Neuroblastoma treatment: clear options and what families should know
Neuroblastoma is a childhood cancer that starts in nerve cells. Treatment depends on the child’s age, where the tumor is, and specific biology like MYCN amplification or ALK mutations. That means two kids with the same tumor can get very different plans. Here’s a straightforward look at common treatments, how they work, side effects to expect, and practical steps you can take right away.
Main treatment options
Surgery: If the tumor is localized, surgeons often remove as much as possible. Surgery can cure many low-risk cases and may be the only treatment needed. Recovery is usually quick, but ask the surgeon about nerve, bowel, or organ risks tied to the tumor location.
Chemotherapy: Chemo shrinks tumors and treats disease that may have spread. It’s the backbone for intermediate and high-risk patients. Expect low blood counts, infection risk, nausea, and hair loss. Modern anti-nausea meds and growth factors help a lot.
Radiation: Used for local control when surgery can’t remove everything or when disease remains. Side effects depend on the area treated — skin irritation, fatigue, and, in growing children, possible effects on bone or organ growth. Ask about shielding and long-term monitoring.
High-dose therapy with stem cell transplant: For high-risk neuroblastoma, doctors often use intensive chemo followed by the child’s own stem cells to recover blood counts. This is tough short-term — long hospital stays, infection risk — but can improve long-term control.
Immunotherapy and maintenance: Anti-GD2 antibodies (like dinutuximab) given after transplant reduce relapse risk. These drugs can cause significant neuropathic pain during infusion; hospitals use pain protocols. A retinoid (isotretinoin) often follows to help cancer cells mature and die.
Targeted therapy: If testing shows an ALK mutation, ALK inhibitors (for example, crizotinib) may help. Tumor genetics matter — request molecular testing so targeted options or clinical trials can be considered.
Practical steps for families
Ask for a complete biology report: MYCN status, ALK mutations, and other markers change treatment and trial eligibility. If you get a high-risk diagnosis, seek care at a pediatric cancer center with experience in neuroblastoma.
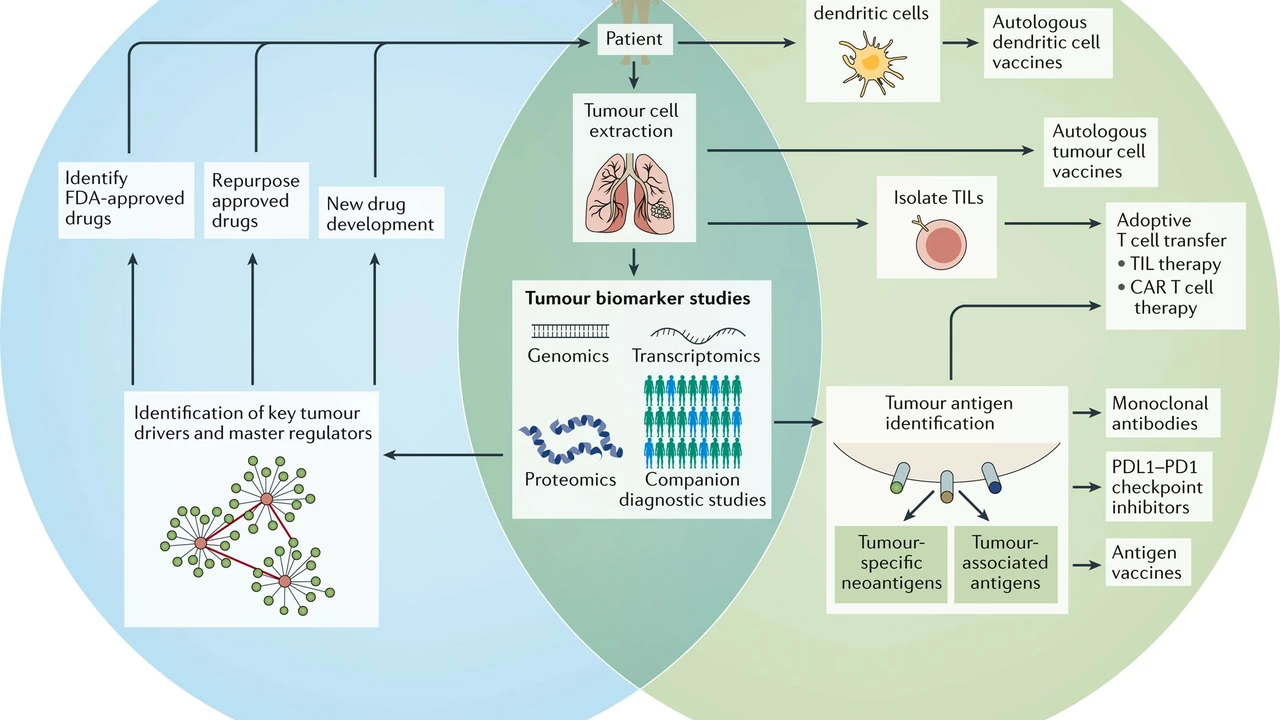
Talk about clinical trials early. Many advances — CAR-T, new targeted drugs, vaccine approaches — are available through trials and may fit your child.
Plan for side effects and long-term issues: hearing loss from some chemo, growth and hormonal changes, and fertility risks are real. Ask about baseline hearing tests, fertility preservation, and follow-up clinics for survivors.
Get a second opinion if you’re unsure. Bring scans, pathology reports, and the tumor biology results. A second team can confirm the plan or point you to options you didn’t hear about.
Support matters. Social workers, pain teams, nutritionists, and rehab therapists make treatment more tolerable and speed recovery. Don’t hesitate to ask the team for these resources.
Neuroblastoma treatment is complex but increasingly precise. Focus on tumor biology, expert centers, and clear questions for the team — that will help you make the best choices for your child.
The Role of Personalized Medicine in Neuroblastoma Treatment
In my recent research, I've delved into the role of personalized medicine in treating neuroblastoma, a type of cancer that mostly affects children. Personalized medicine tailors treatment based on the genetic makeup of the cancer, offering a more effective approach. This targeted therapy means that the treatment can specifically attack cancer cells, reducing harm to healthy cells and potentially leading to better outcomes. The hope is that personalized medicine will not only increase survival rates but also reduce the long-term side effects often experienced by survivors. It's a promising field that could revolutionize how we treat neuroblastoma and other cancers.