Patient Information: What You Need to Know About Medications, Safety, and Your Rights
When it comes to your health, patient information, the practical knowledge you need to use medications safely and make informed choices. Also known as medication literacy, it’s not about memorizing drug names—it’s about understanding what’s in your pill bottle, why it matters, and how to act when something doesn’t feel right. Too many people take pills every day without knowing the risks, the alternatives, or even how to ask the right questions. That’s where real patient information changes everything.
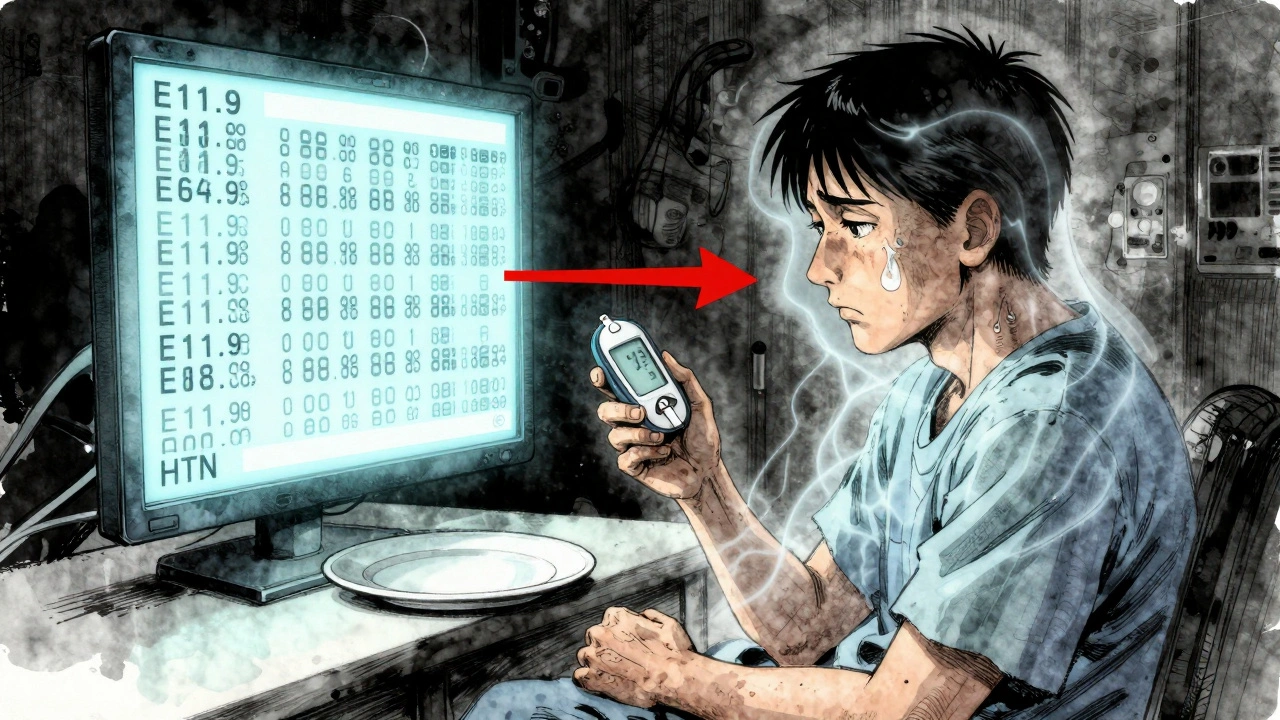
Think about generic drugs, the same active ingredients as brand-name drugs but often 80% cheaper. Also known as generic medications, they’re used in over 90% of U.S. prescriptions, yet many still believe they’re weaker or less safe. That’s not true. The FDA requires them to work the same way. But here’s the catch: some drugs—like seizure meds or blood thinners—need extra care when switching. Medical societies warn against automatic substitutions for these, and your doctor should explain why. Patient information means knowing when generics are perfect, and when they need a closer look. Then there’s drug side effects, the unexpected reactions that can range from mild to life-threatening. Also known as adverse drug reactions, they’re not always listed clearly. Swelling in your hands? A cough that won’t quit? These might not be random—they could be tied to a medication you’ve been taking for months. Patient information helps you connect the dots before it’s too late. And don’t forget medication safety, the daily habits that keep you out of the emergency room. Also known as drug safety practices, it’s about storing pills properly, knowing what to do with expired EpiPens or inhalers, and having a go-bag ready for disasters. It’s also about telling your doctor every drug you’ve ever reacted to—before surgery. One missed detail can cost you your life.
Real patient information isn’t found in brochures you never read. It’s in knowing that expiration dates aren’t hard deadlines, that some pills are still good years later if kept dry and cool. It’s understanding that black box warnings aren’t scare tactics—they’re red flags you should never ignore. It’s realizing that prescription assistance programs exist, and you might qualify even if you have Medicare. It’s knowing that advertising makes brand-name drugs look better, even when the generic does the exact same job. And it’s recognizing that your voice matters—whether you’re asking your pharmacist why your new pill looks different, or pushing back when a doctor dismisses your symptoms.
Below, you’ll find real stories from people who’ve been there—how to dispose of patches safely, how to handle allergic reactions before surgery, why some generics take years to reach shelves, and how to spot liver damage from a common antibiotic. These aren’t theory pieces. They’re what doctors, pharmacists, and patients actually deal with. Use this as your guide to take control—not just of your meds, but of your health.
Patient Information vs Healthcare Provider Information: How Label Differences Affect Care
Patient and provider labels often don’t match-leading to confusion, errors, and missed care. Learn how medical jargon creates gaps in understanding and what’s being done to fix it.