny and what to do
Tiny pupils can mean different things — from a harmless medication effect to a serious brain or nerve problem. "Myosis" (often spelled miosis) is the medical word for abnormally small pupils. This page explains the common causes, how doctors evaluate tiny pupils, and what you should do next.
Common, easy-to-spot causes
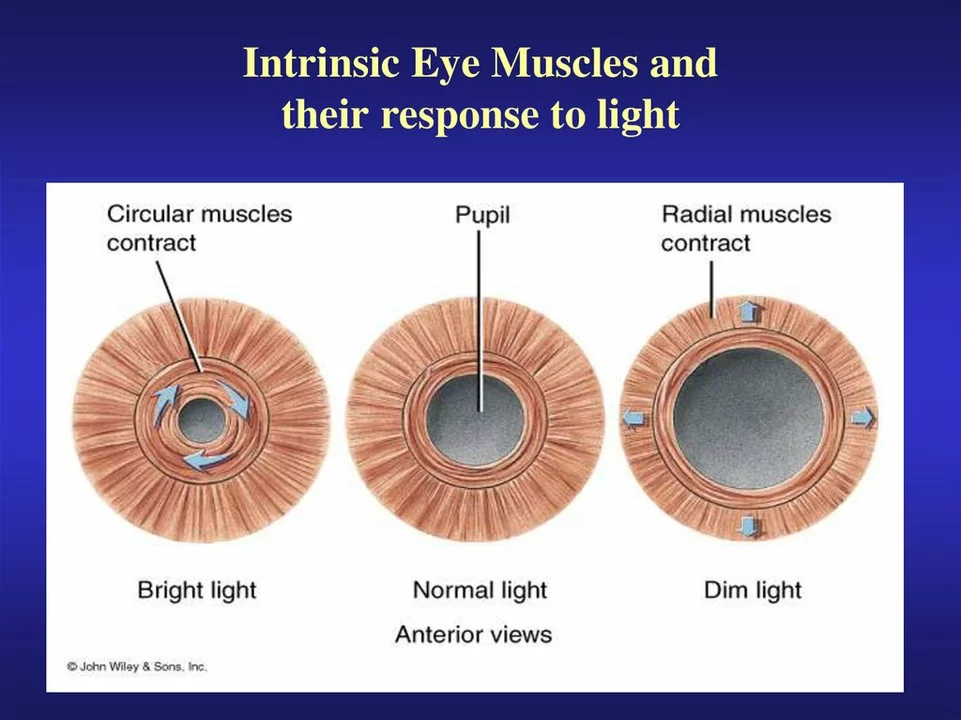
Most of the time, small pupils come from drugs or eye drops. Opioids (like morphine, heroin, oxycodone) cause classic pinpoint pupils. Eye medicines that treat glaucoma — pilocarpine, for example — make pupils small. Some blood pressure medicines (clonidine) and certain anti-anxiety drugs can also shrink pupils. Even bright light will make pupils smaller, so always check in normal room lighting.
Less obvious but important: organophosphate poisoning (found in some insecticides) causes strong, sustained miosis. In that case you might see other signs too — sweating, drooling, muscle twitching — and that’s an emergency.
When tiny pupils point to nerve or brain problems
Small pupils can come from nerve damage. Horner syndrome is a classic cause — one small pupil plus a droopy eyelid and lack of sweating on one side of the face. That can come from a neck or chest tumor, a stroke, or a carotid artery problem.
A rare but urgent cause is a brainstem lesion (for example, a bleeding stroke in the pons). With that you’ll usually see other signs: trouble walking, double vision, weakness, or decreased consciousness. If tiny pupils come with sudden severe headache, vomiting, numbness, or confusion, get emergency care.
Another possibility is a 3rd cranial nerve palsy — usually that makes the pupil large, but in some patterns it can affect pupil size. Your eye doctor or neurologist will sort this out.
How doctors check and diagnose myosis
First they take a history: recent meds, drugs, eye drops, exposure to chemicals, or trauma. Then a simple exam checks how pupils react to light and to focusing on a near object. If Horner syndrome is suspected, doctors may use drops (apraclonidine or cocaine drops) to test the nerve pathway. Blood or urine tests can find opioids or toxins. If a nerve or brain cause is possible, imaging (MRI/CT) follows.
Treatment depends on the cause. If it’s opioids and the person is unresponsive or breathing slowly, naloxone (Narcan) is life-saving. For organophosphate poisoning, atropine and pralidoxime in hospital are needed. If an eye drug caused it, stopping the drop usually fixes the pupil. Horner syndrome needs workup for the underlying problem — sometimes that finds a treatable tumor or vascular issue.
What should you do? If tiny pupils are the only thing, and you know the person took a medication that causes miosis, monitor and contact their doctor. If there’s altered breathing, loss of consciousness, severe headache, weakness, or signs of poisoning — call emergency services now.
Need help deciding? Take a quick photo of the eyes in normal light and note any other symptoms. Share meds, timing, and any drug use with the clinician — that saves time and gets the right care faster.
Pupil Constriction: What Causes Myosis?
As a blogger, I recently explored the topic of pupil constriction, or myosis, and discovered some interesting facts. Myosis occurs when the muscles in our iris contract, causing the pupil to become smaller. There are several factors that can lead to this reaction, such as exposure to bright light, certain medications, and even the natural aging process. Additionally, some underlying health conditions, like brain injuries or eye trauma, can also cause pupil constriction. It's essential to be aware of these factors and consult a healthcare professional if you experience any sudden or unexplained changes in your pupils.